The median nerve is formed by fibers of a number of spinal nerves and has mixed functions. Its main purpose is to innervate some muscles of the forearm and hand. With the development of median nerve neuritis, deterioration in the functions of the affected limb, severe pain and a number of other symptoms appear. If treatment is not provided in a timely manner due to poor quality, neuropathy of the median nerve can result in a lifelong loss of the ability to fully use the arm, up to and including disability.
Contacting specialist neurologists from the Health Workshop network of clinics will help you quickly carry out a diagnosis, draw up a list of necessary health measures and create conditions for complete relief from the manifestations of this disease. Trust your health to our doctors!
Causes of median nerve neuropathy
The causes of median nerve neuropathy include:
- trauma - bruises and wounds with partial rupture of fibers, fractures of the shoulder or forearm (if the nerve was damaged by bone fragments), fractures inside the elbow, wrist (the place where the hand and forearm connect) joints - compression of the median nerve of the arm;
- dislocations, inflammation of these joints;
- the nerve is pinched by a tumor or hematoma, rarely in the presence of a process on the humerus (compressive ischemic neuropathy of the median nerve);
- endocrine dysfunction;
- gout and rheumatism lead to changes in tissues, which can cause neuropathy.
But most often, median nerve neuropathy affects people with specific professional activities: builders, packers, musicians. Breastfeeding women are also susceptible to the disease because they hold the baby for a long time so that his head rests on her forearm.
Tunnel syndromes of the hand
The following forms of hand tunnel syndromes are distinguished:
1.Median nerve tunnels
Carpal tunnel syndrome (wrist) - carpal tunnel syndrome, carpal tunnel syndrome
Pronator syndrome (pronator teres syndrome (in/3 of the forearm)) - Seyfarth syndrome, newlyweds' palsy, honeymoon palsy, lovers' palsy;
Supracondylar syndrome (n/3 shoulders) - Strother's band syndrome, Coulomb, Lord and Bedossier syndrome.
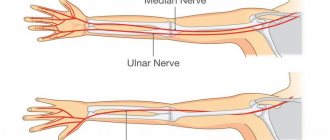
2. Ulnar nerve tunnels
Guyon's syndrome (palm) - ulnar carpal tunnel syndrome, Guyon's bed syndrome, compression-ischemic neuropathy of the distal part of the ulnar nerve;
Cubital tunnel syndrome (elbow) - compression neuropathy of the ulnar nerve in the cubital tunnel, cubital tunnel syndrome, late ulnar-cubital traumatic palsy.
3. Radial nerve tunnels
Radial nerve compression syndrome (in the armpit area) - “crutch paralysis”
Radial nerve compression syndrome (at the level of the middle third of the shoulder) - spiral canal syndrome, “Saturday night paralysis”, “park bench”, “bench” syndrome
Radial nerve compression syndrome (in the subulnar region) - tennis elbow, supinator syndrome, Froese syndrome, Thomson-Kopell syndrome, tennis elbow syndrome, compression neuropathy of the deep (posterior) branch of the radial nerve in the subulnar region.
Tunnel syndromes account for 1/3 of diseases of the peripheral nervous system. There are descriptions of more than 30 forms of tunnel neuropathies in the literature.
Causes
The anatomical narrowness of the canal is, according to many authors, only a predisposing factor in the development of tunnel syndrome. In recent years, evidence has accumulated indicating that this anatomical feature is genetically determined. Another possible cause of the development of tunnel syndrome may be the presence of congenital developmental anomalies in the form of additional fibrous cords, muscles and tendons, and rudimentary bone spurs.
Some metabolic and endocrine diseases (diabetes mellitus, acromegaly, hypothyroidism), diseases of the joints, bone tissue and tendons (rheumatoid arthritis, rheumatism, gout), conditions accompanied by hormonal changes (pregnancy), space-occupying formations of the nerve itself (schwannoma, neuroma) contribute to the development of tunnel syndrome ) and outside the nerve (hemangioma, lipoma). The development of tunnel syndromes is facilitated by frequently repeated stereotypical movements and injuries. Therefore, the prevalence of carpal tunnel syndrome is significantly higher in representatives of certain professions (for example, stenographers have carpal tunnel syndrome 3 times more often).
Clinical manifestations
The most characteristic feature of carpal tunnel syndrome is pain . Usually pain appears during movement, then occurs at rest. The pain may wake the patient at night. Pain in tunnel syndromes is caused by inflammatory changes occurring in the zone of nerve-canal conflict and nerve damage. Tunnel syndromes are characterized by such manifestations of neuropathic pain as a sensation of electric current passing (electrical shooting), burning pain. In later stages, pain may be due to muscle spasm
Then movement disorders arise, manifesting themselves in the form of decreased strength and rapid fatigue. In some cases, the development of the disease leads to atrophy and the development of contractures (“clawed paw”, “monkey paw”).
When arteries and veins are compressed, paleness occurs, a decrease in local temperature, or the appearance of cyanosis and swelling in the affected area.
Diagnostics
In some cases, it is necessary to conduct electroneuromyography (the speed of impulses along the nerve) to clarify the level of nerve damage. tunnel syndrome. Using ultrasound, thermal imaging, MRI, nerve damage, space-occupying formations or other pathological changes can be determined.
Principles of treatment
Stop exposure to the pathogenic factor. Immobilization with the help of orthoses, bandages, splints, allowing to achieve immobilization specifically in the area of damage.
Change the usual locomotor stereotype and lifestyle. Tunnel syndromes are often the result not only of monotonous activity, but also of ergonomic disorders (improper posture, awkward position of the limb during work). Training in special exercises and physical therapy are an important component of the treatment of tunnel neuropathies at the final stage of therapy.
Pain therapy
Anti-inflammatory therapy
Traditionally, for carpal tunnel syndromes, NSAIDs with a more pronounced analgesic and anti-inflammatory effect (diclofenac, ibuprofen) are used. For moderate or severe pain, it is advisable to use the drug Zaldiar (a combination of low doses of the opioid analgesic tramadol (37.5 mg) and the analgesic/antipyretic paracetamol (325 mg). Thanks to this combination, a multiple increase in the general analgesic effect is achieved with a lower risk of side effects.
Impact on the neuropathic component of pain. When pain is the result of neuropathic changes, it is necessary to prescribe drugs recommended for the treatment of neuropathic pain: anticonvulsants (pregabalin, gabapentin), antidepressants (venlafaxine, duloxetine), plates with 5% lidocaine "Versatis". Injections of anesthetic + hormones. An effective and acceptable treatment method for most types of tunnel neuropathies is a blockade with the introduction of novocaine and a hormone (hydrocortisone) into the pinched area.
Other methods of pain relief. An effective way to reduce pain and inflammation is electrophoresis, phonophoresis with dimexide and other anesthetics. They can be carried out in a clinic setting.
Symptomatic treatment. For tunnel syndromes, decongestants, antioxidants, muscle relaxants, and drugs that improve trophism and nerve functioning (ipidacrine, vitamins) are also used.
Surgical intervention. Surgical treatment is resorted to when other methods of helping the patient are ineffective. Surgical intervention consists of releasing the nerve from compression, “reconstructing the tunnel.”
According to statistics, the effectiveness of surgical and conservative treatment does not differ significantly a year later (after the start of treatment or surgery). Therefore, after a successful surgical operation, it is important to remember about other measures that must be followed to achieve a full recovery: changing locomotor stereotypes, using devices that protect from stress (orthoses, splints, bandages), performing special exercises.
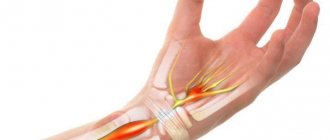
Carpal tunnel syndrome
Carpal tunnel syndrome, or carpal tunnel syndrome, is a common form of compression-ischemic neuropathy. In the population, carpal tunnel syndrome occurs in 3% of women and 2% of men. It is caused by compression of the median nerve where it passes through the carpal tunnel under the transverse carpal ligament. The exact cause of carpal tunnel syndrome is not known. The following factors contribute to compression of the median nerve in the wrist area:
1. Trauma (accompanied by local swelling, tendon sprain).
2. Chronic microtraumatization, often found in construction workers, microtrauma associated with frequent repeated movements (in typists, with constant long-term work with a computer).
3. Diseases and conditions with metabolic disorders, edema, tendon and bone deformities (rheumatoid arthritis, diabetes mellitus, hypothyroidism, acromegaly, amyloidosis, pregnancy).
4. Volumetric formations of the median nerve itself (neurofibroma, schwannoma) or outside it in the wrist area (hemangioma, lipoma).
Clinical manifestations
Carpal tunnel syndrome is manifested by pain, numbness, goosebumps and weakness in the arm and hand. Pain and numbness extend to the palmar surface of the thumb, index, middle and ring fingers, as well as to the dorsum of the index and middle fingers. The following tests are used to clarify the diagnosis of carpal tunnel syndrome.
Tinel test
Tapping the wrist (above the median nerve passage) with a neurological hammer causes a tingling sensation in the fingers or pain radiating (electrical shooting) to the fingers; pain may be felt in the area of the tap. Tinel's sign is found in 26-73% of patients with carpal tunnel syndrome.
Durkan test
Compression of the wrist in the area of the median nerve causes numbness and/or pain in the I-III, half of the IV fingers.
Phalen test
Flexing or extending the wrist 90 degrees causes numbness, tingling or pain in less than 60 seconds. A healthy person may develop similar sensations, but not earlier than after 1 minute.
Opposition test
With severe thenar weakness at a later stage, the patient is unable to connect the thumb and little finger, or the doctor can easily separate the patient's closed thumb and little finger.
Differential diagnosis
Carpal tunnel syndrome must be differentiated from arthritis of the carpo-metacarpal joint of the thumb, cervical radiculopathy, and diabetic polyneuropathy.
Treatment
In mild cases of carpal tunnel syndrome, ice compresses and a decrease in load can help. If these measures do not help, the following is necessary:
- Wrist immobilization. using a splint or orthosis. Immobilization should be carried out at least overnight, and preferably for 24 hours a day in the acute period.
- Drugs from the NSAID group are effective if the inflammatory process dominates in the pain mechanism.
- If the use of NSAIDs is ineffective, it is advisable to inject novocaine with hydrocortisone into the wrist area.
- Electrophoresis with anesthetics and corticosteroids.
- Surgery. For mild or moderate carpal tunnel syndrome, conservative treatment is more effective. When all means of conservative care have been exhausted, surgical treatment is resorted to, which consists of partial or complete resection of the transverse ligament and release of the median nerve from compression. Endoscopic surgical methods are used.
Pronator teres syndrome (Seyfarth syndrome)
This is an entrapment of the median nerve in the proximal part of the forearm between the pronator teres bundles. It usually begins to manifest itself after significant muscle load for many hours with the participation of the pronator and flexor digitorum muscles. Similar types of activities are often found among musicians (pianists, violinists, flutists, and especially often among guitarists), dentists, and athletes.
Long-term tissue compression is of great importance in the development of pronator teres syndrome. This can happen, for example, during deep sleep when the newlywed’s head is positioned for a long time on the partner’s forearm or shoulder. In this case, the median nerve in the pronator snuffbox is compressed, or the radial nerve is compressed in the spiral canal when the partner’s head is located on the outer surface of the shoulder (see radial nerve compression syndrome at the level of the middle third of the shoulder). In this regard, to designate this syndrome, the terms honeymoon palsy, newlyweds' paralysis, and lover's palsy have been adopted. Pronator teres syndrome sometimes occurs in nursing mothers. In them, compression of the nerve in the pronator teres region occurs when the child’s head lies on the forearm for a long time.
Clinical manifestations
With the development of pronator teres syndrome, pain and burning occurs 4-5 cm below the elbow joint, along the anterior surface of the forearm, and pain radiates to the I-III, half of the IV fingers and palm.
Tinel syndrome
In case of pronator teres syndrome, Tinel's sign will be positive when tapping with a neurological hammer in the area of the pronator snuff box (on the inside of the forearm).
Pronator-flexor test
Pronating the forearm with a tightly clenched fist while creating resistance to this movement (counteraction) leads to increased pain. Increased pain can also be observed when writing (prototype of this test).
When studying sensitivity, a violation of sensitivity is revealed on the palmar surface of the first three and a half fingers and palm. Thenar atrophy in pronatar teres syndrome is usually not as severe as in progressive carpal tunnel syndromes.
Suprocondylar process syndrome of the shoulder (Strother's band syndrome, Coulomb, Lord and Bedosier syndrome)
In the population, in 0.5-1% of cases, a variant of the development of the humerus is observed, when a “spur” or supracondylar process (apophysis) is found on its distal anteromedial surface, the median nerve is displaced and stretched, which makes it vulnerable to damage.
This tunnel syndrome was described in 1963 by Coulomb, Lord and Bedossier and has almost complete similarities with the clinical manifestations of pronator teres syndrome: pain, paresthesia, and decreased flexion strength of the hand and fingers are detected in the area of innervation of the median nerve. In contrast to pronator teres syndrome, when the median nerve is damaged under Strather's ligament, mechanical compression of the brachial artery with corresponding vascular disorders is possible, as well as severe weakness of the pronator teres and minor pronators.
In the diagnosis of suprocondylar process syndrome, the following test is performed: when extending the forearm and pronation in combination with formed flexion of the fingers, painful sensations are provoked with a localization characteristic of compression of the median nerve. X-ray examination is indicated.
Treatment involves resection of the supracondylar process (“spur”) of the humerus and ligament.
Cubital tunnel syndrome
Cubital tunnel syndrome is compression of the ulnar nerve in the cubital tunnel at the elbow joint between the medial epicondyle of the humerus and the ulna. It ranks second in frequency of occurrence after carpal tunnel syndrome.
Cubital tunnel syndrome can be caused by frequently repeated flexion of the elbow joint, i.e. the disorder may occur with normal, frequently repeated movements in the absence of obvious traumatic injury. Relying on your elbow while sitting may contribute to the development of cubital tunnel syndrome. Patients with diabetes and alcoholism are at greater risk of developing cubital tunnel syndrome.
Clinical manifestations
Manifested by pain, numbness and/or tingling. Pain and paresthesia are felt in the lateral part of the shoulder and radiate to the little finger and half of the fourth finger. Another sign of the disease is weakness in the arm. For example, it becomes difficult for a person to pour water from a kettle. Subsequently, the hand on the sore arm begins to lose weight and muscle atrophy appears.
Diagnostics
In the early stages of the disease, the only manifestation other than weakness of the forearm muscles may be loss of sensation on the ulnar side of the little finger. The following tests can help verify the diagnosis of Cubital Tunnel Syndrome.
Tinel test
The occurrence of pain in the lateral part of the shoulder, radiating to the ring finger and little finger when tapping with a hammer over the area where the nerve passes in the area of the medial epicondyle.
Equivalent of Phalen's sign
Sudden bending of the elbow will cause paresthesia in the ring and little fingers.
Frohman's test
Due to weakness of the abductor policis brevis and flexor policis brevis, there will be excessive flexion at the interphalangeal joint of the thumb on the affected hand in response to a request to hold a paper between the thumb and index finger.
Wartenberg test
When you put your hand in your pocket, the little finger is moved to the side and does not go into the pocket.
Treatment
It is recommended to fix the elbow joint in an extension position at night using orthoses, hold the car steering wheel with your arms straightened at the elbows, and straighten the elbow when using a computer mouse. In the absence of a positive effect from the use of traditional means: NSAIDs, COX-2 inhibitors, splinting did not have a positive effect within 1 week, an injection of an anesthetic with hydrocortisone is recommended.
If the effect of these measures is insufficient, surgery is performed. All techniques for surgical release of the nerve involve moving the nerve anterior to the internal epicondyle. After the operation, treatment is prescribed to quickly restore nerve conduction.
Guyon's tunnel syndrome
It develops due to compression of the deep branch of the ulnar nerve in the canal formed by the pisiform bone, the hook of the hamate bone, the palmar metacarpal ligament and the palmaris brevis muscle. There are burning pains and sensitivity disorders in the IV-V fingers, difficulty in pinching movements, adduction and extension of the fingers.
The syndrome is very often the result of prolonged pressure from working tools (vibrating tools, screwdrivers, pliers), and is more common among gardeners, leather cutters, tailors, violinists, and people who work with jackhammers. May sometimes develop after using a cane or crutch. Enlarged lymph nodes, fractures, arthrosis, arthritis, ulnar artery aneurysm, tumors and anatomical formations around Guyon’s canal can also cause compression.
Differential diagnosis
In the hand, pain occurs in the hypothenar region and the base of the hand, as well as intensification and irradiation in the distal direction during provoking tests. Sensitivity disorders in this case occupy only the palmar surface of the IV-V fingers. On the back of the hand, sensitivity is not impaired.
Differential diagnosis is made with radicular syndrome (C8). Paresthesia and sensitivity disorders can also appear along the ulnar edge of the hand. Paresis and hypotrophy of the hypothenar muscles are possible. But with C8 radicular syndrome, the zone of sensory disorders is much larger than with Guyon’s canal, and there is no wasting or paresis of the interosseous muscles. With bilateral nerve damage, ALS is sometimes misdiagnosed.
Treatment
If diagnosed early, restricting activity may help. It is recommended to use fixators: orthoses, splints at night or during the day to reduce trauma.
If conservative measures fail, surgical treatment is performed to reconstruct the canal in order to release the nerve from compression.
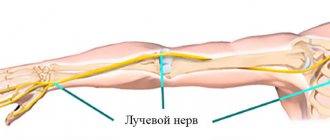
Radial nerve compression syndrome
There are 3 options for compression lesions of the radial nerve:
- Compression in the armpit area. Occurs due to the use of a crutch, paralysis of the extensors of the forearm, hand, main phalanges of the fingers, abductor pollicis muscle, and supinator occurs. The flexion of the forearm is weakened, the reflex from the triceps muscle fades. Sensitivity disappears on the dorsal surface of the shoulder, forearm, partly the hand and fingers.
- Compression at the level of the middle third of the shoulder ("Saturday night paralysis", "park bench", "bench" syndrome). Occurs more often. But most often, compression occurs due to compression of the nerve on the outer back surface of the shoulder during deep sleep (often after drinking alcohol). Nerve compression can be caused by the partner's head lying on the outer surface of the shoulder.
- Compressive neuropathy of the deep (posterior) branch of the radial nerve in the subulnar region (supinator syndrome, Froese syndrome, Thomson-Kopell syndrome, tennis elbow syndrome).
This is a chronic disease caused by a degenerative process in the area of muscle attachment to the lateral epicondyle of the humerus. It manifests itself as pain in the extensor muscles of the forearm, their weakness and hypotrophy.
Treatment includes general etiotropic and local therapy. There is a possible connection between tunnel syndrome and rheumatism, brucellosis, arthrosis of metabolic origin, and hormonal disorders. Anesthetics and glucocorticoids are injected locally into the area of the pinched nerve. Physiotherapy is carried out, the prescription of vasoactive, decongestant and nootropic drugs, antihypoxants and antioxidants, muscle relaxants, ganglion blockers, etc. Surgical decompression with dissection of the tissues compressing the nerve is carried out if conservative treatment is unsuccessful.
Literature
- Al-Zamil M.H. Carpal syndrome. Clinical neurology, 2008, No. 1, pp. 41-45
- Berzins Yu.E., Dumbere R.T. Tunnel lesions of the nerves of the upper limb. Riga: Zinatne, 1989, p.212.
- Zhulev N.M. Neuropathies: a guide for doctors. - St. Petersburg: Publishing house SpBmapo, 2005, p.416
- Levin O.S. "Polyneuropathy", MIA, 2005
- Atroshi I., Larsson GU, Ornstein E., Hofer M., Johnsson R., Ranstam J. Outcomes of endoscopic surgery compared with open surgery for carpal tunnel syndrome among employed patients: randomized controlled trial. BMJ., Jun 24 2006; 332(7556):1473.
- Graham RG, Hudson DA, Solomons M. A prospective study to assess the outcome of steroid injections and wrist splinting for the treatment of carpal tunnel syndrome. Plast Reconstr Surg., Feb 2004; 113(2):550-6.
- Horch RE, Allmann KH, Laubenberger J., et al. Median nerve compression can be detected by magnetic resonance imaging of the carpal tunnel. Neurosurgery, Jul 1997; 41(1):76-82; discussion 82-3.
- Golubev V.L., Merkulova D.M., Orlova O.R., Danilov A.B., Department of Nervous Diseases of the I.M. Sechenov Faculty of Physics and Postgraduate Medical Academy
Diagnostics
A neurologist can diagnose median nerve neuropathy by performing an examination and electroneuromyography. Also, to prescribe the correct treatment and make a diagnosis, the doctor must examine the structures of the bones and muscles by conducting x-rays, ultrasound and tomography.
During the examination, the neurologist asks the patient to undergo several tests, based on the results of which a diagnosis is made:
- make a fist; with neuropathy, the first two fingers cannot be assembled;
- cross your second (index) finger with your nail;
- stretch the paper sheet, grasping it only with the thumb and index (first and second) fingers;
- bring the tip of your thumb and little finger together.
To diagnose the affected area, a neurologist examines pain along the nerve by tapping at the site of injury. This diagnostic method is called Tinel's symptom.
To exclude diseases with similar symptoms (polyneuropathy, brachial plexitis, vertebrogenic syndromes), electroneuromyography is necessary. Joints and bones are also examined using ultrasound, MRI, and CT. The patient also needs to take a blood test for RF, proteins, sugar and to study hormones.
Depending on the root cause of the disease, together with a neurologist, the diagnosis should be carried out by an endocrinologist, orthopedist or traumatologist.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0.01 | 0.01 | 0.1 | 8 | 8 | 10 | 10 | 0.01 | 0.01 | 0.1 | 8 | 8 | 10 | 10 |
Treatment of median nerve neuropathy
Depending on the onset and development of the disease, median nerve syndrome is treated not only by a neurologist, but also by orthopedic traumatologists, surgeons and endocrinologists.
The first step is to eliminate the cause of median nerve neuropathy - hematoma, tumor, injury, and treat the diseases that caused the neuropathy. Simultaneously with the elimination, pain is relieved and inflammation is relieved. During treatment, it is important to improve the nutrition of the nerve with neurometabolites and vascular agents.
If conservative therapy for median nerve neuralgia was not effective, especially with trauma, then surgical treatment is prescribed.
During the recovery period, it is necessary to engage in physical therapy, hand massage, manual therapy, electrical myostimulation, treatment with mud and ozokerite is indicated. In special neurological cases, surgery to restore the median nerve of the arm is indicated.
Types of surgical interventions by technique
Nerve neurolysis
Neurolysis occurs when rough scars form around the nerve fibers, compressing them. Most often, the cause is a fracture or severe bruise of soft tissue. The effectiveness of the intervention reaches 50%. To increase the accuracy of manipulations, a microscope can be used. If the cicatricial adhesions are massive, the electrical excitability of the nerve trunk is checked. If the changes are irreversible, then it is removed and the remaining fragments are stitched together. Access can be external or internal. Neurolysis is carried out in three stages:
- The nerve is isolated from the surrounding affected tissue with a blade or scalpel.
- Scar tissue and dense adhesions are excised.
- The released nerve fiber fits into the formed muscle bed.
Neurotomy
The nerve fiber is cut to eliminate pathological impulses that lead to pain or change the functions of internal organs. Most often performed for peptic ulcers of the duodenum and stomach. Direct indications are irreversible changes in the nerve roots, in which sensitivity and tissue trophism are lost, and motor functions are impaired. An anesthetic block may also be used if the nerve is pinched.
The surgeon isolates the nerve fiber with a scalpel or blade under local anesthesia. To prevent bleeding, the vessels are coagulated, that is, cauterized. To prevent neuromas, microcapsules made of polymer material are installed at the ends of the nerve fiber.
Plastic
For plastic surgery, grafts are used that can be vascularized or non-vascularized. Fragments of nerve fibers that have a vascular “pedicle” are used. The non-blood-supplied type of grafts is recognized as the most effective. Plastic surgery is possible:
- using a solid barrel (free)
- using several grafts (free interfascicular)
- vascularized neurotransplant (free)
- not free according to Strang
- patchwork
- tubulization of nerve fiber
- correction of a nerve fiber defect with its branches
Non-vascularized grafts are used for plastic surgery of small nerve fibers. If it is necessary to restore large fibers, then grafts on a vascular “pedicle” are used. Donors can be subcutaneous nerve fibers, gastrocnemius, ulnar, superficial radial, and peroneal branches.
In order for the grafts to take root more quickly, plastic surgery is performed using microvascular anastomoses, which help nourish the nerve fibers.
Excision of Morton's neuroma
This is a foot disease that is caused by the proliferation of benign fibrous tissue in the area of the plantar nerve fiber. As a result, pain appears in the foot, which intensifies with exercise and wearing tight shoes. Removal of the neuroma is indicated when there is no effect of conservative therapy. During the intervention, resection of the neuroma or dissection of the intermetatarsal ligament is performed. The second method is more gentle. The procedure lasts only 10-15 minutes, after 2 hours you can already walk. However, this technique is dangerous with relapses. Removing a neuroma is more effective because the affected nerve fiber is completely excised.
When is surgery indicated?
- Impaired sensitivity and movement function.
- Tumors.
- Painful neuromas.
- Compression by scars.
- Damage due to trauma.
- Pain syndrome.
Taking into account the nature of the injury, the method of surgical treatment is selected:
- Excision of scar formations – neurolysis;
- Connecting the nerve sheath and applying a special suture;
- Carrying out plastic surgery of nervous tissue.
During surgical treatment, microsurgical techniques are used to make the comparison as accurate as possible.
Rehabilitation
The recovery period takes at least six months. First, touch is restored, then sensitivity when touching two points. For recovery, it is important to recognize objects by touch.
Principles of successful rehabilitation:
- Early intervention;
- Reducing the risk of complications;
- Ensuring healing;
- Restoring the functions of the nerve of the hand;
- Using a multi-stakeholder approach.
Restoration of the hand nerve is carried out at the clinic of the Central Clinical Hospital of the Russian Academy of Sciences, in the department of hand microsurgery. Everything is available here for effective treatment of a nerve rupture in the arm - experienced, highly qualified surgeons work, the most modern microsurgical equipment is used, and the staff is caring.
Registration for a consultation is carried out on the website. You can get the information you are interested in and find out the price of treatment by calling the number provided.
Recovery forecast
Rehabilitation of patients after nerve damage from any type of surgery may require restoration of lost functions. Immediately after the operation, there is pain, which is relieved with painkillers. The sutures are removed after 7-10 days. The surgical wound is treated every day. If the intervention was performed on the limbs, then a plaster cast is indicated to immobilize and prevent the sutures from coming apart. To speed up recovery, physiotherapy, massage, and exercise therapy are indicated.
The speed of healing is affected by:
- patient’s age – the younger the person, the faster the regeneration processes;
- volume and type of injury;
- purpose and size of nerve fiber;
- time from the moment of injury to surgical intervention - this interval should be no more than 1 year, otherwise it will be impossible to restore functions;
- individual characteristics of the body;
- accompanying pathologies.
Healing is better with cut wounds when the ends of the cut fiber have an even cut and are located close to each other. If a fiber close to the neuron is damaged, healing will be slower. Bundles that perform only one function heal better than nerve fibers that are part of a trunk with different purposes.