Radiation diagnostics
CT semiotics
A soft tissue infiltrate is detected in the area of the cavernous sinus, spreading through the optic canal, the superior orbital fissure into the orbit; through the inferior orbital fissure, the infiltrate spreads into the pterygopalatine fossa and paranasal sinuses.
MRI semiotics
T1-weighted images: granulomas have an isointense MR signal
T2-VI, FLAIR: granulomas are iso-, slightly hyperintense
Contrast-enhanced T1-weighted images: granulomas usually accumulate contrast agent
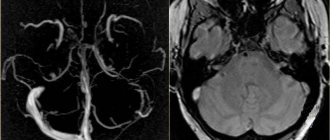
MRA, CT angiography: narrowing of the lumen of the internal carotid artery may be observed.
Differential diagnosis
It is carried out with various pathological processes leading to the development of secondary superior orbital fissure syndrome. These include primary or secondary (metastatic) tumors of the anterior or middle cranial fossa (meningioma, non-Hodgkin's lymphoma), neurosarcoidosis, vascular anomalies (carotid-cavernous anastomosis, dissection of the ICA wall, ICA aneurysms), orbital myositis, cavernous sinus thrombosis, hypertrophic basal pachymeningitis, Wegener's granulomatosis, polyarteritis nodosa, etc.
Fig.1. MRI of the brain, T2-VI in the coronal plane: in the projection of the left cavernous sinus an isointense infiltrate is determined, partially narrowing the lumen of the left ICA.
Fig.2. MRI of the brain in the axial plane, a – T1-FS after IV contrast, b – T2-VI. In the area of the right cavernous sinus, a zone of accumulation of contrast agent is determined with a partial narrowing of the lumen of the right ICA (a, green arrows); on T2-WI this zone has a hypointense MR signal (b, green arrows) due to fibrotic changes.
Fig.3. MRI of the brain, T1-VI in the axial plane after intravenous contrast (a, b): a - state before treatment: in the projection of the left cavernous sinus, apex of the orbit and superior orbital fissure, a tissue component is visualized, intensively homogeneously accumulating contrast agent: b – after treatment with glucocorticosteroids, there is a significant decrease in the size of the infiltrate.
Toloza-Hunt syndrome: a neurological chameleon
V.V. Ponomarev, City Clinical Hospital No. 5, Minsk, Republic of Belarus
Summary
A survey of 130 patients with Toloz-Hunt syndrome was carried out. It has been established that the most common etiological factor in the development of the disease is autoimmune inflammation of the outer wall of the cavernous sinus, sometimes with the formation of granulomas (40%). Less common causes of Toloz-Hunt syndrome were vascular malformations (13%), primary or metastatic brain tumors (7.8%), limited cranial pachymeningitis (4%), orbital myositis (3.0%), cavernous sinus thrombosis and polyarteritis nodosa (0.7%). In 30.8% of patients, the cause of the disease remained unspecified. Epidemiological and clinical features for various causes of the disease have been studied. In autoimmune Toloza-Hunt syndrome, the following have been established: high levels of pro-inflammatory cytokines (interleukin-6 and TNF-alpha) in the blood serum and cerebrospinal fluid; inflammatory infiltration or granulomas of the outer wall of the cavernous sinus on magnetic resonance imaging; in 20% of cases - subclinical damage to the visual analyzer during the evoked potential technique; high efficiency of glucocorticoids.
Keywords
Toloz-Hunt syndrome, cavernous sinus granuloma, proinflammatory cytokines.
Toloza-Hunt syndrome (STX, painful ophthalmoplegia, superior orbital fissure syndrome) was first described by the Spanish neurologist E. Tolosa in 1954 and supplemented by the English physician W. Hunt in 1961 [6, 15]. This pathology is manifested by damage to the structures passing through the superior orbital fissure (orbital artery and vein, abducens, trochlear, oculomotor nerves, first branch of the trigeminal nerve), and the adjacent cavernous sinus. The clinical picture of STX is characterized by pain, often in the orbital area, diplopia, exophthalmos and chemosis, which manifest themselves in various combinations and vary in severity [7, 8, 13]. Practice shows that similar clinical signs are observed in a wide range of neurological and somatic diseases: bacterial, viral and fungal inflammation of the outer wall of the cavernous sinus or meninges; primary or secondary tumors of the brain and orbit; vascular malformations and dissections of branches of the internal carotid artery; thrombosis, lymphoma, epidermoid cysts of the cavernous sinus; orbital myositis, sarcoidosis, Wegener's granulomatosis, some blood diseases, ophthalmic migraine, etc. [1-3, 5, 12, 14].
Thus, the formation of CTX is based on various reasons that determine the multifaceted nature of the disease. In nature, this analogue of diversity is called a chameleon. In recent years, undoubted progress has been made in understanding the mechanisms of development of this disease. According to the criteria developed by the International Headache Society (2004), the diagnosis of CTX is justified in cases where a granuloma of the outer wall of the cavernous sinus is detected during magnetic resonance imaging (MRI) of the brain or during a biopsy [10]. In the absence of changes on MRI, the term “superior orbital fissure syndrome” is more appropriate, and in these cases patients require dynamic monitoring.
The relative rarity of CTX, the polymorphic and polyetiological nature of the disease create significant difficulties in its timely diagnosis and the choice of differentiated therapy in the practice of not only neurologists, but also neurosurgeons, ophthalmologists, endocrinologists, oncologists, rheumatologists, etc. The presented work summarizes our own long-term experience in diagnosis and treatment of this pathology.
Material and research methods
From 1990 to 2007 In the II neurological department of our clinic (until 2005 - the clinical base of the Research Institute of Neurology, Neurosurgery and Physiotherapy of the Ministry of Health of the Republic of Belarus), 130 patients with STX (64 men, 66 women, age 51.7 ± 12.4 years) were observed. A traditional neurological examination was performed. The condition of the fundus was assessed and ophthalmometry was performed according to Hertel. General clinical and immunological tests of blood and cerebrospinal fluid (CSF) were performed. There, interleukin-6 and TNF-alpha were quantified by enzyme-linked immunosorbent assay using a Cytokine reagent kit (St. Petersburg). Visual evoked potentials were recorded using a Compass diagnostic complex from Nicolet (USA). CT and MRI studies of the brain were performed using Siemens Somatom (Germany), Vista Polaris from Picker (USA) with a magnetic field voltage of 1 Tesla, and digital subtraction carotid angiography (CAG) using the Neurostar complex (Germany). The results of laboratory studies were subjected to statistical processing with the calculation of Student's t-test. Results P < 0.05 were considered significant. Follow-up ranged from 1 year to 17 years.
Results and discussion
When analyzing the data obtained, it was found that CTX occurred equally in both men and women over a wide age range (from 15 to 87 years). The left and right sides were affected with equal frequency, but the process was always unilateral. Clinical manifestations of the disease developed acutely or subacutely, after a previous viral infection, hypothermia, increased blood pressure, or for no apparent reason. As a rule, the first neurological symptom of STX was pain of varying intensity, localized in the retrobulbar, frontal, superciliary or temporal regions. A few days later (less often simultaneously), double vision, strabismus, and limited mobility of the eyeball on the side of the pain occurred. The direction of diplopia and strabismus depended on the cranial nerve involved. When all nerves passing through the superior orbital fissure were affected, total ophthalmoplegia developed, but this was noted only in every fourth patient. Incomplete forms of STX were more common, in which nerves VI, IV, III pairs and the I branch of the V pair were involved in the pathological process in various combinations. Some patients experienced exophthalmos and chemosis (swelling and redness of the conjunctiva of the eye). No other neurological syndromes (pyramidal, hypertensive, cerebellar, pseudobulbar, cognitive) were identified in the study group. Quite often, the examined patients had a recurrent course, when similar neurological symptoms recurred at different times (from 6 months to 11 years) on the same, less often on the opposite side of the face.
A comprehensive examination of patients made it possible to identify the main reasons for the formation of CTX. The most common etiological factor in the development of the disease was autoimmune inflammation of the outer wall of the cavernous sinus, sometimes with the formation of granulomas - 52 people. (40%). Less commonly, the cause of STX was vascular malformations - 17 people. (13%), primary or secondary brain tumors - 10 people. (7.8%), limited cranial pachymeningitis - 5 people. (4%), orbital myositis - 4 people. (3.0%), cavernous sinus thrombosis and polyarteritis nodosa - 1 person each. (0.7%). In 40 (30.8%) patients, the cause of the disease remained unspecified, and we interpreted such cases as idiopathic. The etiological factor in the development of CTX determined some epidemiological and clinical features of the disease.
Autoimmune CTX developed not only after hypothermia, previous infections, but also after stress. Men suffered more often (59.6%). The characteristic features of the disease were: acute onset (76.9%), incomplete forms (83.1%), moderate or severe pain syndrome (80.7%) and high efficiency of glucocorticoid therapy (92%). Among the cranial nerves involved, the oculomotor nerve was most commonly involved. In 25% of patients with classic symptoms of its damage (ptosis, divergent strabismus, limited upward and inward movements of the eyeball), normal pupil diameter was observed. In autoimmune CTX, the following were quite typical: recurrent course - in 28% and protein-cell dissociation in the CSF (0.44-1.87 g/l) - in 44% of cases. Mild or moderate exophthalmos (20-24 mm) occurred only in 19.2%, and chemosis in 10% of patients. Conducting evoked visual potentials in 4 people. of 14 patients revealed subclinical damage to the optic nerves. Routine blood tests revealed no pathology. When studying the immune status in blood serum, the most significant disorder in half of the patients was activation of cellular and/or humoral immunity. Changes in the IgG content in the CSF were unreliable. There was a significant increase in interleukin-6 in the blood serum - up to 0.13 ± 0.01 pg/ml (P < 0.05) and TNF-alpha in the CSF - up to 0.109 ± 0.01 pg/ml (P < 0.05 ). MRI of the brain revealed thickening of the outer wall of the cavernous sinus or granulomas in 6 patients.
Vascular malformations were more common in women (70.5%), almost always against the background of decompensated arterial hypertension. The acute nature of the process and moderate pain syndrome predominated. The oculomotor and abducens nerves were involved in the process equally often. Exophthalmos and chemosis were practically not encountered. MRI and CAG revealed arterial aneurysms (3-30 mm in diameter) of the supraclinoid division of the internal carotid artery in 13 patients; in 2 cases - in the infraclinoid region; in 2 patients - carotid-cavernous anastomosis. In 1 case, two aneurysms were simultaneously detected in the carotid region. In 7 patients, aneurysm ruptures were observed and red blood cells were detected in the CSF. In 3 cases, dynamic MRI revealed spontaneous thrombosis of aneurysms. Levels of interleukin-6 and TNF-alpha in serum and CSF did not change. In 6 patients, aneurysm neck clipping was performed.
Tumors more often (in 8 people) developed subacutely for no apparent reason. The clinical picture was dominated by exophthalmos (22-28 mm), chemosis and total ophthalmoplegia in 7 patients. In 6 cases, the cause of STX was primary brain tumors. In four patients, the tumor process was metastatic in nature (the primary focus was found in the lungs, bronchi, prostate gland, and the primary focus was skin melanoma). In 4 patients the tumor was removed (histologically, neurinoma - 2 people, meningioma - 2 people). In 1 case, gamma knaif was used for treatment.
Limited cranial pachymeningitis was diagnosed in 5 patients (4 men, 1 woman, age 29-43 years). These patients were characterized by an acute onset, absence of cerebral, general infectious symptoms and meningeal signs. Exophthalmos and chemosis were not encountered. In the CSF of all patients, predominantly lymphocytic pleocytosis was observed from 258 x 106 to 564 x 106 cells/l, in 2 cases the protein simultaneously increased to 0.81 and 1.7 g/l. In 1 case, the diagnosis was confirmed morphologically during surgery with a biopsy of the dura mater.
Orbital myositis occurred in 4 patients (3 women, 1 man, age 40-70 years). The clinical picture developed subacutely, with intense pain in the orbit, exophthalmos (> 28 mm), severe chemosis and diplopia in only one direction. Thyroid function was not impaired. MRI of the orbit showed a unilateral increase in the volume of the internal muscles of the eye.
Cavernous sinus thrombosis was diagnosed in a 76-year-old woman with subacute development of total ophthalmoplegia on the left, severe chemosis and exophthalmos. MRI revealed a hyperintense area and a sharply dilated left ophthalmic vein in the projection of the cavernous sinus.
Polyarteritis nodosa was noted in a 42-year-old woman who developed subacute arthralgia, then infarction-pneumonia and progressive renal failure. Against this background, 6 months after the onset of the disease, pain in the eyeball and total ophthalmoplegia on the right appeared. CSF studies and MRI of the brain revealed no pathology.
Idiopathic CTX usually develops for no apparent reason. Elderly and senile patients predominated (68%). The pain syndrome was not expressed, protein-cell dissociation was not observed in the CSF, and less effectiveness of glucocorticoids was noted (in 72% of cases). There were no changes on MRI of the brain or they were nonspecific - in the form of external or communicating hydrocephalus and leukoaraiosis.
Neurological symptoms in STX are associated with the topical level of localization of the pathological process. The pain syndrome in this disease is caused by irritation of the first branch of the trigeminal nerve, which runs next to the trunk of the oculomotor nerve. The localization of pain may vary: orbit, forehead, temple, root of the nose. The intensity of pain has a wide range - from minimal to severe. Atypical (painless) variants of STX, associated with the localization of the pathological process before the entry of the V pair into the cavernous sinus, should be taken into account. In relation to the sinus, anterior, middle and posterior variants of STX are distinguished [1]. Oculomotor disorders in this pathology are most often manifested by diplopia when looking straight, inward and upward due to damage to the third cranial nerve. The remaining oculomotor nerves are involved in the pathological process in various combinations. The absence of mydriasis with damage to the oculomotor nerve may be associated with simultaneous damage to the pericarotide sympathetic fibers [15]. The formation of incomplete clinical variants of STX is associated with partial damage to the superior orbital fissure, in which the abducens nerve is located laterally, the oculomotor nerve is located in the middle, and the trochlear nerve is located in its upper part. CC Lin and JJ Tsai found a linear correlation between the number of cranial nerves and the volume of cavernous sinus lesions [9]. The literature describes variants of STX with isolated damage to individual cranial nerves. Thus, A. Kikuchi et al. [7] among 118 patients with STX, isolated lesions of the abducens nerve were observed in 5.1% of cases. The pathogenesis of damage to cranial nerves in STX is associated with their inflammatory infiltration, and in tumors, aneurysms, or orbital myositis, their compression occurs [5].
When the process is localized in the area of the orbital apex, neurological symptoms are combined with a disturbance of the visual analyzer, which is clinically manifested by edema or atrophy of the optic nerve head or central scotoma [1]. The most common ophthalmological symptoms of CTX are exophthalmos and chemosis, the development of which is associated with infiltration of retrobulbar tissue and obstruction of venous outflow from the orbit. Unlike orbital myositis or cavernous sinus thrombosis, these symptoms in STX are never leading and do not reach a pronounced degree [2]. In our studies, in 20% of patients, when performing the visual evoked potential technique, subclinical visual disturbances were identified, indicating that the pathological process in STX may topically extend beyond the superior orbital fissure and cavernous sinus.
Autoimmune mechanisms, which most often underlie CTX, are emphasized by most authors [1, 8, 10, 12, 13]. Y. Tanaka et al. [12], having described the simultaneous development of autoimmune neutropenia and CTX in a 47-year-old woman, note similar immune mechanisms in the formation of both diseases. In our studies, the autoimmune nature of the process was indicated by: recurrent nature, dysimmune disorders in the blood, protein-cell dissociation in the CSF and high levels of pro-inflammatory cytokines (interleukin-6 and TNF-alpha) in the serum and CSF. Noteworthy was the normal content of IgG in the CSF, which indicated the absence of intrathecal synthesis of these antibodies in this disease.
CTX occurs in a number of diseases with a similar clinical picture. Clinical diagnostic criteria for CTX are the following signs [1]:
- “drilling” or “gnawing” pain inside the orbit, ophthalmoplegia following it or developing simultaneously;
- damage in various combinations of all oculomotor nerves, the first branch of the trigeminal nerve and the fibers of the periarterial plexus;
- progression of symptoms over several days and weeks;
- spontaneous remissions, sometimes with a residual defect;
- the possibility of relapses after several months or years;
- the absence of any changes outside the carotid sinus or systemic reactions upon careful examination of the patient.
W. Hunt et al. [6] the diagnostic criteria for this disease included the effect of corticosteroids.
A recurrent course is a characteristic feature of any autoimmune pathology. In autoimmune STX, exacerbations were observed in 28% of patients. The duration of remission varied greatly, with a maximum of 11 years. Our study noted a less severe course of relapses with early administration of specific therapy.
In recent years, neuroimaging methods have been given a greater role in the diagnosis of STX, since biopsy through the transsphenoidal approach is usually limited. T. Ozawa et al. [11] proposed an MRI criterion for STX: the presence in the wall of the cavernous sinus of pathological tissue that is isointense in the T1w mode and isohypointense in the T2w mode. According to La L. Mantia et al. [10], inflammatory infiltration or granulomas in the area of the cavernous sinus were detected on MRI in 44 (35%) of 124 cases of STX. T. L. Haque et al. MRI revealed small lesions adjacent to the cranial nerves without extension to the cavernous sinus. When performing dynamic MRI after taking glucocorticoids, the authors found a complete disappearance of the lesions, which suggests their granulomatous nature [4].
Of practical importance is the exclusion of the secondary (symptomatic) nature of the disease. According to our data, the specific gravity of secondary CTX was 29.2%. Similar data (31%) were obtained by La L. Mantia et al. in a large-scale European study [10]. According to some authors [1, 5], the diagnosis of CTX can only be established by excluding diseases with a similar clinical picture. Among them there are primary brain tumors (pituitary adenoma, sphenoid wing meningioma, craniopharyngioma, neuroma) and metastases to the brain or orbit. Similar clinical symptoms manifest themselves in arteriovenous aneurysms of the internal carotid artery, which are located extradurally and are not always accompanied by subarachnoid hemorrhage, since the walls of the cavernous sinus prevent the enlargement of the aneurysm and protect it from rupture. Another variant of vascular malformations is carotid-cavernous anastomosis, which is manifested by the rapid development of ophthalmoplegia, pulsating exophthalmos, noise in the orbit, and vascular disorders in the anterior segment of the eye. Very rarely, CTX is a manifestation of systemic diseases, in particular Wegener's granulomatosis or polyarteritis nodosa. With this pathology, the neurological symptoms of STX are combined with changes in the respiratory system, ENT pathology and multiple organ symptoms (damage to the eyes, kidneys, skin, musculoskeletal system, gastrointestinal tract). A characteristic laboratory test of the disease is the presence of antibodies to the cytoplasm of neutrophils in 97% of cases [1]. According to P. Thajeb [13], in some cases, CTX represents a limited form of Wegener's granulomatosis. Also rarely, STX is observed with limited pachymeningitis at the base of the brain. In these cases, the diagnosis is confirmed by extraparenchymal infiltration on MRI of the brain or specific pathomorphological abnormalities on biopsy of the dura mater [3]. Particularly noteworthy are cases of idiopathic CTX, when there are no inflammatory or autoimmune causes, and MRI is normal, or these changes are nonspecific. In our opinion, such patients require follow-up observation in order to exclude other genesis of the disease.
Treatment of CTX consists of immunosuppressive therapy. Most researchers indicate the high effectiveness of corticosteroids in this pathology. However, the relative rarity of CTX precludes placebo-controlled studies. Prednisolone or its analogues (Medrol) are usually prescribed in tablets at a dose of 1-1.5 mg/kg body weight or intravenously 500-1000 mg/day. [2, 4-6]. It should be taken into account that glucocorticoids are effective (albeit to a lesser extent) in other pathological conditions: sarcoidosis, aneurysms and tumors.
Thus, CTX is a polyetiological syndrome. Detection of CTX in patients requires careful differential diagnosis. If the autoimmune nature of the disease is established, glucocorticoids are highly effective.
The author expresses sincere gratitude to the staff of the neurological, neurosurgical, diagnostic departments of the hospital, as well as the clinical diagnostic laboratory for their many years of assistance in conducting this study.
References 1. Damulin I.V., Lokshina A.B., Artemyev D.V. and others. Painful ophthalmoplegia syndrome caused by Wegener's granulomatosis // Nevrol. magazine - 2002. - No. 5. - P. 29-35. 2. Ponomarev V.V. Rare neurological syndromes and diseases. - St. Petersburg, 2005. - 216 p. 3. Bosch J., Ortega-Aznar A., Tintore M. et al. Hypertrophic pachymeningits. A review of the histories of two cases and pathological relationship with the Tolosa-Hunt syndrome and the orbital pseudotumor // Rev. Neurol. - 2000. - Vol. 31, No. 10. - P. 946-951. 4. Haque T.L., Miki Y., Kashii S. et al. Dynamic MR imaging in Tolosa-Hunt syndrome // Eur. J. Radiol. - 2004. - Vol. 51, No. 3. - P. 209-217. 5. Gladstone JP, Dodick DW Painful ophthalmoplegia: overview with a focus on Tolosa-Hunt syndrome // Curr. Pain Headache Rep. - 2004. - Vol. 8, No. 4. - P. 321-329. 6. Hunt WE, Meagher JN, Le Fever HU et al. Painful ophthalmoplegia. It's relation to indolent inflammation of the cavernous sinus // Neurology. - 1961. - No. 11. - P. 56-62. 7. Kikuchi A., Shiga Y., Onodera J. et al. A case of Tolosa-Hunt syndrome starting from abducens nerve palsy alone // Rinsho. Shinkeigaku. - 2001. - No. 6. - P. 296-298. 8. Klein LB, Hoyt WF The Tolosa-Hunt syndrome // J. Neur. Neuros. Psych. - 2001. - Vol. 71, No. 5. - P. 577-582. 9. Lin CC, Tsai JJ Relationship between the number of involved cranial nerves and percentage of lesions located in the cavernous sinus // Eur. Neurol. - 2003. - Vol. 49, No. 2. - P. 98-102. 10. Mantia La L., Curone M., Rapoport AM, Bussone G. Tolosa — Hunt syndrome: critical literature review based on INS 2004 criteria // Cephalgia. - 2006. - Vol. 26, No. 7. - P. 772-781. 11. Ozawa T., Minakawa T., Saito A. et al. MRA demonstration of “periarteritis” in Tolosa - Hunt syndrome // Acta Neurochir. - 2001. - No. 3. - P. 309-312. 12. Tanaka Y., Tsukamoto N., Sakuraya M. et al. Autoimmune neutropenia accompanied by Tolosa - Hunt syndrome // Rinsho. Ketsueki. - 1999. - Vol. 40, No. 11. - P. 1168-1173. 13. Tessitore E., Tessitore A. Tolosa — Hunt syndrome preceded by facial palsy // Headache. - 2000. - Vol. 40, No. 5. - P. 393-396. 14. Thajeb P., Tsai JJ Cerebral and oculorhinal manifestations of a limited form of Wegener's granulomatosis with c-ANCA-associated vasculitis // J. Neuroimaging. - 2001. - Vol. 11, No. 1. - P. 59-63. 15. Tolosa E. Periarteritic lesions of the carotid siphon with the clinical features of a carotid infraclinoid aneurysm // J. Neur. Neuros. Psych. - 1954. - Vol. 17. - P. 300-302.
Description example
Descriptive part (brain): in the projection of the outer wall of the right cavernous sinus, soft tissue formations (granulomas) up to 0.6 cm in diameter with a diffuse-homogeneous type of accumulation of contrast agent are determined.
Conclusion: The MR picture of a focal infiltrative lesion in the wall of the right cavernous sinus, taking into account the location, signal characteristics and accumulation of contrast agent, may correspond to the manifestations of Tolosa-Hunt syndrome.
Descriptive part (MRA): multiple small parietal filling defects are determined at the level of the subclinoid segment of the right ICA (ascending part) and siphon, the minimum diameter of the artery at the level of the subclinoid segment on the right is 0.2 cm.
Conclusion: MRA picture of narrowing of the lumen and decreased blood flow of the intracranial section of the right internal carotid artery, multiple small parietal filling defects at the level of the subclinoid segment (ascending part), siphon of the right internal carotid artery.
Mechanism of disease development, symptoms of the disease
The disease begins without any prerequisites and immediately in an acute form, with pain in the orbital region. Painful sensations appear in the frontal part, in the area of the superciliary arches, and with increasing intensity they spread to the eyes. This is followed by the development of symptoms in increasing order, replacing each other:
- There is a problem with eye movement, diplopia (double vision). It is difficult for the patient to concentrate his gaze on one object, everything is double;
- ophthalmoplegia (impaired mobility of the eyeball). In most cases it is unilateral. The degree of immobility depends on the number of nerves damaged and the intensity;
- exophthalmos (displacement of the eyeball) occurs if no treatment is carried out or with a frequently recurring syndrome;
- strabismus can develop with unilateral nerve damage;
- deterioration of general condition and increase in temperature.
All of these symptoms can increase one after another, gradually causing external changes. But in some cases, with a rapid flow, they can appear almost simultaneously.
Sometimes, for unknown reasons, obvious signs of the disease suddenly disappear on their own. However, without receiving appropriate treatment, relapse is possible. The duration of remission can be completely different, as well as the frequency of relapses.
List of used literature and sources
- Diagnostic imaging. Brain / Anne G. Osborn, Karen L. Salzman, and Miral D. Jhaveri. 3rd edition. ELSEVIER. Philadelphia, 2021. P.1237. ISBN: 978-0-323-37754-6
- Rohini Nadgir, David M.Yousem. Neuroradiology. 4th edition. ELSEVIER. Philadelphia, 2021. P.630. ISBN: 78-1-4557-7568-2
- Tolosa-Hunt syndrome [Electronic resource] / Radiopaedia.org: website. – URL: https://radiopaedia.org/articles/tolosa-hunt-syndrome-3 (06/11/2018)
- Neurology: national guide / ch. ed. E.I. Gusev, A.N. Konovalov, V.I. Skvortsova, A.B. Gekht. – M.: GEOTAR-Media, 2009. – 1035 p.
- Ponomarev V.V. Tolosa-Hunt syndrome: definitions, clinical picture, diagnosis, treatment // Medical news. – 2015. – No. 1. – P. 6-9.