What is intercostal neuralgia?
Let's start with the fact that intercostal neuralgia is not a disease.
This is the name for pain that occurs when the intercostal nerves are exposed to various pathological factors, for example, herpetic infection, tumors, injuries, disc herniation, protrusion, osteochondrosis, etc. In other words, thoracic intercostal neuralgia can be called not all chest pain, but only that where intercostal nerves are involved. And this needs to be clearly understood so that the confusion that you often encounter at the everyday level does not arise when you hear people using the term intercostal neuralgia, but at the same time they mean a completely different pathology. By the way, even some doctors sometimes make the diagnosis of intercostal neuralgia erroneously, while in reality it most often turns out to be myofascial syndrome. Intercostal neuralgia, myalgia, myositis, myofascial syndrome, osteochondrosis, disc herniation, protrusion and many other terms are not synonymous. These are the names of specific pathologies that have their own characteristics and differences. And, since they are different, it means that the approach to them must also be different, otherwise there will be no sense in the treatment.
In general, the term intercostal neuralgia should not be used haphazardly, and it is not worth calling all pain in this area that way.
Localization of pain
- Referred pain. Referred pain, as a rule, is a consequence of the development of a pathological process in the internal organs (diseases of the retroperitoneum, aortic aneurysm, pathology of the digestive tract, coronary artery disease).
- Radiating pain. The mechanism of development of this pain has not been fully studied to date. According to experts, parts of the nervous system may misinterpret the source of pain due to the presence of common pathways through which both visceral and somatic pain are carried out. Referring pain, resulting from stretching, irritation or compression of a somatic nerve or nerve root, is more intense. With physical activity, sneezing or coughing, the pain may intensify, and can often spread to the affected area of the body.
- Local pain. Its cause can be any pathological process aimed at pain receptors of various tissues, muscles, ligaments, skin, tendons, bones, joints, etc. In this case, pain develops directly in the area of damage.
Intercostal neuralgia in women & Intercostal neuralgia in men.
Intercostal neuralgia in men occurs as often as in women, but at the same time, intercostal neuralgia in women has its own characteristics. For example, women often perceive pain due to intercostal neuralgia as a manifestation of breast disease, and not as neuralgia. And it is clear that such thoughts can only cause additional anxiety and worry. But there is one consolation - although pathology of the mammary glands is indeed common, even if it is present, the vast majority of pain is not associated with it, but with the spine, nerves and muscles. This does not cancel periodic examinations with a mammologist, but it does mean that you should never panic. And most importantly, keep in mind that in medicine there is such a concept - a disease “in disguise”, when one disease is masked by another. Let's look at the insidiousness of this problem using our example. Pathology of the mammary glands is a psychological dominant that causes much more concern than intercostal neuralgia. Accordingly, if a woman simultaneously has thoracic intercostal neuralgia and pathology of the mammary glands, then all her thoughts will be focused on the glands. The rest will fade into the background. And it is quite natural that in this situation a woman, first of all, will turn to a mammologist. If the mammologist turns out to be knowledgeable, he will quickly figure out what is causing the pain: glands or neuralgia. And, if it is neuralgia, he will refer the patient to a chiropractor. By the way, it is the chiropractor who is the main doctor for intercostal neuralgia (but we’ll talk about this later). And if a mammologist comes across an inexperienced or over-insurer, what will he do? Most likely, having discovered his own profile pathology in the patient, he will also focus on this pathology and will not “dig” deeper. Consequently, if in reality the patient was bothered by pain due to intercostal neuralgia, and the pathology of the mammary glands was only a background that did not cause pain, then treatment by a mammologist will not solve the problem. The pain will remain. And this will cause the woman even more anxiety. Her faith in doctors will suffer. Your nerves and time will be wasted. This is what the disease turns out to be “under the mask.” Meanwhile, intercostal neuralgia in women very often occurs under the guise of mammary gland pathology. Be sure to remember this!
Dear women, the best advice for pain in this area is to contact two specialists at once. A mammologist will give you confidence and relieve fears, and a chiropractor will cure intercostal neuralgia. After all, as we have already said, a chiropractor is the key doctor for intercostal neuralgia. This approach is the most reasonable. It will save you both time and nerves.
Intercostal neuralgia in men also has its own characteristics, and these are not always differences. For example, very similar psychological aspects. So, if in women intercostal neuralgia often occurs under the guise of mammary gland pathology, then in men it occurs under the guise of heart disease. By the way, it is precisely the “disguise” as heart disease that distinguishes left intercostal neuralgia from intercostal neuralgia on the right side. Do you know how to distinguish intercostal neuralgia from a heart attack at home? Very simple. Heart pain is relieved by nitroglycerin, but neuralgia is not.
According to statistics, intercostal neuralgia on the left in the heart area equally often causes a false alarm in both men and women. Moreover, in women, both the heart and the mammary gland come under suspicion. But, right intercostal neuralgia is “suspicious” only for women. Men immediately understand that this is intercostal neuralgia.
Non-drug therapy
Intercostal neuralgia can be treated without the use of medications using the following methods:
- Using massage movements of the hands with a warming ointment or cream applied to them, deep warming and relaxation of the muscles that create a protective “corset” (or, conversely, leading to compression of the intercostal nerve) is achieved. It is performed in a sitting position with rubbing and stroking the intercostal spaces with the fingertips and subsequent kneading of all the spinal muscles.
- Unlike the previous method, acupressure applies pressure to the physiologically and bioenergetically massaged chest points associated with the diseased organ, leading to pain relief, relaxation and a quick effect by stimulating the body’s own defense mechanisms.
- Similar physiologically and bioenergetically justified effects are the methods of acupuncture (acupuncture), cauterization, and laser therapy, which make it possible to quickly neutralize muscle imbalance in the deep back muscles with the elimination of pain.
- Treatment of intercostal neuralgia by placing massage cups on the back pursues the same goals, being a simple and harmless technique for the body (provided there are no contraindications to its use).
- Manual techniques are resorted to after the end of the acute period. They consist in returning to their proper places the bone structures and muscles and ligaments that serve them that have been displaced during the disease and are carried out exclusively after manual diagnosis. As a result of the impact, the diameter of the narrowed tunnels (bone-tendon and musculoskeletal) returns to normal and the function of the pinched nerve is restored.
Like all the above methods, physiotherapeutic methods using:
- magnetic or electromagnetic field;
- ultrasonic, ultraviolet and infrared radiation;
- electro- and iontophoresis, with a dose of the drug substance that is minimal for the risk of the fetus.
Symptoms of intercostal neuralgia
It is believed that the main symptom of intercostal neuralgia is pain in the intercostal space. But how can one distinguish intercostal neuralgia from one symptom, even such a striking one? After all, pain in the ribs also occurs with other pathologies. Obviously, for an accurate diagnosis, more signs of intercostal neuralgia are needed. Therefore, we decided to talk about the symptoms and causes of intercostal neuralgia in more detail.
The name intercostal nerves speaks for itself. They are actually located between the ribs. Starting from the spine, they cover the chest on both sides. The intercostal nerve cannot suffer from a small or even moderate bruise, since it is located deep under the rib. Therefore, the mechanical cause of intercostal neuralgia can be serious injuries, for example, a fracture; a tumor compressing a nerve, or dystrophic pathology of the spine - osteochondrosis, hernia and disc protrusion.
In addition to mechanical ones, there are also infectious causes of intercostal neuralgia, most often a herpetic infection. Due to its characteristics, it often affects these nerves. Herpes, as a sign of intercostal neuralgia, is easily recognized by characteristic rashes that coincide with the area of pain.
Thus, the causes of intercostal neuralgia are infectious and mechanical. But, the connection between intercostal neuralgia and breathing is a myth. Remember, at the beginning of the article we talked about the difference between real intercostal neuralgia and what many people mistakenly consider to be such. For example, the appearance of intercostal neuralgia after a cold is not neuralgia at all, but myofascial syndrome. If you are not aware, myofascial syndrome is a muscle disease in which small painful areas - trigger points - form in the muscles. These points may remain in a latent state for a long time and not manifest themselves in any way. But as soon as they are activated, pain immediately arises. The most common factor in the activation of trigger points is overload of the affected muscles. The intercostal muscles are classified as respiratory muscles, as they are involved in the act of breathing. A cough is a forced exhalation. Therefore, intercostal neuralgia when coughing or after a cold is not neuralgia, as many people mistakenly think, but myofascial syndrome, provoked by overload of the respiratory muscles from coughing. By the way, an indirect sign of how to distinguish intercostal neuralgia from myofascial syndrome is the duration of the disease. True intercostal neuralgia takes a long time to heal. Especially if it is caused by a fracture or tumor. And myofascial syndrome has a shorter treatment period. But it is impossible to say exactly how long intercostal neuralgia lasts without seeing the patient. Firstly, you need to make sure that it is intercostal neuralgia and not some other pathology, and secondly, it all depends on the situation. Agree, neuralgia from herpes and from a fracture will have completely different treatment periods.
Separately, it is necessary to say about the so-called false symptoms of intercostal neuralgia. Muscle tension, muscle twitching, increased pain when coughing, sneezing, turning the body; forced body position to relieve pain, sweating, high blood pressure and a number of other symptoms are not signs of intercostal neuralgia, although they are often attributed to it. These symptoms refer to pathologies similar to neuralgia. Being able to distinguish between similar pathologies is one of the basic skills of a doctor, which is specially taught, and which allows the doctor to make an accurate and correct diagnosis. It remains only to remind you that a doctor for intercostal neuralgia is a chiropractor, or even better, a chiropractor-neurologist.
Diagnostics
After the doctor has collected the patient’s complaints and history of the development of the disease, additional examinations must be carried out to confirm the diagnosis.
The most informative and used of them:
- Chest X-ray - reveals disturbances in the structure of bone tissue, as the main cause of the development of neuralgia;
- Bacteriological blood test - if the cause of thoracalgia is an infection, it reveals the causative agent of the disease, in other cases the analysis remains unchanged;
- Complete blood count - normal values are typical, or a slight increase in leukocytes in the case of an inflammatory reaction in the nerve area;
- Magnetic resonance imaging - determines bone and cartilage changes, swelling, pinching or inflammation of the intercostal nerve;
- Computed tomography is a more accurate method compared to x-rays; it reveals smaller abnormalities in the structure of bone tissue;
- Ultrasound – used to differentiate neuralgia from other pathologies, with thoracalgia it remains unchanged;
- Electrospondylography – determines the pathology of the intervertebral discs and spine;
- Myelography - the spinal cord and intercostal nerves are examined using a contrast agent on an X-ray machine, and allows you to identify changes in the nervous tissue;
- Electromyography - determines abnormalities in muscle fibers along the affected nerve.
Treatment of intercostal neuralgia
Treatment for intercostal neuralgia depends on what causes it. Statistics say that the vast majority of pain in this area is caused by mechanical causes - pathology of the spine and muscles - osteochondrosis, disc herniation, protrusion, myalgia and myofascial syndrome. Therefore, the answer to the question of how to treat intercostal neuralgia is obvious. Since most of the reasons are mechanical, then they should be eliminated mechanically. This means that the best way to treat thoracic intercostal neuralgia is manual therapy. Moreover, not ordinary, but soft manual therapy, which is not only softer, but also much more effective than simple realignment of the vertebrae. Gentle manual therapy works extremely gently and delicately. Its main advantage is the safe elimination of muscle tension that “pinches” the nerve and stiffens the spine. This is why a chiropractor is the primary physician for intercostal neuralgia. In cases where the problem is advanced, manual therapy can be supplemented with medications and physical therapy.
Treatment of intercostal neuralgia with herpetic lesions requires parallel treatment by a dermatologist. Rare and severe forms caused by fractures and tumors require high-tech and expensive medical care, which is carried out under government programs in specialized clinics.
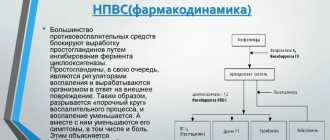
How to relieve pain from intercostal neuralgia if a person finds himself far from full-fledged medicine and only a pharmacy nearby? Pain in acute intercostal neuralgia is best relieved with the combined use of non-steroidal and steroidal anti-inflammatory drugs. But, we draw your attention - see a specialist as soon as possible. This must be done even if the pain stops completely. It is in your best interests to be sure that nothing more serious lies behind the pain and intercostal neuralgia.
Exercises
Physical therapy (physical therapy) is an effective way to treat neuralgia due to the anatomical structure of the human body. The nerves are located in the grooves of the ribs, which are covered by muscles. Spasmed muscles put pressure on nerve trunks, which causes pain. Exercises relax the muscles of the back and chest, improve blood circulation, and as a result the pain goes away. Gymnastics are prescribed only after acute pain has been relieved.
When performing physical exercises, you must consider some rules:
- Classes begin with a light warm-up - the body should be warmed up.
- The load must be increased gradually.
- You can't exercise through pain.
- Movements should be careful and smooth.
- Exercises should be aimed at strengthening the back muscles and stretching the spine.
- When performing exercises, you need to relax your back muscles as much as possible.
- You need to study every day, without skipping.
Gymnastics using the method of Dr. Bubnovsky is very effective. The essence of his technique: no medications, the medicine will be exercises, including those performed on special simulators. These exercises increase blood circulation and relax the deepest muscles.
Causes
Intercostal neuralgia can be caused by various reasons. Basic:
- Poor posture, injuries, intervertebral hernias, osteochondrosis.
- Hypothermia, which led to poor circulation.
- Infectious and other diseases that lead to nerve damage. For example, destruction of the nerve sheath in multiple sclerosis.
- Neoplasms that compress nerve roots.
- Muscle spasms, prolonged tension during sudden movements or prolonged uncomfortable body posture.
- Operations.
- Pathologies of internal organs.