Tunnel neuropathies account for 1/3 of diseases of the peripheral nervous system. More than 30 forms of tunnel neuropathies have been described in the literature [Levin O.S., 2005]. Various forms of compression-ischemic neuropathies have their own characteristics. We will first consider their general characteristics, then we will focus on the most common forms of hand tunnel syndromes (Table 1).
Causes
The anatomical narrowness of the canal is only a predisposing factor in the development of tunnel syndrome. In recent years, evidence has accumulated indicating that this anatomical feature is genetically determined. Another reason that can lead to the development of tunnel syndrome is the presence of congenital developmental anomalies in the form of additional fibrous cords, muscles and tendons, and rudimentary bone spurs. However, predisposing factors alone for the development of this disease are usually not enough. Some metabolic and endocrine diseases (diabetes mellitus, acromegaly, hypothyroidism), diseases accompanied by changes in joints, bone tissue and tendons (rheumatoid arthritis, rheumatism, gout), conditions accompanied by hormonal changes (pregnancy), space-occupying formations can contribute to the development of tunnel syndrome the nerve itself (schwannoma, neuroma) and outside the nerve (hemangioma, lipoma). The development of tunnel syndromes is facilitated by frequently repeated stereotypical movements and injuries. Therefore, the prevalence of carpal tunnel syndrome is significantly higher in people engaged in certain activities and in representatives of certain professions (for example, stenographers have carpal tunnel syndrome 3 times more often).
Clinical manifestations
The full picture of tunnel syndrome includes sensory (pain, paresthesia, numbness), motor (decreased function, weakness, atrophy) and trophic disorders.
Various clinical course options are possible. Most often it starts with pain or other sensory disorders. Less commonly, it begins with movement disorders. Trophic changes are usually expressed insignificantly and only in advanced cases. The most characteristic feature of carpal tunnel syndrome is pain. Typically, pain appears during movement (load), then occurs at rest. Sometimes the pain wakes the patient up at night, which exhausts the patient and forces him to see a doctor. Pain in tunnel syndromes can include both a nociceptive component (pain caused by inflammatory changes occurring in the area of the nerve-canal conflict) and a neuropathic component (due to nerve damage). Tunnel syndromes are characterized by manifestations of neuropathic pain such as allodynia and hyperpathy, a sensation of electric current passing (electrical shooting), and burning pain. In later stages, pain may be due to muscle spasms. Therefore, when choosing pain therapy, it is necessary to be guided by the results of a thorough clinical analysis of the characteristics of the pain syndrome. Motor disorders arise as a result of damage to the motor branches of the nerve and manifest themselves in the form of decreased strength and rapid fatigue. In some cases, the progression of the disease leads to atrophy and the development of contractures (“clawed paw”, “monkey paw”).
With compression of arteries and veins, vascular disorders may develop, which is manifested by pallor, a decrease in local temperature, or the appearance of cyanosis and swelling in the affected area. With isolated nerve damage (in the absence of compression of arteries and veins), trophic changes are most often insignificantly expressed.
Treatment of damage to the radial, ulnar and median nerves at the Echinacea clinic
When it is clear where, how and why nerve compression occurs, local treatment in the form of physiotherapy, therapeutic blockades, massage, and manual therapy becomes much more effective. Therefore, treatment in our clinic begins with finding out the cause and location of nerve damage .
The main goals of treatment for nerve compression:
- Remove nerve compression. To do this, we use powerful resorption therapy: we use enzymes that resolve and soften scar tissue, bone and cartilage growths (Karipazim enzyme, etc.), massage, and injecting medications directly into the site of nerve compression. Sometimes, to release the nerve, manual therapy and massage of the areas of compression of the ulnar, median and radial nerves (cervical spine, elbow, wrist joints, etc.) are sufficient.
- Accelerate healing and restoration of the nerve. To do this, we use modern medications that help restore the nerve freed from compression and scarring.
- Restore muscle function and volume. Special exercises, electrical stimulation of muscles, and physiotherapy are used here. The rehabilitator will tell you in detail and show you how to perform rehabilitation procedures at home.
Diagnostics
As a rule, the diagnosis is established on the basis of the characteristic clinical manifestations described above. It is convenient for the clinician to use a number of clinical tests that allow differentiating different types of carpal tunnel syndromes. In some cases, it is necessary to conduct electroneuromyography (the speed of impulses along the nerve) to clarify the level of nerve damage. Nerve damage, space-occupying lesions or other pathological changes causing carpal tunnel syndrome can also be determined using ultrasound, thermal imaging, MRI [Horch RE et al., 1997].
Diagnosis of tunnel syndromes
Diagnosis of carpal tunnel syndrome begins with collecting a medical history and examining the patient by a doctor. To record the localization of paresthesia, the patient fills out a hand diagram on which he schematically marks the areas in which there is a sensation of tingling, numbness or pain.
There are quite informative tests that allow you to diagnose CTS: Tinel test, Durkan test, Phalen test, opposition test [3]. Electromyography is prescribed to evaluate nerve conduction. Ultrasound examination helps determine the size of the median nerve, the presence and nature of pathological changes in the tissues around the nerve. If there is swelling of the median nerve, narrowing of the carpal tunnel, or impaired blood circulation, an MRI is indicated for the patient. To assess the general condition of the body and the presence of chronic diseases, the doctor may prescribe blood tests and examination of other organs and systems.
Stop exposure to the pathogenic factor. Immobilization
The first thing to do is to stop physical impact on the affected area. Therefore, immobilization in the affected area is necessary. Recently, special devices have appeared in our country - orthoses, bandages, splints, which allow immobilization in the area of injury. At the same time, they are very convenient to use, they can be put on and taken off very easily, which allows the patient to maintain his social activity (Fig. 1). These funds are widely and successfully used abroad. Studies have appeared on the effectiveness of splinting, which have convincingly shown that it is quite comparable to the effectiveness of hormone injections and surgical operations. In our country, these devices are already used by traumatologists; They are clearly not yet sufficiently introduced into neurological practice.
Change the usual locomotor stereotype and lifestyle
Tunnel syndromes are often the result not only of monotonous activity, but also of ergonomic disorders (improper posture, awkward position of the limb during work). Special exercises and recommendations for optimal organization of the workplace have been developed. To relieve pain and prevent relapse, orthoses and splints using the splinting principle are used. In rare cases, you have to change your profession. Training in special exercises and physical therapy are an important component of the treatment of tunnel neuropathies at the final stage of therapy.
Pain therapy
Physical influences (cold, heat).
In mild cases, ice compresses and sometimes “hot” compresses can help reduce pain. A doctor is usually consulted when these or other “home” methods “do not help.” • Anti-inflammatory therapy. Traditionally, for carpal tunnel syndromes, NSAIDs with a more pronounced analgesic and anti-inflammatory effect (diclofenac, ibuprofen) are used. It should be remembered that with long-term use of drugs in this group there is a risk of gastrointestinal and cardiovascular complications. In this regard, for moderate or severe pain, it is advisable to use a combination of low doses of the opioid analgesic tramadol (37.5 mg) and the safest analgesic/antipyretic paracetamol (325 mg). Thanks to this combination, a multiple increase in the general analgesic effect is achieved with a lower risk of side effects.
• Impact on the neuropathic component of pain. Often, with tunnel syndromes, the use of analgesics and NSAIDs is ineffective (it is in these cases that patients consult a doctor). This may be due to the fact that the dominant role in the formation of pain is played not by the nociceptive, but by the neuropathic mechanism. When pain is the result of neuropathic changes, it is necessary to prescribe drugs recommended for the treatment of neuropathic pain: anticonvulsants (pregabalin, gabapentin), antidepressants (venlafaxine, duloxetine), plates with 5% lidocaine. The choice of a particular drug should be made taking into account the clinical manifestations and individual characteristics of the patient (the possibility of developing side effects). It is important to inform the patient that drugs used for neuropathic pain, unlike “classical painkillers,” do not begin to act immediately (it is necessary to titrate the dose; the effect occurs several days or even weeks after starting the drug).
• Injections of anesthetic + hormones. A very effective and acceptable treatment method for most types of tunnel neuropathies is a blockade with the introduction of an anesthetic (Novocaine) and a hormone (hydrocortisone) into the area of infringement. Special guidelines describe techniques and doses of drugs for various tunnel syndromes [Zhulev N.M., 2005]. This procedure is usually resorted to if other measures are ineffective (cold compresses, the use of analgesics, NSAIDs), but in some cases, if the patient comes at a more advanced stage of the disease and experiences severe pain, it is advisable to immediately offer such a patient this manipulation.
• Other methods of pain relief. Currently, there are reports of the high effectiveness of injection of meloxicam with hydrocortisone into the tunnel area. An effective way to reduce pain and inflammation is electrophoresis, phonophoresis with dimexide and other anesthetics. They can be carried out in a clinic setting. Symptomatic treatment. For tunnel syndromes, decongestants, antioxidants, muscle relaxants, and drugs that improve the trophism and functioning of the nerve (ipidacrine, vitamins, etc.) are also used.
Surgical intervention. Surgical treatment is usually resorted to when other options for helping the patient have been exhausted. At the same time, for certain indications, it is advisable to immediately offer the patient surgical intervention. Surgery usually involves releasing the nerve from compression, “reconstructing the tunnel.” According to statistics, the effectiveness of surgical and conservative treatment does not differ significantly a year later (after the start of treatment or surgery). Therefore, after a successful surgical operation, it is important to remember about other measures that must be followed to achieve a full recovery (prevention of relapses): changing locomotor patterns, using devices that protect against stress (orthoses, splints, bandages), performing special exercises.
Carpal tunnel syndrome - how to reduce pain?
Class Clinic
Who is more susceptible to carpal tunnel syndrome - women or men, young or elderly? What professions are at risk? Which modern treatment methods are most effective? Tatyana Borisovna Avdeeva, a practicing neurologist at the Kaliningrad medical center Class Clinic, spoke about tunnel syndromes and the peculiarities of using local injections in their treatment.
What is carpal tunnel syndrome and how does it manifest?
Tunnel syndromes are a group of diseases that occur when nerves are compressed by bones, muscles and tendons. The most common symptoms are numbness in the area innervated by the compressed nerve and prolonged, intermittent pain. Often, tunnel syndrome is understood only as carpal tunnel syndrome (carpal syndrome), when compression of the median nerve occurs between the bones, tendons of the wrist and the transverse carpal ligament. This is not entirely true, since this is only a special case of the disease.
Is carpal tunnel syndrome really a disease of programmers and office workers, or is this opinion wrong?
Almost everyone is at risk, since there are a huge number of carpal tunnel syndromes, but carpal syndrome, which is talked about in this case, more often actually occurs from working at a computer. Meanwhile, it occurs no less often in athletes, drivers, milkmaids and representatives of any other professions where chronic injury in the wrist joint is possible.
In my practice, there was a case when carpal tunnel syndrome developed in a patient who, due to his occupation, constantly carried water in twenty-liter bottles and practically did not work at the keyboard. We can say that representatives of any profession where it is necessary to regularly repeat the same type of actions are at risk.
Is local injection therapy (blockades) used for this disease?
The main manifestations of carpal tunnel syndrome are pain and numbness, and in severe, advanced cases - paralysis and muscle atrophy. In this disease, the nerve is compressed in the canal, as a rule, this is caused by local tissue swelling due to chronic injury. With such mechanisms and symptoms, it is really effective to use local injection blockades as one of the methods of complex therapy.
In what cases is local injection therapy indicated for tunnel syndromes and what drugs are used?
Almost all, if there are no contraindications - concomitant infectious or oncological processes. In case of tunnel syndromes, blockades can be used not only as a symptomatic method of relieving intense pain, but also as a pathogenetic treatment, since by relieving swelling, we relieve nerves from compression. Thus, with the help of local injection therapy, we can influence the mechanism of disease development, while obtaining a long-term and fairly stable result.
Glucocorticosteroid hormonal drugs are also used, which, in combination with or without local anesthetics, lead to a reduction in edema and stop compression of the nerve. Nonsteroidal anti-inflammatory drugs may also be used. In such cases, we quickly get results; the effects of local injection therapy appear the very next day: pain disappears, sensitivity and normal mobility are later restored.
Is it possible to treat carpal tunnel syndrome solely with blockades?
It is difficult to guarantee complete recovery using only blockades. It is always necessary for the patient to participate in treatment, adherence to a certain work schedule, position of the affected limb, reduction of stress and other recommendations of the neurologist. Sometimes local injection therapy is used as an emergency method to restore performance. It can also be used as a method of minimally invasive pathogenetic treatment, but only in cases where the degree of pain of the process allows this. There are cases when it is impossible to cope with carpal tunnel syndrome other than surgery.
It should be remembered that the result (especially in the early stages of the development of this disease) largely depends on the implementation of the neurologist’s recommendations. Injection blockades will certainly bring relief. But without proper occupational hygiene, improvements will be temporary and the process of re-traumatization will again lead to deterioration. That is why you should not consider local injection therapy as a guaranteed method of getting rid of carpal tunnel syndrome. This disease must be treated comprehensively.
Make an appointment with Tatyana Borisovna Avdeeva on the website or by phone (4012) 33-44-55. When you register on the website, there is a 20% discount on your initial appointment.
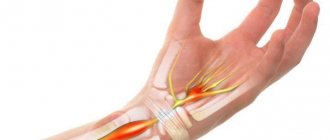
Carpal tunnel syndrome
Carpal tunnel syndrome (carpal tunnel syndrome) is the most common form of compression-ischemic neuropathy encountered in clinical practice. In the population, carpal tunnel syndrome occurs in 3% of women and 2% of men [Berzins Yu.E., 1989]. This syndrome is caused by compression of the median nerve as it passes through the carpal tunnel under the transverse carpal ligament. The exact cause of carpal tunnel syndrome is not known. The following factors most often contribute to compression of the median nerve in the wrist area: • Trauma (accompanied by local swelling, tendon stretching). • Ergonomic factors. Chronic microtraumatization (often found among construction workers), microtraumatization associated with frequent repeated movements (among typists, with constant long-term work with a computer). • Diseases and conditions accompanied by metabolic disorders, edema, tendon and bone deformities (rheumatoid arthritis, diabetes mellitus, hypothyroidism, acromegaly, amyloidosis, pregnancy). • Massive formations of the median nerve itself (neurofibroma, schwannoma) or outside it in the wrist area (hemangioma, lipoma).
Clinical manifestations
Carpal tunnel syndrome is characterized by pain, numbness, paresthesia and weakness in the arm and hand.
Pain and numbness extend to the palmar surface of the thumb, index, middle and 1/2 ring finger, as well as to the dorsum of the index and middle finger. Initially, symptoms occur when performing any activities using a brush (working on a computer, drawing, driving), then numbness and pain appear at rest, sometimes occurring at night. The following tests are suggested to verify the diagnosis of carpal tunnel syndrome. Tinel test: tapping the wrist (above the median nerve) with a neurological hammer causes a tingling sensation in the fingers or pain radiating (electrical shooting) to the fingers (Fig. 2). Pain may also be felt in the tapping area. A positive Tinel sign is found in 26–73% of patients with carpal tunnel syndrome [Al Zamil M.H., 2008]. Durkan's test: compression of the wrist in the area of the median nerve causes numbness and/or pain in the 1st–3rd, half of the 4th fingers (as with Tinel's symptom). Phalen Test: Wrist flexion (or extension) 90 degrees produces numbness, tingling, or pain in less than 60 seconds (Figure 3). A healthy person may also develop similar sensations, but not earlier than after 1 minute. Opposition test: with severe thenar weakness (which occurs at a later stage), the patient cannot connect the thumb and little finger (Fig. 4); or the doctor (researcher) can easily separate the patient’s closed thumb and little finger.
Differential diagnosis
Carpal tunnel syndrome should be differentiated from arthritis of the carpo-metacarpal joint of the thumb, cervical radiculopathy, and diabetic polyneuropathy. Patients with arthritis will show characteristic bone changes on x-rays. In cervical radiculopathy, reflex, sensory and motor changes will be associated with neck pain, while in carpal tunnel syndrome these changes are limited to distal manifestations. Diabetic polyneuropathy is usually a bilateral, symmetrical process involving other nerves (not just the median nerve). At the same time, a combination of polyneuropathy and carpal tunnel syndrome in diabetes mellitus cannot be ruled out.
Treatment
In mild cases of carpal tunnel syndrome, ice compresses and a decrease in load can help. If this does not help, the following measures must be taken: 1. Immobilization of the wrist. There are special devices (splints, orthoses) that immobilize the wrist and are convenient to use (Fig. 1). Immobilization should be carried out at least overnight, and preferably for 24 hours (at least in the acute period). 2. NSAIDs. Drugs from the NSAID group will be effective if the inflammatory process dominates in the pain mechanism. 3. If the use of NSAIDs turns out to be ineffective, it is advisable to inject novocaine with hydrocortisone into the wrist area. As a rule, this procedure is very effective. 4. In outpatient settings, electrophoresis can be performed with anesthetics and corticosteroids. 5. Surgical treatment. For mild or moderate carpal tunnel syndrome, conservative treatment is more effective. In cases where all conservative treatment options have been exhausted, surgical treatment is resorted to. Surgical treatment consists of partial or complete resection of the transverse ligament and releasing the median nerve from compression. Recently, endoscopic surgical methods have been successfully used in the treatment of carpal syndrome.
Treatment of symptoms of ulnar neuritis
For symptoms of ulnar nerve neuritis, a neurologist prescribes treatment, which may include medications, physiotherapy, massage, and physical therapy.
Sometimes they resort to acupuncture
In severe cases, surgery may be required. The surgeon frees the ulnar nerve from pathologically altered tissues that compress it, or sews the ends together if its integrity is compromised.
The sooner you contact a competent doctor, the sooner the correct treatment will be prescribed, and the restoration of impaired functions will occur more quickly and fully. Make an appointment with a specialist right now: +7 (495) 230-00-01.
The material was prepared by Natalya Yurievna, a neurologist at the international clinic Medica24, Candidate of Medical Sciences Lasch.
Pronator teres syndrome (Seyfarth syndrome)
Entrapment of the median nerve in the proximal part of the forearm between the pronator teres fascicles is called pronator syndrome.
This syndrome usually begins to appear after significant muscle activity over many hours involving the pronator and flexor digitorum muscles. Such types of activities are often found among musicians (pianists, violinists, flutists, and especially often among guitarists), dentists, and athletes [Zhulev N.M., 2005]. Long-term tissue compression is of great importance in the development of pronator teres syndrome. This can happen, for example, during deep sleep when the newlywed’s head is positioned for a long time on the partner’s forearm or shoulder. In this case, the median nerve in the pronator snuffbox is compressed, or the radial nerve in the spiral canal is compressed when the partner’s head is located on the outer surface of the shoulder (see radial nerve compression syndrome at the level of the middle third of the shoulder). In this regard, to designate this syndrome in foreign literature, the terms “honeymoon paralysis” (honeymoon paralysis, newlywed paralysis) and “lovers paralysis” (lovers paralysis) have been adopted. Pronator teres syndrome sometimes occurs in nursing mothers. In them, compression of the nerve in the area of the pronator teres occurs when the baby’s head lies on the forearm, he is breastfed, lulled to sleep, and the sleeping person is left in this position for a long time.
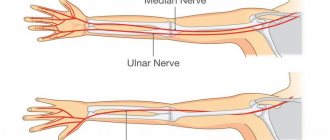
Anatomy
The ulnar nerve originates from the lower part of the brachial plexus. The brachial plexus begins in the lower part of the neck from the anterior branches of the spinal nerves at the level of C5 - C8. Spinal nerves exit the spinal canal through small openings between the cervical vertebrae at the C5 – Th1 level.
It is believed that the spinal nerves at the C7-C8 level participate in the formation of the ulnar nerve. Nerve fibers, intertwining with fibers of other spinal nerves, form the brachial plexus, and then, leaving the plexuses, form nerves. The ulnar nerve is one of the major nerves of the brachial plexus. The ulnar nerve emerges from the axilla, following as part of the neurovascular bundle. Approximately in the middle of the shoulder, the nerve branches off from the brachial artery to the internal intermuscular septum. In the lower part of the shoulder, the nerve passes along the posterior surface of the internal epicondyle of the shoulder. On the posterior surface of the internal epicondyle of the shoulder there is a special bone groove for the ulnar nerve. This is where the ulnar nerve can become pinched. If you straighten your arm, you can feel this groove medially from the olecranon process. If this area of the elbow joint is injured, then lumbago is felt going to the 4-5 fingers of the hand.
Coming out of the groove, the nerve follows in the thickness of the muscles of the inner side of the forearm, being responsible for their innervation; it innervates the skin of the inner side of the forearm and the 4th and 5th fingers, as well as small muscles of the hand. {banner_st-d-1}
Clinical manifestations
With the development of pronator teres syndrome, the patient complains of pain and burning 4–5 cm below the elbow joint, along the anterior surface of the forearm and pain radiating to the 1st–4th fingers and palm.
Tinel's syndrome. In case of pronator teres syndrome, Tinel's sign will be positive when tapping with a neurological hammer in the area of the pronator snuff box (on the inside of the forearm). Pronator-flexor test. Pronating the forearm with a tightly clenched fist while creating resistance to this movement (counteraction) leads to increased pain. Increased pain can also be observed when writing (prototype of this test). When examining sensitivity, a sensitivity disorder is revealed, involving the palmar surface of the first three and a half fingers and the palm. The sensory branch of the median nerve, innervating the palmar surface of the hand, usually passes above the transverse carpal ligament. The occurrence of sensory disturbances on the palmar surface of the first finger, the dorsal and palmar surfaces of the second and fourth fingers, with preservation of sensitivity in the palm, allows one to confidently differentiate carpal tunnel syndrome from pronator teres syndrome. Thenar atrophy in pronator teres syndrome is usually not as severe as in progressive carpal tunnel syndromes.
Supracondylar process syndrome of the shoulder (Strother's band syndrome, Coulomb, Lord and Bedossier syndrome)
In the population, in 0.5–1% of cases, a variant of the development of the humerus is observed, in which a “spur” or supracondylar process (apophysis) is found on its distal anteromedial surface. Due to the accessory process, the median nerve is displaced and stretched (like a bowstring). This makes him vulnerable to defeat. This tunnel syndrome, described in 1963 by Coulomb, Lord and Bedossier, has almost complete similarities with the clinical manifestations of pronator teres syndrome: pain, paresthesia, and decreased flexion strength of the hand and fingers are detected in the zone of innervation of the median nerve. In contrast to pronator teres syndrome, when the median nerve is damaged under Strather's ligament, mechanical compression of the brachial artery with corresponding vascular disorders is possible, as well as severe weakness of the pronator teres (teres and minor). The following test is useful in diagnosing supracondylar process syndrome. When extending the forearm and pronation in combination with formed flexion of the fingers, painful sensations are provoked with localization characteristic of compression of the median nerve. If it is suspected that the compression is caused by a “spur” of the humerus, an x-ray examination is indicated. Treatment involves resection of the supracondylar process (“spur”) of the humerus and ligament.
Cubital tunnel syndrome
Cubital tunnel syndrome (Sulcus Ulnaris Syndrome) is compression of the ulnar nerve in the cubital canal (Mouchet's canal) in the area of the elbow joint between the internal epicondyle of the humerus and the ulna bone and is the second most common after carpal tunnel syndrome. Cubital tunnel syndrome develops for a number of reasons. Cubital tunnel syndrome can be caused by repetitive bending of the elbow joint. Therefore, cubital tunnel syndrome is classified as a disorder called accumulated trauma disorder (overuse syndrome). Those. the disorder may occur during normal, repetitive movements (most often associated with a specific occupational activity) in the absence of obvious traumatic injury. Direct trauma can also contribute to the development of cubital tunnel syndrome, such as leaning on the elbow while sitting. Patients with diabetes and alcoholism are at greater risk of developing cubital tunnel syndrome.
Prices for treatment of ulnar nerve tunnel syndrome
Specialist consultations
| Primary appointment (examination, consultation) with a surgeon | 1 500₽ |
| Repeated appointment (examination, consultation) with a surgeon | 1 500₽ |
In Romanyutina N.S. consultation is free until September 30, 2021.
Ulnar nerve tunnel syndrome
| Ligamentotomy for cubital tunnel syndrome | 150 000₽ |
| Neurolysis, decompression of nerves in carpal tunnel syndrome | 130 000₽ |
| Relocation of the ulnar nerve in cubital tunnel syndrome with increased mobility of the ulnar nerve | 180 000₽ |
Anesthesia
| Local anesthesia | 5 000₽ |
| Intravenous anesthesia (IVVA) | 20 000₽ |
| General anesthesia (GENA). The cost depends on the duration of the operation (from 2 to 8 hours) | from 30,000₽ to 40,000₽ |
Hospital stay
| Stay of patients in the ward after general anesthesia (1 day) | 10 000₽ |
| Patients' stay in the ward after intravenous anesthesia (day) | 5 000₽ |
View full price list
Clinical manifestations
The main symptoms of cubital tunnel syndrome are pain, numbness and/or tingling. Pain and paresthesia are felt in the lateral part of the shoulder and radiate to the little finger and half of the fourth finger. At first, discomfort and pain occur only when pressure is applied to the elbow or after prolonged bending. In a more severe stage, pain and numbness are felt constantly. Another sign of the disease is weakness in the arm. It manifests itself as a loss of “confidence” in the hand: suddenly objects begin to fall out of it during some habitual actions. For example, it becomes difficult for a person to pour water from a kettle. In advanced stages, the hand on the sore arm begins to lose weight, and pits appear between the bones due to muscle atrophy.
Diagnostics
In the early stages of the disease, the only manifestation (besides weakness of the forearm muscles) may be loss of sensation on the ulnar side of the little finger. If the clinical picture is blurred, the following tests can help verify the diagnosis of Cubital Tunnel Syndrome: Tinel test - the occurrence of pain in the lateral part of the shoulder, radiating to the ring finger and little finger when tapping with a hammer over the area where the nerve passes in the area of the medial epicondyle. Equivalent to Phalen's sign, sudden flexion of the elbow will cause paresthesia in the ring and little fingers. Frohman's test. Because of weakness of the abductor policis brevis and flexor policis brevis, excessive flexion of the interphalangeal joint of the thumb on the affected hand may be detected in response to a request to hold a paper between the thumb and index finger (Figure 5). Wartenberg test. Patients with more severe muscle weakness may complain that when putting their hand in a pocket, the little finger is pulled to the side (does not fit into the pocket) (Fig. 6).
Cubital and radial tunnel syndrome
Israeli doctors - Consultation | Diagnostics | Treatment > Cubital and radial tunnel syndrome
Ulnar nerve entrapment (ulnar tunnel syndrome) occurs when the ulnar nerve in the arm becomes compressed or irritated by something.
The ulnar nerve is one of the three main nerves of the arm. It runs from the neck down to the arm and can be narrowed in several places, such as under the collarbone or at the wrist. The most common location for nerve compression is at the back or inside of the elbow.
Common symptoms of cubital tunnel syndrome are numbness and tingling in the hands and fingers. In most cases, symptoms can be controlled with conservative treatments such as activity modifications. If conservative treatments do not relieve symptoms or nerve compression causes muscle weakness or damage to the arm, your doctor may recommend surgery.
The ulnar nerve passes through a tunnel of tissue (the cubital tunnel) and follows the tubercle of bone on the inside of the elbow. This bony tubercle is called the medial epicondyle. The place where the nerve passes under the medial epicondyle is commonly referred to as the "funny bone." At this point the nerve passes very close to the skin, and when touched, a very painful sensation similar to shock occurs.
The ulnar nerve provides sensation to the little finger and half of the ring finger. It also controls most of the small muscles in the hand that help make fine movements.
Causes
In many cases, the exact cause of cubital tunnel syndrome is not known. The ulnar nerve is especially vulnerable to compression at the elbow joint because it must pass through a narrow space with very little soft tissue to protect it. The ulnar nerve passes behind the medial epicondyle on the inside of the elbow.
There are several factors that can cause pressure on the nerve in the elbow:
In a flexed elbow position, the ulnar nerve is stretched around the ridge of the medial epicondyle. Because this stretch can irritate the nerve, holding the elbow in a bent position for long periods of time or bending the elbow repeatedly can cause painful symptoms. For example, many people sleep with their elbows bent. This may worsen the symptoms of ulnar nerve compression and cause the patient to wake up during the night. In some people, the nerve slips out from behind the medial epicondyle when the elbow is flexed. Over time, this sliding back and forth can irritate the nerve. Leaning on your elbow for an extended period of time can put pressure on the nerve. Fluid accumulation in the elbow can cause swelling, which can compress the nerve. A direct blow to the inside of the elbow can cause pain, an electric shock sensation, and numbness in the little and ring fingers.
Sleeping with your elbows bent can make symptoms worse.
Risk factors
Certain factors put you at greater risk of developing cubital tunnel syndrome. These include:
♦ Fracture or dislocation of the elbow ♦ Bone spurs/arthritis of the elbow ♦ Swelling of the elbow joint ♦ Cysts near the elbow joint ♦ Repeated or prolonged activities that require a flexed elbow position
Symptoms Cubital tunnel syndrome can cause aching pain on the inside of the elbow. Most symptoms, however, appear in the arm.
Numbness and tingling in the ring and little fingers are common symptoms of ulnar nerve impingement. Often these symptoms come and go. They occur more often when the elbow is bent, such as when driving a car or holding a phone. Some people wake up at night with numbness in their fingers. Feeling of "falling asleep" in the ring and little fingers, especially when the elbow is bent. In some cases, it may be more difficult to move your fingers or manipulate objects. Loss of grip and difficulty with finger coordination (for example, when playing a musical instrument). These symptoms are usually seen in more severe cases of nerve compression. If the nerve is very compressed or compressed for a long time, thinning of the muscles in the arm can occur, leading to loss of muscle mass. For this reason, it is very important to see a doctor if symptoms are severe or if they are less severe but have been present for more than 6 weeks.
Diagnosis The doctor first discusses with the patient his medical history, as well as his general health. He may ask the patient about his job, activities, and medications the patient may be taking.
After discussing symptoms and medical history, the doctor will examine the arm to determine which nerve is pinched and where. Some of the physical exam checks your doctor may do include: Tests ♦ X-rays. These tests provide detailed pictures of dense bone structures. Most causes of ulnar nerve compression may not be visible on x-rays. However, the doctor may take an X-ray of the elbow or wrist to look for bone spurs, arthritis, or evidence that the bone may be compressing a nerve.
♦ Nerve conduction studies. These tests can determine how well the nerve is functioning and also help determine where it is being compressed. Nerve conduction studies measure signals traveling along the nerves of the arm and hand. Nerves, like "electrical cables" that run through the body, carry messages between the brain and muscles. When the nerve does not perform its function properly, conduction takes a long time.
During a nerve conduction test, a nerve is stimulated in one location and its response is measured. Where the readings indicate a delayed reaction, there is probably a place where the nerve is being experienced. Nerve conduction studies can also determine whether the compression is also causing muscle damage. During the test, small needles are placed into some of the muscles. Muscle damage is a sign of more severe nerve compression.
Treatment If nerve compression does not cause muscle atrophy, your doctor will likely recommend nonsurgical treatment first. Non-steroidal anti-inflammatory drugs. If symptoms have just begun, your doctor may recommend anti-inflammatory medications to help reduce swelling around the nerve.
Although steroids such as cortisone are very effective anti-inflammatory medications, steroid injections are generally not used due to the risk of nerve damage.
Fixation. Your doctor may prescribe keeping your elbow in a straight position while you sleep.
Exercises. Some doctors believe that exercises that help the ulnar nerve slip through the cubital tunnel and Guyon's canal into the wrist may relieve symptoms. These exercises may also help prevent hand and wrist stiffness.
Surgical intervention. Your doctor may recommend surgery to relieve nerve pressure if:
♦ Non-surgical methods have not improved the condition ♦ The ulnar nerve is severely compressed ♦ Nerve compression has caused muscle weakness or damage
There are several surgical procedures that relieve pressure on the ulnar nerve. The orthopedic surgeon discusses with the patient the most suitable option for him.
These procedures are most often performed in an outpatient setting, but some patients may benefit from a 1-night hospital stay.
Release of the ulnar nerve. In this operation, the ligament from the cubital tunnel is separated. This increases the size of the tunnel and reduces pressure on the nerve.
After the procedure, the ligament begins to heal and new tissue begins to grow throughout the area. New tissue growth heals the ligament and creates more space for the ulnar nerve to pass through. Anterior transposition of the ulnar nerve. In this procedure, the nerve is moved from its location behind the medial epicondyle to a new location in front of it.
The nerve may be moved under the skin and fatty tissue, on top of the muscle (subcutaneous transposition), or into the muscle (intermuscular transposition), or under the muscle (axillary transposition).
Medial epicondylectomy. Another option to free the nerve is to remove part of the medial epicondyle. As with ulnar nerve transposition, this technique also prevents the nerve from being compressed and stretched when the elbow is flexed. Depending on the type of surgery, the patient may sometimes have to wear a brace for several weeks after surgery. Typically, submuscular axillary transposition requires a longer fixation time (3 to 6 weeks).
Your surgeon may recommend exercise to help restore strength and movement in your arm. The doctor also tells the patient when it is safe to return to their normal activities.
The results of the operation are usually good. Each surgical method has a similar success rate for common cases of nerve compression. If the nerve is severely pinched, or if there is muscle atrophy, it is possible that the nerve cannot be repaired and some symptoms may persist even after surgery. Nerves recover slowly, and it may take a long time to determine how well the nerve will function after surgery.
Contact us if you are not sure about your health condition or diagnosis, want to know the opinion of a leading Israeli doctor, need a clear, professional and reliable medical opinion and treatment according to modern protocols. We will promptly organize consultation and treatment in Israel.
Tel / Whatsapp / Viber +972 54 803 45 32 [email protected]
Treatment
At the initial stages of the disease, conservative treatment is carried out.
Changing the load on the elbow and eliminating elbow flexion as much as possible can significantly reduce pressure on the nerve. It is recommended to fix the elbow joint in an extension position at night with the help of orthoses, hold the car steering wheel with your arms straightened at the elbows, straighten the elbow when using a computer mouse, etc. If the use of traditional drugs (NSAIDs, COX-2 inhibitors, splinting) for 1 week does not have a positive effect, an injection of an anesthetic with hydrocortisone is recommended. If the effectiveness of these measures is insufficient, then an operation is performed. There are several techniques for surgical release of the nerve, but all of them in one way or another involve moving the nerve anteriorly from the internal epicondyle. After surgery, treatment is prescribed aimed at quickly restoring nerve conduction. Guyon's tunnel syndrome Guyon's tunnel syndrome develops due to compression of the deep branch of the ulnar nerve in the canal formed by the pisiform bone, the hook of the hamate, the palmar metacarpal ligament and the palmaris brevis muscle. There are burning pains and sensitivity disorders in the 4th–5th fingers, difficulty in pinching movements, adduction and extension of the fingers.
Tunnel ulnar syndrome is very often the result of prolonged pressure from working tools, for example, vibrating tools, screwdrivers, pliers, and therefore occurs more often in representatives of certain professions (gardeners, leather cutters, tailors, violinists, people working with jackhammers). Sometimes the syndrome develops after using a cane or crutch. Pathological factors that can cause compression also include enlarged lymphatic ganglia, fractures, arthrosis, arthritis, ulnar artery aneurysm, tumors and anatomical formations around Guyon's canal. Differential diagnosis. The difference between Guyon's canal syndrome and ulnar canal syndrome is indicated by the fact that when a nerve is damaged in the hand area, pain occurs in the hypothenar and base of the hand, as well as intensification and irradiation in the distal direction during provoking tests. In this case, sensitivity disorders occupy only the palmar surface of the 4th–5th fingers. On the back of the hand, sensitivity is not impaired, since it is provided by the dorsal branch of the ulnar nerve, which arises from the main trunk at the level of the distal third of the forearm.
When making a differential diagnosis with radicular syndrome (C8), it should be taken into account that paresthesia and sensitivity disorders can also appear along the ulnar edge of the hand. Paresis and hypotrophy of the hypothenar muscles are possible. But with C8 radicular syndrome, the zone of sensory disorders is much larger than with Guyon’s canal, and there is no hypotrophy and paresis of the interosseous muscles. If the diagnosis is made early, limiting activity may help. Patients can be recommended to use fixators (orthoses, splints) at night or during the day to reduce trauma. If conservative measures fail, surgical treatment is performed aimed at reconstructing the canal in order to free the nerve from compression.
More about the procedure
Causes of Carpal Tunnel Syndrome
Ulnar neuropathy occurs due to pressure on the ulnar nerve. Common causes of this disease are the following factors:
- systematic support on the elbow on a hard surface;
- the elbow joint is in a bent position for a long time;
- abnormal bone growth;
- heavy or frequent physical activity;
- a profession in which the joint is under constant load (working on a computer, telephone, etc.);
- injuries.
Diagnostics
Typically, a history and a thorough physical examination are sufficient to suspect ulnar tunnel syndrome. Treatment largely depends on the stage of development of the disease and the cause of its occurrence, which can be determined during the diagnostic process. For this purpose, the following methods are used:
- Electroneuromyography is a study that gives the doctor the opportunity to evaluate the work of the muscles of the forearm and hand, determine the speed of impulse transmission along the nerve - the degree of conduction disturbance (nerve function).
- X-ray, ultrasound, MRI are also used in the diagnostic process, especially if there is a suspicion of injury, fracture, arthritis, gout and other diseases.
Preparing for surgery
There are no special recommendations for preparing for surgery. On the morning of surgery, do not eat or drink anything. If you take medication regularly, take it with one sip of water.
Contraindications
- Diseases that prevent anesthesia (discussed during consultation with a doctor)
- Purulent-inflammatory diseases in the area of surgery
Features of the operation
The operation consists of freeing the nerve from compressing tissue. If there is excessive mobility of the nerve, it is moved, covered with muscles so that it does not stretch when the arm is bent at the elbow joint.
Postoperative period
- After surgery, it is imperative to continue treatment with medications: painkillers; vitamins; decongestants; improving conductivity and nerve trophism.
- It is imperative to use medications in conjunction with physical therapy and physiotherapeutic methods. Only in this case will it be possible to achieve the effect in 3-6 months. In rare cases, with an advanced stage and severe muscle atrophy, complete restoration of sensory and motor functions is not possible, so it is very important to consult a specialist as soon as the first symptoms of the disease appear.
Radial nerve compression syndrome
Three variants of compression damage to the radial nerve can be distinguished: 1. Compression in the armpit area.
Rarely seen. It occurs as a result of the use of a crutch (“crutch paralysis”), and paralysis of the extensors of the forearm, hand, main phalanges of the fingers, abductor pollicis muscle, and supinator develops. The flexion of the forearm is weakened, the reflex from the triceps muscle fades. Sensitivity is lost on the dorsal surface of the shoulder, forearm, and partly the hand and fingers. 2. Compression at the level of the middle third of the shoulder (spiral canal syndrome, “Saturday night paralysis”, “park bench”, “bench” syndrome). It occurs much more often. The radial nerve, emerging from the axillary region, bends around the humerus, where it is located in the bony spiral groove (groove), which becomes the musculoskeletal tunnel, since the two heads of the triceps muscle are attached to this groove. During the period of contraction of this muscle, the nerve is displaced along the humerus and as a result can be injured during forced repeated movements in the shoulder and elbow joints. But most often, compression occurs due to compression of the nerve on the outer-posterior surface of the shoulder. This usually occurs during deep sleep (deep sleep often occurs after drinking alcohol, which is why it is called “Saturday night syndrome”), in the absence of a soft bed (“park bench syndrome”). Pressure on the nerve may be due to the location of the partner's head on the outer surface of the shoulder. 3. Compressive neuropathy of the deep (posterior) branch of the radial nerve in the subulnar region (supinator syndrome, Froese syndrome, Thomson-Kopell syndrome, “tennis elbow” syndrome). Tennis elbow, tennis elbow, or epicondyllitis of the lateral epicondyle of the humerus is a chronic disease caused by a degenerative process in the area of muscle attachment to the lateral epicondyle of the humerus. Compression syndrome of the posterior (deep) branch of the radial nerve under the aponeurotic edge of the short extensor carpi radialis or in the tunnel between the superficial and deep bundles of the supinator muscle of the forearm can be caused by muscle overload with the development of myofasciopathies or pathological changes in perineural tissues. It manifests itself as pain in the extensor muscles of the forearm, their weakness and hypotrophy. Dorsal flexion and supination of the hand, active extension of the fingers against resistance provoke pain. Active extension of the third finger while pressing it and simultaneously straightening the arm at the elbow joint causes intense pain in the elbow and upper forearm. Treatment includes general etiotropic therapy and local effects. Take into account the possible connection of tunnel syndrome with rheumatism, brucellosis, arthrosis of metabolic origin, hormonal disorders and other conditions that contribute to compression of the nerve by surrounding tissues. Anesthetics and glucocorticoids are injected locally into the area of the pinched nerve. Complex treatment includes physical therapy, the prescription of vasoactive, decongestant and nootropic drugs, antihypoxants and antioxidants, muscle relaxants, ganglion blockers, etc. Surgical decompression with dissection of the tissues compressing the nerve is indicated if conservative treatment is unsuccessful. Thus, hand tunnel syndromes are a type of damage to the peripheral nervous system caused by both endogenous and exogenous influences. The outcome depends on the timeliness and adequacy of treatment, correct preventive recommendations, and the patient’s orientation in choosing or changing a profession that predisposes to the development of tunnel neuropathy.
The article uses drawings from the book by S. Waldman. Atlas of commom pain syndromes. – Saunders Elsevier. – 2008.
Rehabilitation
With conservative treatment
Conservative treatment can be considered successful if improvements are visible after 5-6 weeks. At the first stage, all exercises are performed together with an instructor or physical therapy doctor. Special exercises help to avoid constantly repeating tension on the ulnar nerve and pinching it in the groove. As improvements occur, the exercises become more challenging, adding exercises that strengthen the muscles and exercises that simulate daily activities. You may need to wear an elbow splint at night. Try doing all daily activities using your other arm or affected limb, keeping it straight. Avoid activities that require repeated flexion-extension of the elbow joint, especially while holding heavy objects. It is also unacceptable to keep your arm bent at the elbow joint for a long time.