Familiarize yourself with other diseases starting with "P": Felon, Panic attack, Pancreatitis, Papillomas, Paralysis, Bell's palsy, Paranoia, Paraproctitis, Facial nerve paresis, Periodontitis, Periodontal disease, Paroxysm, Paroxysmal tachycardia, Scab (favus), Pediculosis, Spermatic cord torsion , Bone fracture, Rib fracture, Hip fracture, Post-term pregnancy
How to detect facial nerve paresis
This neurological disease, diagnosed with weakness of the facial muscles, leading to immobility and asymmetry of one part of the face, occurs due to disruption of the passage of impulses of the facial nerve. Outwardly it manifests itself in the patient’s inability to speak clearly, smile normally, or close an eye. With timely contact with a neurologist, the mobility of the facial muscles can be restored.
There are 3 forms of the disease:
- Congenital facial nerve paresis occurs in only 10% of cases. With this pathology, the newborn also experiences other damage to the nerve branches. With this form, the child requires surgical intervention;
- The first syndrome in peripheral paresis is pain in the postauricular area. On one half of the face, swelling of the nerve fibers and muscle hypotonicity occur;
- With central paresis, the eyes and forehead do not suffer from pathology, which preserves the patient’s ability to blink normally. Under the influence of pathology of brain neurons, the muscles of the lower part of the face are affected.
In addition, paresis is classified into stages: acute, subacute, chronic.
Results of surgical treatment of paralysis of facial muscles
The result of these operations (with the exception of static correction) does not appear immediately. As a rule, the result appears after 4-8 months - the first weak movements appear, which gradually intensify with mandatory adherence to the specialist’s recommendations. This is due to the fact that nerves re-grow, according to the literature - up to 1 mm per day. First, sensations appear in the form of “lumbago”, “running goosebumps”, etc. This indicates the growth of the nerve along the nerve fibers. The first movements are quite weak, since the muscles have been without load for a long time, so it takes time for their functional restoration, and it is necessary to constantly load them rationally. Thus, rehabilitation plays a very important key role in the final outcome. And the patient must be prepared for daily exercise and not immediate results.
Causes
The disease can be caused by various factors, which differ depending on the age of the patient. Facial nerve paresis can be affected by:
- Nerve damage due to surgery or otitis media;
- Hypothermia of the head and behind-the-ear area;
- ARVI of the upper respiratory tract;
- Herpetic infections;
- Head injuries;
- Mumps;
- Tuberculosis;
- Polio;
- Syphilis.
The severe inflammatory process that accompanies these pathologies provokes disruption of the facial nerve. In addition, poor blood circulation in the face can affect it. Contributes to this:
- Ischemic stroke;
- Hypertensive crisis;
- Diabetes;
- Multiple sclerosis.
Where is surgical treatment for paralysis of the facial muscles performed?
Specialists from the Department of Maxillofacial and Reconstructive Surgery of the Federal State Budgetary Institution NKCO FMBA of Russia, together with the Department of Ear Diseases, have developed and put into practice a unique method of surgical treatment of patients with paralysis of the facial muscles. The first operations on patients with this pathology in Russia were performed by specialists from the Federal State Budgetary Institution NCCO FMBA of Russia - otosurgeon, MD. Hassan Diab and maxillofacial surgeon Ekaterina Orlova.
A healthy person rarely thinks about how important facial expressions are and what role they play in our lives, especially a smile... Smile more often!
Characteristic clinical signs
Symptoms of the disease are:
- Smoothing the nasolabial fold;
- Drooping of the mouth on one side;
- Deterioration or loss of taste on the tip and sides of the tongue;
- Wide eyelid and lagophthalmos when closing the eye;
- Leakage of food from the mouth on the affected side of the face;
- Inability to stretch lips;
- In the first days of illness, noise phobia is present;
- lacrimation;
- Inability to wrinkle forehead;
- Facial asymmetry of varying degrees;
- Pain in the area behind the ear.
If these symptoms are detected, you should consult a neurologist.
Symptoms
Problems with muscle tone in newborns are clearly visible. The face is deformed on one side or both. The ear or the tissue around it may hurt. There is constant tearing or drying of the eye. It is difficult for the child to breastfeed, he does not want to eat, milk flows out of the mouth.
Sensitivity to loud sounds increases and tearfulness in the newborn increases. The eyes are wide open, and lagophthalmos appears in the affected area.
Acute symptoms are diagnosed within 2 weeks. The subacute phase lasts for a month. Then the disorder becomes chronic if left untreated.
Therapy
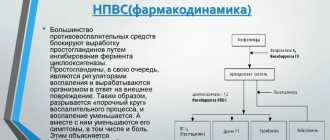
Facial nerve paresis requires a long course of treatment, which lasts about six months. It includes:
- Analgesics;
- Decongestants;
- Corticosteroids;
- Vasodilators;
- Sedatives;
- Vitamin and mineral complexes with a high content of B vitamins;
- If the eyes are affected, use artificial tears;
- Massage;
- Physiotherapy;
- Physiotherapeutic procedures.
If the nerve is completely severed, surgery is necessary.
Diagnostics
We list the common methods:
- Primary testing is for the ability to smile, wince, sucking function, use of lips in a calm state or during a cry.
- Consultation with other doctors is carried out in order to exclude the development of neoplasms and various pathologies.
- Electromyography allows you to determine the speed of passage of a nerve signal.
- CT scan.
- An MRI helps rule out possible brain damage.
What types of wounds are there?
A wound is a tissue damage that is characterized by a violation of the integrity of the skin or mucous membranes. The wound is accompanied by pain and bleeding.
The first sign is pain. It occurs due to damage to local nerve endings, and subsequently due to swelling, which puts pressure on the nerve and irritates it. In this case, pain can spread not only along the surface of the wound, but also along the damaged nerve.
The second mandatory sign of a wound is bleeding. It occurs as a result of damage to capillaries, veins or arteries. Bleeding can be weak and drip, for example, with a small cut, and severe when the integrity of the vein and artery is damaged.
The third sign of a wound is gaping. However, gaping appears only with deep wounds, for example, with abrasions it does not exist. Gaping is the divergence of the edges of the wound on either side of the axis of the cut. If there is severe gaping, the wound is usually sutured.
There are many types of wounds. For a person in everyday life, it is necessary to know several classifications. The first is based on whether there is an infection in the wound. Wounds may be aseptic, contaminated, or infected.
An aseptic wound is a pure injury to the skin. Usually these are surgical wounds that are performed in order to penetrate the internal organs. Children most often experience contaminated wounds. This means that microbes have entered the area of skin damage. At first, these are relatively safe wounds: local protective mechanisms inhibit the development of microorganisms. If a contaminated wound is not treated, it becomes infected: an infectious process develops, which is accompanied by inflammation, severe pain and suppuration. An infected wound can cause a strong reaction in the child’s body: body temperature rises, chills, drowsiness and apathy appear.
Depending on the nature of the damage, there are the following wounds:
- punctured - they occur when punctured by a narrow and piercing object, for example, when a child falls on a nail. Typically, a puncture wound bleeds slightly and hurts. Outwardly it may seem that this is a safe wound, but this is not so: large vessels, nerves are often damaged, and even an infection occurs;
- cut - occur upon contact with a sharp oblong object: a knife, razor, sharp scissors, a shard of glass and paper. With an incised wound, the tissue is usually slightly damaged. The wound bleeds heavily and hurts moderately;
- Chopped wounds occur when damaged by a heavy sharp object, such as an ax. Usually the bleeding is moderate, but the wound is very painful and gapes. May lead to serious condition;
- a bruise wound appears when struck with a blunt object or falling on asphalt. Most often, the bruised wound is located on the head, elbows and knees. The edges of a bruised wound are uneven and soaked in blood. It bleeds slightly and is moderately painful.
There are also bite wounds that occur when children are bitten by animals or other children. The difficulty with this wound is that in most cases it contains infection from the animal's oral cavity. This is how rabies, insect and snake poison, and putrefactive infection are transmitted.
The wound process consists of several stages:
- In the first seconds after skin damage, local blood vessels reflexively constrict and biologically active substances are produced - platelets, which adhere to the wound area and close the damaged vessel. The blood clotting system turns on, stopping the bleeding. In a healthy child, bleeding stops on its own within 15 minutes.
- Inflammation. Lasts 3 days from the moment of injury. Inflammation is manifested by pain, redness and local fever. Also, swelling in the form of a tumor appears on the wound within two hours.
- 2–4 hours after injury, leukocytes migrate to the area of injury. They absorb foreign particles and cleanse the wound of microorganisms.
- Healing phase. Begins 3–5 days after injury. Bioactive substances arrive to damaged tissues, which restore vascular and skin tissue.
- Epithelization phase. Begins 2 weeks after injury. The wound mark becomes pale and a scar forms. The epithelialization phase may be delayed if bacteria are present in the wound.
Forecast
In newborns, the disease develops favorably, and there are no complications if treated in a timely manner. Mild paresis is eliminated without intervention. To avoid the occurrence of contractures, after diagnosis you need to engage in therapy and follow all the doctor’s instructions.
Caring for a newborn contributes to his recovery, improving the functionality of the muscle responsible for facial expressions. Developing disease is rarely diagnosed. Isolation and tension of the tissues, in which the corner of the mouth is directed downward, indicates the presence of pathology.
Massage procedures gymnastics
Specially developed massage techniques make it possible to strengthen the muscles on the face and increase their tone. You can press your finger on the baby's lips when he pulls them into a tube. If you touch the cheeks near the mouth, the baby will begin to move his lips to feel the mother's breast. Thus, the muscle tissue will be strengthened.
Massage procedures help increase tone and improve the conductivity of nerve fibers. It is necessary that all manipulations are carried out with moderate force, the direction of massage should correspond to the treatment of lymph, the location of the lymph nodes has an undesirable effect on the skin. It is necessary to stroke the neck muscles without touching the spine.
Having entrusted such manipulations to a specialist, after some time you can carry out a massage at home, following all the instructions. To get the desired result, massage must be performed regularly at least once a day.
Prevention
It is necessary to register with the antenatal clinic to determine possible circumstances and the nature of the destruction. If there is a possibility of complications, you can prepare and reduce the risk of negative consequences. Prevention is carried out even during childbirth, if it occurs through natural channels.
The girl needs to avoid the effects of infections on the body; after the birth of the baby, she needs to pay a lot of attention to them, to prevent hypothermia or inflammation. A child develops otitis media; the disease must be diagnosed and treated in time.
If you follow all preventive recommendations, the likelihood of developing paresis will be reduced. The possibility of illness must be prevented after childbirth. When the first signs appear, you need to go to the doctor; if you try to help the child on your own, health problems may arise.
Parents are not able to determine the disease based on external symptoms. To accurately make a diagnosis, you need to conduct several examinations using special medical equipment. Doctors often make a diagnosis after childbirth if paresis occurs due to abnormal formation of nerve fibers. Even with an external examination, it is possible to identify diseases. In some situations, electroneuromyography is performed.
Treatment recommendations
To cope with such paresis, you need to contact a specialist as soon as possible. The doctor will conduct an accurate diagnosis, give some advice, and help cope with the symptoms.
Here are the recommendations:
- It is necessary to protect damaged areas under the influence of input. There should be no draft in the room where the baby is. During walks you will have to cover your face with a cloth.
- The room where the child is located should not be noisy. It is not advisable to use rattles or shout during entertainment.
- If the cause of the cut is some kind of pathology, you need to treat it.