13 May 2020
173381
1
3.8 out of 5
Sciatica is sometimes also called lumbosacral radiculitis - a chronic neurological disease in which the sciatic nerve passing through the buttock and leg is compressed. This is accompanied by severe pain and a number of other disorders. It can occur at any age in people of both sexes, often occurs in pregnant women, but is most often diagnosed in people 40–60 years old. Although sciatica is not life-threatening, it can significantly reduce the quality of life and deprive a person of ability to work. Therefore, when the first signs appear, you should contact a neurologist and begin treatment immediately. In this case, it will be as easy as possible, effective and will allow you to quickly eliminate both the signs of the disease and the causes of its occurrence.
What does the word lumboischialgia mean?
Sciatica is pain in the lower back that extends to one or both lower limbs. It is a reflex syndrome and belongs to the non-radicular phase of lumbar osteochondrosis, as well as lumbodynia and lumbago. Therefore, it would be more correct to say that there is lumboischialgia syndrome on the right or lumboischialgia syndrome on the left.
What is “discogenic lumboischialgia”?
If during diagnosis it is established that the cause of such complaints is a disc herniation or protrusion, then we can say that this is discogenic lumboischialgia.
How is it going?
If the pain occurs acutely and is of a pronounced nature, then this is acute lumboischialgia. If the pain is moderate and bothers you for a long time, periodically exacerbating, this is chronic lumboischialgia.
What can lumboischialgia be?
Depending on the nature of neurological disorders, vascular, muscular-tonic, and muscular-dystrophic forms of lumboischialgia are distinguished.
What causes lumboischialgia syndrome to appear?
Vertebrogenic lumboischialgia syndrome most often occurs after hypothermia, as well as after increased stress on the muscles of the lower back and legs. As a result, tonic muscle strain occurs and pain appears in the lower back and leg.
Advantages of the clinic
Energy of Health clinics offer each patient high-quality and affordable medical care, including:
- comprehensive screening programs to identify acute and chronic diseases;
- consultations with specialists of a wide and narrow profile;
- full range of laboratory diagnostics;
- modern methods of instrumental and functional examination;
- all types of drug and non-drug treatment;
- preventive measures to maintain the health of the body.
A pinched sciatic nerve can cause severe pain that interferes with normal movement and self-care. Do not try to treat it at home, seek help from Health Energy.
Symptoms of lumbar sciatica and diagnosis of lumbar sciatica
The main complaints are pain in the lower back and legs. Both lumbar sciatica on the right and lumbar sciatica on the left are equally common, but bilateral lumbar sciatica is much less common. The pain is usually not as severe as with lumbago and the radicular stage of lumbar osteochondrosis (radiculitis). However, they are more intense than with chronic lumbodynia. Most often, the pain is severe or moderate in nature.
According to the subjective characteristics, it is aching, burning, squeezing, localized in the lower back or leg.
Symptoms
The main symptom of sciatica is severe pain, which is initially localized in the lumbar and sacral region, and as the disease progresses, it spreads along one, or less often, both lower extremities. The pain can be burning or dull, continuous or “shooting”, periodically occur in the form of attacks or be present all the time with variable intensity. The pain intensifies with movements of the spine, and in some cases, even a slight movement of the affected limb leads to a severe outbreak of pain.
In some patients, the pain is moderate, but tingling or numbness is felt in the limb or a certain area thereof. Some time after the onset of sciatica, individual muscle groups gradually weaken, which is why the patient has difficulty walking. In the most severe cases, nerve entrapment leads to problems with urination and defecation due to paralysis of the sphincter.
Are you experiencing symptoms of sciatica?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Vascular disorders in lumboischialgia
Vessels are narrowed
Studies have shown that the vascular tone of the legs in patients with lumboischialgia is most often increased. This is a vasospastic variant of this syndrome. In other words, the vessels are narrowed in this case.
And if vascular tone is increased, then patients note chilliness in the leg. She may be paler and colder to the touch than healthy. And the temperature in the lower leg and foot of the diseased leg is slightly lower than the healthy one. The most interesting thing is that after physical activity the temperature difference only increases. On the sore leg, the temperature drops even more, while under normal conditions it should rise. Temperature asymmetries are detected not only on sore and healthy legs. In some cases, even in a limited area of the affected leg, the temperature may be different at nearby points.
Vessels are dilated
When vascular tone is reduced, this is a vasodilatory variant of lumbar ischialgia syndrome. However, this manifestation is much less common. But if vascular tone is reduced, then a feeling of heat or warmth appears in the affected limb, and its temperature rises. (V. P. Veselovsky)
Prevention
- it is necessary to promptly treat diseases and get rid of problems in the joints, blood vessels, and spine;
- Avoid situations with hypothermia and injuries if possible;
- control of correct posture and weight control;
- wear comfortable shoes;
- you need to lift heavy objects correctly, and it is better to avoid lifting heavy objects;
- sedentary work requires a comfortable workplace, short breaks and warm-up for a few minutes;
- if the activity involves long car trips, you need to stop more often to warm up;
- lead a healthy active lifestyle;
- chronic lumbar ischialgia requires regular sanitary and spa treatment;
Any form of lumbar ischialgia requires a mandatory clinical examination. At the “Medical Center YES!” The neurologist, after examining and collecting anamnesis, will definitely prescribe additional instrumental and laboratory examination of the patient, necessary to assess the condition of the spine, bones and joints, in order to differentiate the disease, to identify, if any, pathologies of the blood vessels of the abdominal cavity and lower extremities . Additional studies help exclude fractures, tumor processes and other conditions and diseases.
Make an appointment with a neurologist at the “YES Medical Center!” possible by phone or by filling out the form on the website.
Our licenses for medical activities
All rights reserved by copyright law. No part of the contents of the site may be used, reproduced, transmitted by any electronic, copying or other means without the prior written permission of the copyright owner.
Autonomic disorders in lumboischialgia
When examining patients, a large number of autonomic disorders are determined. Initially, there is limited pallor of the nail phalanges of the toes. But in the future, the entire foot may turn pale. This process is often accompanied by a feeling of numbness, as well as other unpleasant sensations: burning, tingling, distension. In some cases, the pallor of limited areas of the skin of the leg is replaced by moderate cyanosis. These disorders are clearly identified after hypothermia, especially after work associated with high humidity.
Disc protrusion or herniation
Disc protrusion is a condition when the central gel-like part of the disc (nucleus pulposus) protrudes towards the spinal canal, while the integrity of the outer wall of the disc (annulus fibrosus) is not compromised. A disc herniation occurs when the nucleus pulposus extends beyond the annulus fibrosus. With protrusion or herniation of the disc, the protruding part of the disc can compress the adjacent nerve root and cause sciatica. The consequences of a herniated disc are worse. In this case, the prolapsed disc core not only causes direct compression of the nerve root, but at the same time the disc substance contains an acid, a chemical irritant (hyaluronic acid), which causes inflammation of the nerve. Nerve compression and irritation cause inflammation and pain, often leading to limb numbness, tingling, and muscle weakness.
Factors contributing to the occurrence of lumboischialgia
If a person is bothered by chronic vertebrogenic lumboischialgia, then diseases of various internal organs and the central nervous system are often detected. On the part of the central nervous system, these are, as a rule, residual effects of inflammatory and traumatic brain damage. Based on experimental studies, it has been established that the creation of additional foci of damage even outside the spine contributes to the occurrence of lumbar osteochondrosis. These lesions can be in the brain, muscles and internal organs. (V. P. Veselovsky)
Reflex curvature of the spine with lumboischialgia
In addition to pain and various autonomic disorders, patients with lumboischialgia often have reflex deformities of the lumbar spine. This manifestation is called antalgic scoliosis. It was believed that in most cases it was of a protective nature, as if helping to reduce irritation of the sinuvertebral nerve.
However, quite often, especially in young people, these curvatures remain for a long time, even after a significant reduction in pain. Therefore, reflex deformation of the spine cannot be considered as a physiologically useful mechanism. And also consider that this mechanism is aimed at reducing irritation of sensitive nerve formations, which are the source of pain. It would be more correct to say that there is vertebrogenic lumboischialgia with reflex muscular-tonic syndrome.
Treatment of lumboischialgia
Before talking about how lumbar sciatica is treated, it is important to note that drug treatment, physiotherapeutic procedures, and exercises for lumbar sciatica are best determined individually. And you need to proceed from the characteristics of each specific case and stage of the process.
- To relieve pain, drug therapy and physiotherapy are prescribed. If there are indications, then medical therapeutic blockades are used. They are performed by a doctor. The medicine is injected paravertebrally, as well as into trigger points on the sore leg. As a rule, droppers with decongestants and anti-inflammatory drugs are prescribed.
- It is recommended to fix the lumbar spine using an orthopedic semi-rigid dynamic corset. This also helps reduce pain, because it reduces the load on the spine.
- Functional disorders (blocks) in the functioning of the spine must be identified. This is done by a chiropractor. And this is necessary because it is the incorrect functioning of the spine that leads to the development of osteochondrosis, and ultimately to the appearance of protrusions and herniations of intervertebral discs. First, manual diagnosis is performed, and then manual therapy. Typically, there are an average of seven to ten procedures per course.
- In order to stimulate recovery processes, physiotherapeutic procedures, reflexology, and massage are prescribed.
- Physical therapy is very important.
The importance of physical therapy
Gymnastics for lumboischialgia should initially be aimed at eliminating muscle spasms. Equally - to relieve muscle swelling and venous stagnation in them and the roots of the intervertebral foramina. Ultimately, the goal of therapeutic exercise is to optimize the movement pattern. In other words, it is necessary to make the spine work more correctly, without overloading any of its segments. This is necessary to ensure that the disks do not fail prematurely. And new hernia protrusions did not appear in them, and old ones did not increase. All physical therapy should be built taking into account the individual characteristics of the patient. This is posture, features of the location of hernias and protrusions of intervertebral discs. Physical therapy exercises in combination with manual therapy are not only the prevention of relapses in chronic vertebrogenic lumbodynia. They are a prevention of the degenerative-dystrophic process (osteochondrosis of the spine), as such.
Impact of comorbidities
With the development of osteochondrosis, the formation of protrusions and hernias of the spine, concomitant diseases play an important role. This is, first of all, endocrine pathology: diseases of the thyroid and parathyroid glands, adrenal glands, as well as progressive diabetes mellitus. With lumbago, as a particular manifestation of osteochondrosis, it is necessary to check the condition of the kidneys. To do this, you need to perform an ultrasound of the kidneys, do a general blood and urine test.
The syndrome of chronic lumboischialgia is, as a rule, persistent. Constant pain in the lower back significantly limits the ability to work, if not completely deprives it. To prevent this from happening, treatment should begin as early as possible. Moreover, treatment measures must be comprehensive and the entire treatment process must be carried out under the supervision of a doctor.
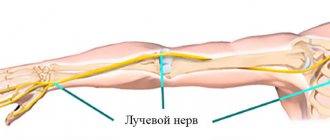
Piriformis syndrome
This syndrome is named after the piriformis muscle and pain is caused when this muscle irritates the sciatic nerve. The piriformis muscle is localized in the pelvic region, connects the femur and is involved in hip rotation. The sciatic nerve passes under the piriformis muscle. Piriformis syndrome occurs when this muscle spasms, thereby compressing the sciatic nerve. Due to the insufficient information content of X-rays and magnetic resonance imaging, diagnosing this pathology is difficult.