Pyramidal or pyramidal insufficiency syndrome is a violation of the tone of the muscles of the extremities, especially the lower ones. This pathology is also called “toe walking” or “ballerina symptom.” Often accompanied by equinus or equinovarus foot placement (the feet seem to move apart in different directions, and the ankle “falls” inward). This condition is often diagnosed in children in the first year of life (before the child learns to walk), less often in two or three year old children. Like the consequences of meningitis, head injury and other lesions of the nervous system, they can develop in adulthood.
Why does pyramidal insufficiency syndrome occur?
The medulla oblongata, whose cells are called “pyramids,” is responsible for complex reflexes in the human body. It is as a result of any disturbances in this part of the brain that the so-called pyramidal insufficiency occurs, i.e., disturbances in the adequacy of reflexes. The most common causes of deficiency are:
- congenital pathologies of the NS,
- birth injuries,
- fetal hypoxia during pregnancy or childbirth,
- disruption of the production or outflow of cerebrospinal fluid (cerebrospinal fluid),
- infectious diseases,
- abscesses,
- inflammation of the meninges that cause hydrocephalus (meningitis, encephalitis),
- tumors
- cerebral hemorrhages.
Pyramidal insufficiency syndrome is by and large not a separate disease. This is a secondary condition caused by an underlying disease of the nervous system. It is worth noting that in infancy (2-3 months), tightening of the legs and hypertonicity of the lower leg muscles is not a terrible pathology. As the nervous system ages and matures, this condition usually goes away.
How are children with this diagnosis treated?
Basically, for children diagnosed with pyramidal insufficiency, the doctor prescribes various physiotherapy procedures. You may also need orthopedic means, with the help of which parts of the body are given a physiological position, and balneotherapy (health baths).
To reduce muscle tone and strengthen muscles, doctors recommend acupressure and relaxation massage, a course of which is taken every 6 months.
Every day, parents should do special health-improving and preventive exercises with their child.
If necessary, doctors can prescribe vitamins, vasoactive agents (for microcirculation) and drugs that improve the process of metabolic breakdown.
Surgeries are resorted to only when the doctor has diagnosed:
- brain or spinal cord injuries/tumors;
- acute cerebrovascular accidents that cannot be cured by chemical, physical and biological means (for example, thrombosis or intracerebral hematoma).
Symptoms of pyramidal insufficiency in children
Pyramidal insufficiency in children manifests itself in
- weak grasp reflex in infancy and difficulties with holding objects at an older age,
- tremors of the arms, legs or chin,
- throwing your head back,
- walking only on toes without support on the heel,
- in a standing position - tuck your toes.
Making such a diagnosis is often unjustified, and it only means hypertonicity of the calf muscles without any other symptoms. We can talk about real insufficiency only when the child can already walk freely, but at the same time steps only on his toes, plus he has other symptoms of dysfunction of the nervous system. However, if you find any of the listed symptoms in your child, consult a pediatric neurologist, because simple hypertension sometimes hides serious illnesses that can lead to delayed physical (or even mental) development.
What is pyramidal deficiency?
There are clear criteria that characterize pyramidal deficiency. This is a description of paralysis or paresis (partial paralysis). Here they are:
- decreased strength (for example, with bilateral pyramidal symptoms in the lower extremities) in adults or children;
- the ability for subtle movements decreases (embroidery, playing musical instruments);
- muscle tone increases (hypertensive type), which is called spasticity. Thus, with pyramidal insufficiency of the legs, a spastic gait occurs, in which there is weakness in the legs and at the same time a limitation in the range of movements;
- tendon reflexes increase. When struck with a hammer, the knees and elbows “jump”; when a lying person tries to sharply bend the foot, it makes convulsive twitches - clonus;
- at the same time, skin reflexes, for example, abdominal ones, decrease;
- pathological reflexes arise, for example, Babinsky, Zhukovsky, Bekhterev, Oppenheim, Rossolimo. For example, Babinski's sign is that when a thin, ticklish object (such as the point of a pencil) is passed along the edge of the sole from bottom to top, the toes will fan out. Normally they should bend.
In children under the age of one and a half to two years, the toes on the leg, on the contrary, should extend, and then extension (extension) is replaced by flexion (flexion). Therefore, treating a child under one year old just because he has a pathological reflex is illiterate. When the pyramid system matures, it will disappear on its own. And a two-year-old baby already has signs of normal foot reflexes, and at the age of 3–5 years the motor system is already mature.
In patients with deep paresis, or central plegia, Babinski's symptom is sharply positive.
- there is no muscle atrophy. This serves as an important differential sign between peripheral or flaccid paralysis and central or spastic (pyramidal) paralysis.
Diagnosis of deficiency level
A few words need to be said about the difficulty of accurately diagnosing pyramidal insufficiency. For example, all of the following options are the subject of our topic, from top to bottom:
- subcortical lesions (with tumors, cerebral infarctions, hematomas). Fine and professional fine motor skills are impaired or epileptic seizures occur;
- when the internal capsule (a place of high density of bundles) is damaged, unilateral hemiparesis occurs, or paralysis of the arms and legs, with possible paralysis of the hypoglossal nerve and paresis of the muscles of half the face;
- involvement of the cerebral peduncle adds to hemiparesis paralysis of the oculomotor nerve on the same side (Weber syndrome);
- going down below, into the bridge, we get paralysis of one arm or leg or even bilateral hemiplegia, that is, two unilateral paralysis on both sides: as a result, both arms and legs are paralyzed, this can be expressed to varying degrees, from mild paresis to complete tetraplegia;
- when the “culprit” of the article itself, the pyramid, is damaged, flaccid paresis of the arm and leg on the opposite side occurs;
- The cervical level suffers from multiple sclerosis and amyotrophic lateral sclerosis. The cross was higher, so hemiparesis or hemiplegia occurs on the groan of the lesion;
- thoracic level of insufficiency causes spastic paralysis of one leg on the groan of defeat;
- finally, damage to the motor root, which can be considered the end of the tract (the last neuron), causes flaccid paresis of one limb.
Now compare how quickly, often without examination, the diagnosis of “pyramidal insufficiency” appears in the outpatient chart. Miracles, and that’s all...
Diagnosis of pyramidal insufficiency
First of all, an examination is carried out by a pediatric neurologist, who conducts various tests for age-related reflexes. Very effective and indicative diagnostic tools are tomography and electroencephalography. In cases where a child not only experiences convulsive muscle twitching, but also a fever, lethargy, etc., a spinal cord puncture may be prescribed to identify the underlying disease that requires urgent treatment (for example, meningitis).
Clinical picture and diagnostic methods
To identify pyramidal syndrome in adults, a simple examination by a neurologist is not enough. The patient must undergo a series of modern diagnostic procedures. To obtain comprehensive information about the patient’s health status, the neurologist will need the results of the following examinations:
Pyramidal insufficiency in adulthood also manifests itself in more noticeable symptoms that can be detected during a medical examination:
- hypertension;
- increased tone of the muscles of the arms and legs;
- convulsions;
- complete or partial paralysis of different parts of the body;
- violations of reflex activity, in particular, a decrease in its speed;
- in some cases, especially if the damage has occurred to the hypothalamic-pituitary system, sexual dysfunction and increased body weight may be observed.
Treatment of pyramidal insufficiency in children
In the case of real pyramidal insufficiency, medical measures are aimed at treating the underlying disease that caused this insufficiency, including surgical intervention. However, in most cases, apart from hypertonicity of the lower leg, no other symptoms are detected. In this case, the main treatment is to relieve hypertonicity and form the correct position of the ankle joint.
- Massage and exercise therapy. It is important to combine visits to an experienced specialist who can relax and strengthen muscles with light massages at home. Swimming and light physical exercise also contribute to the proper development of muscles and joints, and the formation of good coordination of movements. To restore energy metabolism and the proper flow of fluids in the body, you can contact an osteopath.
- Orthopedic shoes. If pyramidal insufficiency is discovered at an age when the child has already begun to walk, it is important to correctly form the ankle joint, since its incorrect position will lead not only to injuries to the ankle, but also to disruption of the entire musculoskeletal system.
- Vitamin therapy.
- Sometimes medications are prescribed to improve metabolic processes and nerve conduction.
Childhood lays the foundation for health for the rest of your life. It is very important to respond to any deviations from the norm in a timely manner so as not to miss a serious illness that can significantly reduce a person’s quality of life. If you suspect any pathology or you just want to know that everything is fine with your child, contact our Aximed neurology clinic. Our doctors are qualified specialists with many years of experience; the clinic is equipped with the most modern equipment and has the latest diagnostic tools. With us you will receive a comprehensive diagnosis and comprehensive consultation from the best neurologists in Kyiv.
A rare cause of stroke in a young patient
Patient A, 41 years old, was admitted to the 1st neurological department on August 21, 2015.
Upon admission, the patient was concerned about numbness and awkwardness in the left arm and left half of the body, dizziness, instability when walking, nausea, headache, discomfort and pain in the left cervical spine, pain in the lumbar spine radiating down the back of the left leg.
History: 08/19/15, after eating food from a catering establishment, abdominal discomfort occurred, and then repeated loose stools. On August 19 and August 20, I followed a gentle diet and took enterosorbents. Also, a few days before the development of the above complaints, while playing at home with the children, there was a sharp load on the left arm with subsequent pain in the cervical spine. On the morning of August 20, I acutely felt dizziness of a “systemic” nature, nausea, and within an hour after that, numbness developed in my left hand. He was urgently hospitalized at City Clinical Hospital No. 71 with suspected ischemic stroke, where a CT scan of the brain was performed; no pathology was identified (according to the patient). 08.21.15. At his own request, he was discharged from City Clinical Hospital No. 71, continued the examination on an outpatient basis: Doppler ultrasound of the brachiocephalic arteries was performed: Features of the development of VA: entry of the left VA at the level of the 5th cervical vertebra, on the right - at the level of the 6th cervical vertebra. Difference in VA diameters and hemodynamic predominance of the right VA. Non-linearity of the course of both PAs along the entire visible length, more on the left.
X-ray of the cervical spine with functional tests: Violation of statics. Osteochondrosis. Disco-osteophytic complex C5-C6. Retrolisthesis C2, C3, C4.
MRI of the brain: in the media-basal part of the left hemisphere of the cerebellum, an irregularly shaped area with fairly clear contours is determined by an area of altered MP signal: moderately hyperintense on T2 VI, T2 flair, moderately hypointense on T1 VI, with enhancement on T2 diff, with a maximum size of 3 , 71×1.81×1.87 cm without signs of perifocal edema. In the white matter of the frontal and parietal lobes, subcortically and paraventricularly, single microfocal changes in the MP signal of a vascular nature, measuring 0.14-0.18 cm, were detected. No additional formations were identified in the area of the cerebellopontine angles. The internal auditory canals are not dilated. The subarachnoid space of the cerebral hemispheres and cerebellum is not expanded. The convexital grooves of the cerebrum and cerebellum are without features. Uneven expansion of the perineural liquor spaces around the optic nerves on both sides; (indirect MP sign of increased intracranial pressure). Otherwise, the orbits are without features. The cerebellar tonsils are located at the level of the foramen magnum. The craniovertebral junction is without features. In the right maxillary sinus: on the upper wall there is an MR signal with the characteristics of a polyp with a diameter of 0.644 cm; on the lower wall there is an MP signal with the characteristics of a polyp 0.56×1.56 cm, unevenly thickened, hyperhydrated mucosa of the lower wall. In the left mandibular sinus: MP signals with the characteristics of polyps on the outer and lower walls measuring 1.85×1.35 cm and 1.02×1.26 cm and MP characteristics of a fluid-containing cavity with a diameter of 1.504 cm. Conclusion: MR data stroke of ischemic type in the vertebrobasilar region, MRI picture of a few foci of gliosis, indirect signs of intracranial hypertension; MRI signs of polyps of the maxillary sinuses.
Based on the results of an MRI of the brain, he was urgently hospitalized at Clinical Hospital No. 1 for examination and treatment.
History: osteochondrosis of the cervical spine, periodically in the morning I am bothered by numbness of 3-5 fingers of both hands, more so than the right one. Discomfort and pain in the cervical spine have also been a concern for several years. Engaged in swimming and kinesiotherapy.
She is being observed by an endocrinologist for nodular goiter.
Since 2012, according to MRI of the brain (performed for non-systemic dizziness and numbness in the fingertips of both hands, which arose after a long flight), polyps of both maxillary sinuses up to 0.7 cm have been identified. The above episode of dizziness went away within a few days while taking betaserc .
Operations: septoplasty.
Allergy history: not burdened.
Heredity is burdened with cancer: mother - intestinal cancer, father - cancer in the nasal cavity (does not specify).
Objectively upon admission: The condition is relatively satisfactory. The skin is of normal color. There is no swelling. In the lungs, the breathing is vesicular with a hard tint, there are no wheezes. NPV up to 14 per minute. Heart sounds are muffled, rhythmic, heart murmurs cannot be heard, heart rate is 62 per minute. Blood pressure 110/70 mm Hg. Art. The tongue is clean and moist. The abdomen is soft, painless on palpation, there are no symptoms of peritoneal irritation, peristalsis can be heard. The liver does not protrude from under the edge of the costal arch. The kidneys are not palpable. The symptom of effleurage is negative on both sides. Body temperature 36.6 0C. He controls urination and has daily bowel movements.
Neurological status: Conscious, contactable, oriented in place, time, self. The mood background is smooth. There are no meningeal signs. Pupils D=S Photoreactions preserved. Movement of the eyeballs is not limited. Medium-amplitude horizontal nystagmus when looking to the right, fading. There are no sensory disturbances on the face. The exit points of the trigeminal nerve are painless. The face is symmetrical. The pharyngeal reflex is preserved. Swallowing and phonation are not impaired. Tongue in the midline. Right-sided pyramidal insufficiency. Tendon reflexes are low, S=D. There are no pathological foot signs. Muscle tone is not changed. There are no sensory disturbances. In Romberg's pose he falls to the right. Coordinator tests are performed with intention and ataxia. Gait with ataxia.
Additional examination methods:
Upon admission: a general blood test shows moderate leukocytosis with a shift in the leukocyte formula to the right, eosinopenia, erythrocytosis; a blood test revealed a moderate decrease in serum iron; Urinalysis revealed proteinuria 0.3 g/l, erythrocyturia.
Blood test for HIV, hepatitis B, C, MR for syphilis - negative.
ECG : Sinus rhythm with heart rate 77/min. , vertical position of the EOS. AV block of the first degree with violation of the MPP. Changes in the LV myocardium.
ECHO-CG : Aorta of medium echogenicity. The valve apparatus has not been changed. The heart chambers are not dilated. Local and global contractility is preserved. The walls of the left ventricular myocardium are not thickened. With DKG-MR-0-1 st., TR-0-1 st. Diastolic function was preserved.
To search for rare causes of stroke, the patient was examined to exclude vasculitis, cardioembolic brain damage, and thrombophilia. :
In the hemostasis system (APTT, Prothrombin time, Prothrombin index, Fibrinogen, Thrombin time, D-dimer) - without pathology.
Immunological examination of T4 (f), TSH is normal.
Hemostasiological studies: Protein S (free), Protein C, Antithrombin III (AT III) - normal, Lupus anticoagulant - not detected.
Diagnostics of autoimmune diseases: Antibodies to double-stranded DNA (dsDNA), Antibodies to phospholipids IgG (APL screen), Antibodies to phospholipids IgM (APL screen), Antibodies to mitochondrial membrane antigens (AMA-M2), Antibodies to nuclear antigens, screening (ANA screen ), Antibodies to single-stranded DNA (ssDNA), Antibodies to cardiolipin IgG (CLP-IgG), Antibodies to cardiolipin IgM (CLP-IgM) – are within the reference values.
PCR diagnosis of respiratory infections (DNA of herpes simplex virus types I and II, Mycobacterium tuberculosis complex, DNA of herpes virus type VI, Listeria monocytogenes DNA, Toxoplasma gondii DNA, Varicella-Zoster virus DNA, Candida albicans/glabrata/krusei DNA, Candida albicans DNA, DNA of Candida krusei, DNA of Candida glabrata, DNA of Cytomegalovirus/Epstein-Barr virus/Herpes virus type VI, RNA of rubella virus (Rubella virus), DNA of cytomegalovirus, DNA of Epstein-Barr virus) - not detected.
Blood test for markers of thrombophilia: PCR analysis revealed no mutations in the factor 5, methylenetetrahydrofolate reductase and prothrombin genes.
A diagnostic lumbar puncture was performed: in the analysis of the cerebrospinal fluid, protein cellular dissociation was noted, an increase in glucose levels, a decrease in the level of chlorides in the cerebrospinal fluid; In a microbiological study of the cerebrospinal fluid - microflora was not isolated, gram +, gram -, fungi - no growth was detected.
Upon discharge, the blood test, blood test, and CAM were monitored - all indicators were within the reference values.
ECG : Sinus rhythm with heart rate 77/min. , vertical position of the EOS. AV block of the first degree with violation of the MPP. Changes in the LV myocardium.
ECHO-CG : Aorta of medium echogenicity. The valve apparatus has not been changed. The heart chambers are not dilated. Local and global contractility is preserved. The walls of the left ventricular myocardium are not thickened. With DKG-MR-0-1 st., TR-0-1 st. Diastolic function was preserved.
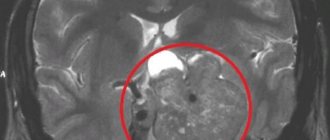
MRI examination of the brain : In the left hemisphere of the cerebellum, a zone of hyperintense MR signal with clear uneven contours on T2WI and in the TIRM program and hypointense on T1WI, measuring up to 42x25x25 mm, is determined. After intravenous administration of Omniscan, no areas of pathological accumulation of contrast pretarate were detected in the affected area or other parts of the brain. Conclusion: MR picture of a fresh ischemic stroke in the left hemisphere of the cerebellum (see Fig. 1).
MRI examination of the cervical spine : signs of moderate degenerative-dystrophic changes in the cervical spine with a predominant lesion of C5-C7. Small hernia C5-C6. Focal lesion of the spinal cord at the level of the C4 vertebra.
Selective angiography of the brachiocephalic arteries: The aortic arch is without features. The brachiocephalic trunk is not changed. The right CCA is patent, without changes. The right ESA is passable, without changes. The right ICA is passable, without changes. The right vertebral artery is large, patent, without changes. Intracranial sections are unchanged. The right subclavian artery is patent, without changes. The right anterior cerebral and middle cerebral arteries and their branches are patent, without changes. The left CCA is patent, without changes. The left ESA is passable, without changes. The left ICA is passable, without changes. The left vertebral artery is occluded in p/3 and cannot be further visualized. Intracranial sections are unchanged. The left subclavian artery is patent, without changes. The left anterior cerebral and middle cerebral arteries and their branches are patent, without changes (see Fig. 2).
The results of blood tests for autoimmune lesions, coupled with the results of angiography, can exclude the diagnosis of vasculitis. The results of angiography and the results of a cerebrospinal fluid analysis for infection can exclude virus-associated vasculitis. Cardioembolic stroke and thrombophilia were also excluded.
Considering the presence of pain syndrome at the cervical level, anamnestic indication of stretching of the cervical spine several days before the onset of symptoms, dissection of the left VA was the cause of its occlusion and subsequent stroke.
Dissection is the penetration of blood through an intimal tear from the lumen of the artery into its wall with the formation of an intramural hematoma (IMH), which stenoses/occludes the lumen of the artery or is a source of arterioarterial embolism, which in turn leads to ischemic stroke.
The main clinical signs of VA dissection are ischemic cerebrovascular accidents and isolated neck/headache. This pain occurs in about a third of cases. Rare manifestations include circulatory disorders in the cervical spinal cord, isolated radiculopathy, and hearing impairment. In more than a third of patients, dissection is found in both VAs, and dissection of one VA may be the cause of UCI, and the second VA may be the cause of isolated neck/headache or be clinically asymptomatic and detected only by neuroimaging. A characteristic feature of NMC during VA dissection is its association with neck/headache on the side of the dissected VA. The causes of neck/headache during VA dissection are irritation of the pain receptors of the arterial wall by the hematoma forming in it, as well as ischemia of the neck muscles, the blood supply of which involves the branches of the VA.
Thus, our patient developed
Acute circulatory disturbance in the brain and spinal cord of the ischemic type in the posterior inferior cerebellar artery and anterior spinal artery (in the left hemisphere of the cerebellum, in the C5 segment of the spinal cord) dated August 20, 2015 against the background of occlusion of the left vertebral artery caused by its dissection.
Treatment was carried out: intravenous drip: magnesium sulfate, Mexidol, Ceraxon, Cerebrolysin, Actovegin; i/m: eglonyl; orally: glycine, eglonyl, cardiomagnyl, omez. ERT. Exercise therapy, IRT, ILBI, Erythrocytepheresis.
As a result of the treatment, the patient's condition showed positive dynamics: headaches regressed, manifestations of vestibulo-ataxic syndrome decreased, and vague hypoesthesia on the left hand remained.