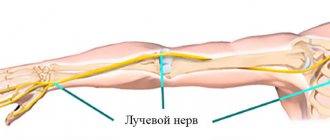
The radial nerve runs along the back surface of the shoulder, as if in a spiral, and gives off branches that provide movement of the muscles responsible for extension of the forearm and hand, outward rotation of the forearm, sensitivity of the skin of the back surface of the shoulder and forearm. Among other nerves of the hand, neuritis occurs most often in it.
Our expert in this field:
Lashch Natalia Yurievna
Neurologist of the highest category, candidate of medical sciences, associate professor. Laureate of the Moscow City Prize in the field of medicine.
Call the doctor Reviews about the doctor
General overview
Carpal tunnel syndrome (carpal tunnel syndrome) is a set of characteristic symptoms that occur when the median nerve is compressed in the wrist, ICD-10 code: G56.0. Includes numbness, paresthesia and pain in the zone of innervation of the median nerve. These sensations may be accompanied by objective changes in sensitivity and strength in the hand.
Diagnostics
The first line of diagnosis for numbness of the fingers in our clinic is electroneuromyography, this is especially true for carpal tunnel syndrome. To make a diagnosis, a combination of characteristic clinical signs and deviations from the norm found during electroneuromyography is necessary. Electrophysiological testing can also exclude other neurological problems (for example, in the cervical spine). With this study, it is possible to assess the severity of nerve damage, which helps in choosing further treatment tactics and determines the prognosis of the disease. An ultrasound scan can reveal masses that are putting pressure on the nerve.
MRI for carpal tunnel syndrome is prescribed exclusively for preoperative planning in cases of significant joint damage or neoplasms.
Treatment
There is evidence of the benefits of aerobic exercise and weight control in carpal syndrome. A bicycle or exercise bike is not the best exercise option, as it puts constant stress on your arms.
Using physical therapy such as ultrasound may provide temporary relief.
Many people with incipient syndrome (as measured by ENMG) usually respond well to the use of a night splint to maintain a neutral hand position during sleep (minimum three weeks).
Injection (blockade) with glucocorticoids, such as diprospan, shows good results if more conservative means do not work.
Patients who do not respond to conservative methods, or those who initially present with severe disease, are referred for surgical treatment.
Surgery for carpal tunnel syndrome (CTS) involves cutting the palmar ligament, which is compressing the median nerve. The success rate is very high (more than 90%), and the risk of complications is minimal. Recurrence after complete dissection of the palmar ligament of the hand is extremely rare. Surgical success is less likely for patients with normal electroneuromyography findings.
1.General information
The radial nerve is one of the branches of the brachial nerve plexus; it “bends around” the arm in a spiral channel and controls a number of motor functions and tactile sensitivity of the shoulder, forearm and hand.
Various lesions and injuries of the radial nerve, united by the concept of “radial nerve neuropathy,” are distinguished by a specific clinical picture and are an urgent problem for several branches of medicine (neurology, orthopedics, microsurgery, traumatology), since they occur more often than any other types of nervous pathology of the upper extremities.
A must read! Help with treatment and hospitalization!
Causes and pathophysiology of the process
Before the invention of electroneurophysiological testing in the 1940s, numbness in the fingers was more often attributed to compression of the brachial plexus by the cervical ribs or other structures in the anterior cervical spine. Now we know for sure that the median nerve is compressed in the inextensible rigid carpal tunnel, demyelination occurs (damage to the sheath of the nerve ending), and then damage to the axon itself. Sensory fibers are damaged first, motor fibers later. The ultimate mechanism of injury is still a matter of debate. At the moment, it is believed that the main problem is increased pressure inside the carpal tunnel. This pressure blocks venous outflow, swelling increases and even greater compression occurs, which ultimately leads to ischemia (lack of blood supply) to the nerve. The risk of occurrence may be associated with many factors: genetic, medical, social, occupational and demographic. Various combinations of these risk factors lead to the development of carpal tunnel syndrome, but at the moment we cannot confidently name a simple and clear cause.
Epidemiology
Disease frequency
The most accurate statistics are for the United States of America, where about 1–3 new cases of the disease are registered per 1000 people per year. On average, about 50 people out of 1000 suffer from carpal tunnel syndrome.
There is some lack of international statistics on this issue, but the prevalence of the syndrome in developed countries is similar to the United States, for example, in Holland there are about 2.5 new cases per year, and in the UK about 70-160 out of a thousand people ever seek help. Carpal syndrome is practically unheard of in developing countries, for example, among the indigenous population of South Africa.
Mortality/health threat
The disease is not fatal and cannot lead to a fatal outcome, but it can lead to serious irreversible impairment of hand function if correct treatment is not carried out.
It occurs more often in white Caucasian people.
It is believed that women suffer from carpal tunnel syndrome three times more often than men.
Peak occurrence occurs between 45–60 years. Only 10% of patients with this diagnosis are under 31 years of age.
Forecast and recovery
The recovery time for the radial nerve of the arm takes on average 1 – 2 months. The duration of rehabilitation is determined by the patient’s age, the nature of the lesion and the characteristics of concomitant diseases. Post-traumatic neuropathy requires a longer recovery.
To prevent neuropathy, you need to sleep in a comfortable position and give up bad habits. Persons whose profession involves frequent repetitive movements should regularly exercise and massage the upper extremities. It is also recommended to undergo a complete body examination every 6 months.
With timely treatment, it is possible to restore the functions of the radial nerve in 1-2 months. The timing and extent of nerve recovery largely depend on the depth and extent of its damage. In some cases, the disease becomes chronic and periodically worsens.
Neuropathy responds well to treatment at a young age.
In older people, complete recovery is difficult to achieve, especially in the presence of concomitant diseases. If left untreated, limb paralysis or contractures may occur. Elderly patients need to consult a doctor at the first signs of illness.
Symptoms of the disease
Often, the history and complaints of hand disease are more important than examination data when diagnosing carpal tunnel syndrome.
Numbness and tingling
Most often, people complain that objects fall out of their hands, their hands become “wobbly” and “weak,” needles and goosebumps can become frequent guests in their fingers.
Signs of carpal tunnel syndrome appear during certain jobs or activities:
- behind the wheel;
- when reading a book/newspaper;
- when working at a computer;
- while writing or drawing.
At night, unpleasant sensations force you to wake up and shake your brush. Some note that they need to walk around and put their hand in cold/hot water. Bilateral carpal tunnel syndrome is quite common, with the dominant hand usually affected earlier and more severely than the other.
Localization
Complaints should be focused on the palmar surface of the wrist and hand in the 1-2-3 and half of the fourth fingers, this is the zone of innervation of the median nerve. Numbness of the little finger and the back of the hand is the area of responsibility of other nerves and is not typical for carpal tunnel syndrome. Surprisingly, many patients cannot localize their symptoms and complain of numbness/weakness in the entire arm, which does not exclude this diagnosis.
Pain
Loss of sensitivity may be accompanied by burning pain in the palm, which often spreads to the fingers or along the forearm, sometimes to the elbow.
Pain in the area of the epicondyles of the elbow and higher in the shoulder or neck makes you think about other problems of the musculoskeletal system with which carpal tunnel syndrome can be combined. Identifying the causes of these pains requires a more detailed diagnosis.
Signs related to the autonomic nervous system
Patients often complain about the entire hand: a feeling of fullness, swelling of the hand and fingers; the hand may freeze or, conversely, feel hot. Many people react to the ambient temperature and do not tolerate cold well. Sometimes a change in skin color is noticed. In rare cases, there are complaints of changes in sweating in the palm. All this is associated with a violation of parasympathetic innervation, since the median nerve contains a considerable number of autonomic nerve fibers.
Weakness, lack of coordination
Decreased hand strength, especially when gripping with the thumb, often accompanies the disease. This may be due to loss of sensory response or pain. Objectively, weakness of the flexor digitorum longus and flexor digitorum profundus occurs when the median nerve is compressed above the level of the carpal tunnel. During the examination, the doctor will help determine the level of compression and choose the treatment necessary for you.
3. Symptoms and diagnosis
The clinical picture depends both on the location of the radial nerve lesion and on the severity of the damage. The most characteristic symptom associated with such neuropathies is a “dangling hand” when the outstretched arm is positioned parallel to the floor.
Other symptoms that occur with lesions and damage to the radial nerve are very diverse. It includes all kinds of pain (including during palpation along the nerve), disorders of the skin sensitivity of the shoulder and forearm, as well as the thumb, index, middle, and partially ring fingers (hypoesthesia and paresthesia, respectively, decreased sensitivity and false sensations in the form tingling, electric current, numbness, burning, etc.). Reflexes inherent in the upper limb are lost and/or weakened. Certain extension and flexion movements in the hand, elbow joint, and fingers are limited or become impossible (in particular, it is impossible to abduct the thumb or, conversely, bring it to the rest of the group of fingers). If neuropathy of the radial nerve remains for a long time without effective treatment, muscle atrophy may also begin against the background of degenerative changes and thinning of the nerve.
Lesions and injuries to the radial nerve are diagnosed clinically and reflexologically. Of the instrumental methods, electroneuromyography (measurement of nerve conduction functions and muscle response), as well as radiography and MRI, are of greatest importance - primarily to determine the causes of the lesion and for differential diagnosis.
About our clinic Chistye Prudy metro station Medintercom page!
What can be found during inspection?
Clinical examination is very important to exclude other pathologies of the musculoskeletal system or nervous system. Also, during the examination, you can identify characteristic signs of the disease to draw up a further examination plan.
Sensitivity tests
Changes in sensitivity can be observed along the palmar surface of fingers 1-2-3 and along the radial surface of the fourth finger. There is a Semmes-Weinstein test, a two-point discrimination test. The most commonly used test in practice is a prick test.
Sensory assessment confirms that areas outside the median nerve innervation are normal.
Strength tests
Weakening or loss of function of the following muscles: 1-2 lumbricals, oppons pollicis, flexor brevis, and abductor pollicis brevis indicate damage to the motor fibers of the median nerve distal to the carpal tunnel.
Special tests
There are no 100% reliable clinical tests to confirm carpal tunnel syndrome; a combination of them is evaluated.
- Tinel's sign. Gently tapping over the carpal tunnel causes shooting sensations in the fingers. It is the most common symptom in daily practice, despite its low sensitivity and specificity.
- Phalen's sign. Tingling/numbness occurs in the fingers when bending the wrist for 1 minute. The sensitivity of this test is 80%, the specificity is slightly lower.
- Wrist pressure test. When pressing on the wrist area with your thumb for 30 seconds, symptoms characteristic of nerve compression appear/intensify. Sensitivity 89%, specificity 96%.
- Palpation. The soft tissue surrounding the wrist is palpated for masses or other mechanical causes of nerve compression. Sensitivity reaches 90%, specificity 75% or more.
- Measurements to eliminate “square wrists”. If the thickness of the wrist in relation to its width has a proportion of more than 0.7, then the probability of developing carpal tunnel syndrome is about 70%.
Clinical picture
Clinical picture of de Quervain's tenosynovitis
The main complaint of patients is pain in the wrist on the side of the radius, which radiates to the forearm when trying to grab something with the thumb or straighten it. The pain is described as “constantly aching, burning, twitching.” Often the pain is aggravated when performing grasping, squeezing or twisting movements. Examination may reveal swelling in the area of the anatomical snuffbox, tenderness in the area of the styloid process of the radius, decreased range of motion in the first metacarpal joint, palpable thickening of the first dorsal compartment, and tendon crepitus. Other symptoms include weakness and paresthesia of the hand. These symptoms appear with a positive Finkelstein diagnostic test.
Causes
It is worth mentioning from the outset that carpal tunnel syndrome can be associated with various factors. On the one hand, it can be noted that the symptoms are more pronounced after or during the load on the hand, on the other hand, it cannot be said that the load on the hand is the cause or causes the disease. Associated does not mean is the cause.
Demography:
- Elderly age
- Female
- Increased body mass index, especially after rapid weight gain
- “Square” wrist shape
- Brachymorphic type of body structure (short arms, short legs)
- Dominant hand
- White Caucasian
Many factors are inherited (“square” wrist, thick palmar ligament, body type). Also, conditions associated with carpal tunnel syndrome have a hereditary predisposition (diabetes, thyroid disease, nephropathy, neuropathy).
Diseases/medical problems:
- Fractures of the distal radius
- Acute wrist injury (sharp flexion/extension)
- Neoplasms, injuries occupying a place in the carpal tunnel (tenosynovitis of the flexors, hygromas, hematomas, aneurysms, abnormal muscles, various tumors, edema)
- Diabetes
- Thyroid disorders (usually myxedema)
- Rheumatoid arthritis and other inflammatory diseases of the wrist joint
- Recent menopause
- Hemodialysis
- Acromegaly
- Amyloidosis
Carpal tunnel syndrome due to specific stress on the hand:
- Long power grip
- Prolonged stay in an extremely uncomfortable position
- Repeating the same movements multiple times
- When using the mouse and keyboard for a long time
- Prolonged exposure to vibration/cold
Other development factors:
- Lack of aerobic exercise
- Pregnancy and breastfeeding
- Using crutches/walkers/canes
Radial nerve. Anatomy
Note 1
The radial nerve (in Latin - n. radialis) is mixed in function. The radial nerve includes motor fibers that innervate the extensor muscles of the forearm.
Figure 1. Radial nerve. Author24 - online exchange of student work
From an anatomical point of view, these muscles include:
- Muscle of the hand (extensor of the little finger, supinator, extensor of the fingers, extensor carpi radialis: long and short, long muscle that abducts the thumb),
- Elbow muscle,
- Triceps.
Are you an expert in this subject area? We invite you to become the author of the Directory Working Conditions
Instrumental/laboratory diagnostics
Laboratory tests
There are no blood tests to diagnose carpal tunnel syndrome, but they may be ordered to screen for underlying conditions (such as diabetes or rheumatoid arthritis).
Radiation diagnostics
Radiation diagnostics is not used in routine practice.
MRI of the wrist may be useful in preoperative preparation to identify the causes of mechanical compression of the median nerve. Changes in the MR signal can be observed with chronic nerve compression, but they do not yet have practical significance for determining treatment tactics for the disease.
Many specialists now use ultrasound in addition to electrophysiological research methods. Ultrasound can reveal pathological processes that occupy space in the carpal tunnel, confirm changes in the median nerve (increase in cross-sectional area), which really help in diagnosis.
Electroneurophysiological studies
Electroneuromyography is the first-line diagnostic tool for carpal tunnel syndrome. Abnormalities found on ENMG in combination with specific symptoms and tests are the key to the correct diagnosis. Electroneuromyography can also exclude other neurological disorders.
Electrophysiological studies can also determine the extent of nerve damage, which is an objective criterion for prognosis.
Carpal tunnel syndrome is usually divided into mild, moderate and severe. The ranges for these groups may vary depending on the laboratory. In general, patients with isolated sensory disorders belong to the mild group, and if motor dysfunction occurs, they move to the moderate group. Confirmation of axonal damage (markedly decreased or absent sensory/motor response distal to the carpal tunnel) indicates severe disease.
Tracking the dynamics during ENMG helps determine the further approach to the disease.
Other quantitative tests, such as thermography or vibrometry, are less informative compared to ENMG and are not recommended for practical use.
Treatment of neuritis: methods
The treatment regimen for neuritis is drawn up taking into account the reasons that provoked the development of the pathological process. The patient may be recommended:
- antibiotics and antiviral agents (for infectious forms of the disease);
- anti-inflammatory, analgesic and decongestant drugs (for traumatic neuritis);
- vasodilators (in cases where the cause of the pathology is ischemia), etc.
Along with drug therapy, the treatment program includes physiotherapeutic procedures - UHF, exercise therapy, massage, ultraphonophoresis, etc. If the nerve is severely compressed, surgical intervention may be required (decompression of the nerve trunk by cutting the tissues pressing on it). With timely treatment of neuritis, the prognosis of the disease is favorable.
Treatment
Physical therapy
Since carpal tunnel syndrome has been shown to be associated with obesity and low mobility, correcting these factors will help improve the condition. An exercise bike, a bicycle and other exercises requiring prolonged grip are not indicated for this disease.
The use of physiotherapy devices may provide temporary relief. For example, short-wave diathermy provides significant temporary improvements compared with placebo, including reduction in symptoms and pain, and improvement in hand function.
Ergonomics and hand therapy
Wrist braces, which keep the hands in the correct position, have been shown to be effective as an at-home treatment when used at night for a minimum of 3 to 4 weeks.
They are inexpensive and safe, so in the initial diagnosis of the disease, a neutral night splint should be considered first.
Specific muscle strengthening programs and gliding exercises have not been shown to be effective. Massage and manual techniques that improve nerve glide have no proven therapeutic effect. Changes in the ergonomics of the workplace (table, chair, body position settings), changing equipment or tools are not effective in cases where the syndrome has already been confirmed.
Making a custom tire
Most people with early stage hand tunnel syndrome respond well to conservative therapy, which primarily consists of using a night brace for three weeks. Ready-made splints from orthopedic stores can provide improvement, but individual ones are more convenient and more effective, and therefore are preferable. It can be said that a special plastic splint molded to the patient's hand (orthosis) is the best choice for the initial treatment of carpal tunnel syndrome.
Drug therapy
Steroid injections into the carpal tunnel have been shown to be effective over the long term when other treatments have failed. Blockades can be indispensable in case of contraindications to surgical treatment, for example, during pregnancy. Ultrasound measurements of the median nerve of the arm predict the effectiveness of steroid blocks. Ultrasound navigation when performing a blockade does not lead to a reduction in complications or an increase in the effect of the blockade.
Anticonvulsants such as gabapentin or pregabalin, which are prescribed for various neuropathic pain, may also be used for carpal tunnel syndrome.
Nonsteroidal anti-inflammatory drugs (NSAIDs) and/or diuretics sometimes have some effectiveness in patients with special conditions (fluid retention or flexor tendon tenosynovitis)
However, in general, for all patients with carpal tunnel syndrome, the effectiveness of gabapentin, diuretics, or NSAIDs is controversial. According to the American Orthopedic Association guidelines, systemic medications (pills, intramuscular injections, IVs) are no more effective than placebo for treating carpal tunnel syndrome. In addition, it is worth noting that supplements with B vitamins (B-6 and B-12) also do not provide proven benefits.
4.Treatment
In case of damage to the radial nerve, the affected limb is immobilized and any physical activity on it is limited. Non-steroidal anti-inflammatory drugs, diuretics (to relieve swelling), painkillers, vitamin complexes, physiotherapeutic treatment, massage (only as prescribed and under the supervision of a doctor!) are prescribed. In some cases, hormone therapy is used, incl. with their injection into the affected area.
If compression of the nerve persists, conservative treatment is ineffective, and the cause of the lesion is known by time (for example, a recent fracture), microsurgical surgery on the radial nerve is indicated. If in the next few months it also turns out to be insufficiently effective in terms of restoring the functional viability of the limb, orthopedic surgery is performed.
Surgery
Sign up for a consultation
In patients for whom conservative therapy has failed, or for those who initially come to the appointment with a severe degree of carpal tunnel syndrome (according to ENMG), there are indications for surgery. Surgical dissection of the palmar ligament is highly likely (more than 90%) to lead to significant improvement with a low complication rate. The success of surgical treatment is reduced for people with normal electromyography.
Carpal tunnel decompression surgery is performed under local anesthesia in an outpatient operating room. This operation does not require hospitalization or the participation of an anesthesiologist.
The operation can be performed using a classic wide approach, as well as minimally invasive with or without the use of endoscopic equipment. The long-term results of a correctly performed operation are comparable for different methods of intervention.
The details of the surgical intervention and its necessity in your case should be discussed with a hand surgeon.
Causes of the disease
Neuritis is a polyetiological disease . The reasons for its occurrence may be:
- infections (herpes, brucellosis, influenza, etc.);
- injuries;
- hypothermia of the body;
- lack of vitamins and other nutrients;
- vascular disorders, ischemia;
- intoxication;
- compression of the nerve trunk that occurs while working or sleeping in an uncomfortable position;
- occupational hazards (for example, the need to constantly bend and straighten the hand when playing the cello).
In addition, neuritis can be provoked by medical errors made during surgical interventions.
What to do after detection?
When conservative therapy for carpal tunnel is initially prescribed, a follow-up consultation with a specialist is required within 4–6 weeks to assess effectiveness.
Patients who have not achieved the desired result with conservative treatment should be referred for surgical decompression of the carpal tunnel.
If symptoms persist after surgery, ENMG monitoring is required.
Re-appointment of the study should be done no earlier than 3 months after surgery.
Prevention
There are no proven effective methods of prevention for carpal tunnel syndrome.
Complications
Without treatment, the median nerve continues to be damaged, leading to permanent impairment of hand function and helplessness. If left untreated for a long time, some people develop constant pain in the wrist and hand.
Forecast
Carpal tunnel syndrome usually progresses over time and can lead to permanent damage to the median nerve. Whether a conservative approach can prevent progression is currently unclear.
Even after surgical decompression of the carpal tunnel, partial return of CTS symptoms after several years is possible (about a third of patients within 5 years).
If detected early, up to 90% of patients experience improvement with conservative treatment, which does not preclude the need for surgery in the future.
Patients with comorbidities (diabetes or radius fracture, etc.) have a relatively worse prognosis compared to those who do not have such factors.
Patients with normal ENMG findings are less likely to improve after surgery compared with those with confirmed median nerve compression.
Patients with confirmed axonal injury have a poorer prognosis for complete nerve recovery.
Classification of the disease
Radiation neuropathy refers to compression of nerves localized in the following areas of the extremities:
- Armpit – causes paralysis of the forearm muscles and weakening of the triceps muscle.
- Middle third of the shoulder.
- Elbow joint – this type of neuropathy is called “tennis player’s syndrome.” Damage to the nerve causes dystrophic changes in the ulnar ligaments and extensor muscles of the hand.
- Wrist.
Symptoms of a pinched radial nerve are as follows:
- if a person stretches his arms in front of him, then his hands hang down, his fingers are close together;
- the elbow joint, hand and forearm do not straighten;
- the hand goes numb;
- if the hand is lowered down, the thumb is not retracted;
- the palm cannot be turned upward;
- the thumb cannot touch the palm;
- the interosseous muscles of the injured arm atrophy;
- painful sensations.
Diagnosis of the disease is a very important step on the path to recovery. The fact is that dysfunction of the hand extensors, which is often observed with a pinched nerve, is accompanied by a loss of performance of the flexors. Therefore, the disease can easily be confused with damage to the ulnar nerve, and to make the correct diagnosis you need to undergo special tests.
Test No. 1. If your doctor asks you to shake his hand and your hand sags even more when you try, you definitely have neuropathy.
Test No. 2. Squeeze your palms in front of you so that all fingers are in contact with their “counterparts” on the other hand. If you begin to move your palms away from each other, the fingers on the injured hand will begin to bend into a fist.