Craniopharyngioma is a rare type of brain tumor. It is localized in the pituitary gland. It is mainly first diagnosed in children aged 5-14 years or in adults over 40. The survival rate for craniopharyngioma for 10 years is about 90%. For a long time, the neoplasm does not manifest itself with any symptoms, but over time, multiple abnormalities develop: endocrinological, visual, hormonal.
Reasons for development
Craniopharyngioma develops due to excessive proliferation of epithelial cells in Rathke's pouch. It is formed in the fetus in the first trimester of pregnancy and is the basis for the future pituitary gland. If development occurs normally, then after the formation of the pituitary gland, Rathke cells are no longer produced. Craniopharyngioma appears only if this tissue continues to divide.
Typically, pituitary craniopharyngioma occurs due to a hereditary predisposition. A mutation of chromosomes occurs, which leads to the formation of a tumor. It can also occur due to intrauterine development disorders in the first trimester of pregnancy - this is when all the fetal organs are formed. This can be affected by taking medications, exposure to radiation, poisons and toxins.
Intrauterine infection and early severe toxicosis significantly increases the likelihood of craniopharyngioma. Chronic diseases of the mother, such as kidney pathologies, diabetes mellitus or tuberculosis, can contribute to the development of a tumor in a child.
Craniopharyngioma in children
Craniopharyngioma is uncommon in children. It is diagnosed in only 4% of all brain tumors. Typically, the first signs of the disease are diagnosed at the age of 5-14 years; craniopharyngioma occurs equally often in boys and girls. Initially, the pathology does not manifest itself with any obvious signs. Over time, the patient begins to complain of the following symptoms:
- Frequent headaches, worse in the morning;
- Nausea and vomiting;
- Delayed sexual and physical development;
- Violation of hormonal and endocrine functions;
- Change in behavior;
- Confusion;
- Visual impairment;
- Decreased appetite, increased thirst;
- Impaired motor functions;
- Increasing epilepsy;
- Swelling of the fundus;
- Altered psychopathological state.
Depending on the location of the tumor and its size, the manifestations of the disease may vary. It is important for parents to monitor the condition of their child, because timely diagnosed craniopharyngioma responds well to treatment.
Diagnosis of craniopharyngioma
Diagnosis of craniopharyngioma begins with a consultation with a neurologist and oncologist. Next, an X-ray of the brain is prescribed, which reveals the structure and erosion of its walls characteristic of the tumor, as well as corresponding changes in the structure of the sella turcica. Calcified tumors are clearly identified by such studies.
Laboratory tests are also performed to determine the concentration of hormones in the blood.
The tumor is diagnosed using MRI and CT scans of the pituitary gland of the brain, which allow one to see the layers of brain structures and determine not only the location of the craniopharyngioma, but also its size, which is extremely important.
Sometimes Dopplerography of cerebral vessels, as well as angiography of the brain and spinal cord, are prescribed.
To make an adequate diagnosis, craniopharyngioma should be differentiated from a number of other tumors with similar symptoms, for example, pituitary adenoma, glioma, colloid cyst of the third ventricle.
Craniopharyngioma in adults
Craniopharyngioma is a benign tumor in the brain. Usually it begins during embryonic development and is localized in the hypothalamic-pituitary region. Due to the growth of the tumor, numerous cysts often form, inside which fluid from proteins and cholesterol accumulates. In this case, the papillary form of craniopharyngioma is mainly diagnosed in adults.
Suprasellar and intrasuprasellar craniopharyngioma
The initial classification of craniopharyngiomas was developed by V. Grekhov at the Institute of Neurosurgery named after. Burdenko. In the future, it was repeatedly detailed and changed. Today it is customary to distinguish the following topographic variants of craniopharyngiomas:
- Suprasellar
. Such tumors grow within the sella turcica, displacing the diaphragm. They can spread supra- and parasellar. The neoplasm develops from the remnants of the epithelium, which is preserved at the level of the pituitary gland; - Stem
. They spread in the area of the pituitary gland stalk, gradually affecting the bottom of the 3rd ventricle. They are localized above the sella turcica, displacing its diaphragm down; - Intra-extraventicular
. They develop at the level of the pituitary infundibulum and spread into the cavity of the third ventricle. This type of craniopharyngioma is associated with the accumulation of embryonic epithelium in the infundibulum area.
Adamantimatous and papillary craniopharyngioma
Craniopharyngiomas vary in structure. They may contain cysts or consist of dense tissue. Cystic formations are characterized by slow growth, extremely rarely their diameter exceeds 5 centimeters. Typically, such tumors have up to 50 cysts, in rare cases their number reaches 200. The formation itself is dense, with a strong capsule, and quickly connects with brain tissue and blood vessels.
NB!
Under the influence of various factors, the tissue structure of craniopharyngioma can change.
If craniopharyngioma has been present in the body for a long time, there is a risk of necrosis. This contributes to the rapid formation of cysts. Inside they are filled with liquid with a high lipid content. Craniopharyngiomas can vary in cytological structure. The following types of such tumors are distinguished:
- Adamantine-like
. Occurs in most cases. Mostly diagnosed in children. A neoplasm of this type consists of remnants of embryonic tissue. They mainly consist of cysts. Adamantine-like craniopharyngiomas are characterized by polymorphism; - Papillary
. It is mainly diagnosed in people over 40 years of age, and practically never occurs in children. Such a tumor consists of metaplastic cells, with virtually no fossilization. Papillary craniopharyngiomas can consist not only of epithelial but also epidermal cells. In such tumors, degenerative processes occur and cysts and stroma develop.
Stages of development of transnasal removal of craniopharyngiomas
For a long time, using the transsphenoidal approach, we performed only intracapsular tumor removal
with initial growth within the sella turcica.
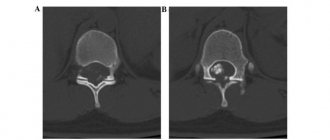
The endoscopic method was used for partial removal of the tumor and emptying of cysts in craniopharyngiomas with initial growth within the sella turcica - endo- and endosuprasellar craniopharyngiomas according to the classification developed and used at the Research Institute of Neurosurgery named after. N.N. Burdenko. When such tumors form within the sella turcica, the pituitary gland and the pituitary stalk are displaced posteriorly and upward. The cyst capsule lines the walls of the dilated sella turcica and, with suprasellar spread, displaces the sella diaphragm upward and fuses with it (Fig. 2).
Figure 2. Diagram of the anatomical relationships of endosuprasellar craniopharyngioma, sella turcica, pituitary gland and its stalk. 1 - solid part of craniopharyngioma; 2 - capsule of craniopharyngeal cyst; 3 - raised seat diaphragm; 4 - pituitary gland; 5 - stems of the pituitary gland.
For craniopharyngiomas of this anatomical variant, two removal options are possible:
1. Partial removal of the tumor and emptying of the cyst. It is also possible to partially remove the wall of the tumor cyst (subdiaphragmatically).
2. Radical removal of the tumor along with the wall of the cyst, including its upper part, fused with the remains of the sellar diaphragm.
For a number of years, we have used the first option for endoscopic removal of endo- and endosuprasellar craniopharyngiomas.
In the absence of intraoperative liquorrhea, at the end of such operations we left the bottom of the tumor cyst open in the expectation that its contents would flow into the main sinus. Unfortunately, these operations usually provided a temporary effect - the walls of the cyst closed the defect formed by the surgeon at different rates. In Fig. 3
Figure 3. Example of a stable craniopharyngioma after transnasal voiding. a — MRI before transnasal surgery; b — MRI 1.5 years after transnasal surgery. The size of the cyst does not exceed the preoperative size; c — MRI 2.5 years after transnasal surgery. The size of the cyst did not change over time. A rare observation is presented when, within 2.5 years after transnasal opening of the walls of a craniopharyngioma, its reaccumulation was not observed.
More often, reaccumulation of tumor cavities occurs.
Attempts to install drainage into the cyst cavity
during transnasal operations were ineffective.
Over time, the drainage tube became completely embedded in the dense scar (Fig. 4).
Figure 4. Transnasal drainage of cystic craniopharyngioma. a — diagram of installation of a drainage tube in craniopharyngioma cysts; b — intraoperative photo — scar tissue in the lumen of the drainage tube.
Radical operations
, in which the tumor capsule is completely removed, are so far the only effective treatment method.
During transnasal endoscopic operations, radical removal of craniopharyngiomas became possible due to improved visualization of the surgical field and panoramic view, which provided the possibility of a complete examination of all parts of the tumor (Fig. 5).
Figure 5. Areas of accessibility of craniopharyngiomas during endoscopic transnasal removal.
a — accessibility of the tumor in the sagittal plane with extended access; b — an example of the possibility of removing a tumor located on the clivus without resection of the dorsum sella and clivus; c — accessibility of the tumor in the axial plane. Removal of endosellar
craniopharyngiomas, when the tumor capsule is separated from the dura mater of the walls of the sella turcica and the diaphragm, does not present significant difficulties. Often, during such operations, the pituitary gland stalk, and often the pituitary gland itself, remains intact and is not functionally affected. Usually, during such operations, a defect is formed in the remnants of the saddle diaphragm, but its dimensions are, as a rule, small and its plastic surgery does not cause significant difficulties.
Radical removal of suprasellar
Craniopharyngiomas (stem and infundibular - intra-extraventricular craniopharyngiomas) became completely possible after the introduction of expanded approaches, in particular the anterior one, into practice [3]. Resection of the anterior wall of the sella turcica and the posterior sections of the sphenoid bone platform allows one to obtain a good panoramic view of the chiasmatic region. Available for removal are tumors located from the middle of the main bone area in front to C1 in the back, between both carotid arteries and extending into the cavity of the third ventricle up to the foramina of Monroe. The beginning of the use of expanded approaches has shown that in most cases it is possible to preserve numerous small arterial vessels supplying the basal parts of the chiasm and the diencephalic region.
Most retrochiasmally located craniopharyngiomas are accessible to transnasal removal, which has recently made this technique the “method of choice.” It also became clear that in most cases, such tumors are formed both from the stem of the sella turcica (often its upper third) and from the infundibulum area (Fig. 6).
Figure 6. Various variants of the relationship between the pituitary stalk and the tumor. a — observation 1. Small craniopharyngioma (2), actually adjacent to the pituitary gland stalk (1) and not destroying it. The pituitary gland (3) is intact; b — observation 2. Craniopharyngioma (2), forming in the infundibulum area of the hypothalamus. Stem (1) is shortened, but preserved. The pituitary gland (3) is intact; c — observation 3. Craniopharyngioma (2), forming in the region of the hypothalamic infundibulum and the proximal parts of the stalk (1), which is visualized, but sharply reduced. The pituitary gland (3) is intact; d — observation 4. Craniopharyngioma forming in the pituitary gland stalk. The tumor (2) is located directly above the pituitary gland (3) and is surrounded by a thin layer of tissue from the pituitary stalk (1). In almost all such observations, in order to mobilize the tumor and completely remove it, we had to completely transect the stem or its remains.
To remove craniopharyngiomas, we use both standard instruments from the endoscopic set and those modified by us.
To separate the tumor capsule from the basal parts of the chiasm and the bottom of the third ventricle, it is necessary to use suction, microdissectors, pliers with significant bending angles and a significant length of the working part, as well as microscissors of various shapes. Very often, two surgeons have to work - one tightens the tumor capsule with pliers, the second, using various dissectors and curettes, gradually separates the capsule from the brain structures and vessels. Destruction of petrification of various densities and removal of dense tumor fragments in most cases is impossible without the use of an ultrasonic destructor. We use a device manufactured by Soring, equipped with a long thin tip and a set of protective attachments on them.
As a result of careful separation of the tumor from the remains of the bottom of the third ventricle in the postoperative period, intellectual-mnestic and endocrine disorders occur rarely and are less pronounced. In our series of observations (56), out of 30 patients who did not have pituitary insufficiency before radical tumor removal using an extended endoscopic approach, it appeared in 19 (63.3%). Elements of Korsakoff's syndrome, which were initially detected in 7 (12.5%) patients, regressed in 6 (85.7%) of them. High detail of the surgical field during endoscopy allows you to clearly see the “glial” capsule of craniopharyngioma - the area where the tumor capsule passes into the medulla without a clearly defined boundary, and to separate the capsule from the medulla (Fig. 7).
Figure 7. Identification of infiltration of structures of the diencephalic region.
a, b — MRI before surgery; c — intraoperative photo: 1 — medulla of the basal surface of the chiasm; 2 - “glial” capsule; 3 - tumor capsule; 4 - anterior edge of the chiasm; 5 — lateral wall of the third ventricle with single petechial hemorrhages, after separation of the tumor capsule; d — histological preparation of the “glial” capsule (zone 2 of Fig. c): 1 — medulla; 2 - “glial” capsule; 3 - tumor tissue. In addition, in most cases, it is possible to preserve most of the thinnest vessels that provide blood supply to the basal surface of the chiasm, the bottom of the third ventricle, the infundibulum and the pituitary stalk. In most cases, it is possible to separate the vessels from the tumor without the use of coagulation (Fig. 8).
Figure 8. Possibilities of preserving blood supply to the diencephalic region during transsphenoidal endoscopic removal of craniopharyngiomas. a—c—case 1: a—MRI before surgery; b — intraoperative photo. The arrows indicate the preserved numerous arterial vessels supplying the basal surface of the chiasm and the diencephalic region; c — MRI control 4 months after tumor removal. d—f — observation 2: d — MRI before surgery; d — intraoperative photo. The arrows indicate the preserved arterial vessels in the arachnoid membrane, supplying the basal surface of the chiasm and the diencephalic region. 1 — tumor capsule separated by an instrument; 2 - posterior communicating artery; e - no MRI after surgery. g—i — observation 3: g — MRI before surgery. The area of heterogeneity in the posterior parts of the tumor is petrified; h — intraoperative photo. The arrows indicate the preserved arterial vessels supplying the diencephalic region (2). 1 - tumor; 3 - left posterior communicating artery; 4 - left oculomotor nerve; and - MRI control 4 months after tumor removal.
During such operations, the optic nerves and chiasma experience virtually no serious traction, and in most cases, the visual impairment is transient. In our material, vision deterioration occurred in only 6 (12.8%) of 56 patients. Of the 47 (83.9%) patients who had visual impairment, improvement occurred in 27 (57.5%).
It is not possible to completely remove the craniopharyngioma capsule in all cases. In our series of observations, radical tumor removal was achieved in 39 (69.6%), and in the remaining 17 (30.4%) the removal was subtotal.
In some cases, when the capsule thins to the state of a thin film resembling the arachnoid membrane, it becomes impossible to separate it from the structures of the chiasmal region. This creates the preconditions for tumor recurrence and determines the indications for stereotactic irradiation (Fig. 9 and 10).
Figure 9. An example of subtotal removal of a craniopharyngioma followed by radiation therapy to the area of the remaining cyst capsule. a, b — MRI before surgery. Craniopharyngioma of heterogeneous structure is a combination of solid and cystic components; c — diagram of visual fields before surgery. Chiasmal syndrome is represented by bitemporal hemihypopsia and central scotoma on the left; d — intraoperative photo. The stage of separation of the solid part of the tumor (1) from the basal surface of the left optic nerve (2), left posterior communicating artery (3), left oculomotor nerve (4). Traction is performed with a curved suction (5); d — intraoperative photo. The stage of separating the solid part of the tumor (1) from the basal surface of the chiasm (4) with an instrument (5). During tumor traction, a pituitary stalk (2) was discovered reaching the upper pole of the gland (3); e — intraoperative photo. The posterior sections of the tumor were represented by a cyst, the walls of which (1) resembled a thin translucent film, which could not be separated. Large image of the cyst capsule before its opening. Small image - the capsule of the cyst is opened (the edge of the capsule is indicated by arrows), which made it possible to see the cavity of the third ventricle (2); g, h — MRI control 3 months after surgery. In image g, arrows and a yellow dotted line indicate the remainder of the tumor and its capsule; and - diagram of visual fields after tumor removal. Bitemporal hemihypopsia persists. The central scotoma OS regressed; j — MRI before irradiation; k - diagram of the distribution of dose curves during irradiation on the Novalis device; m - MRI control 3 months after the end of irradiation. The size of the cyst has decreased somewhat, its capsule is clearly thickened.
Figure 10. Scheme of multilayer plastic “sandwich” type (explanation in the text). 1 - dura mater; 2 - bone base of the skull; 3 — fibrin sponge TachoComb; 4—fascia fragment; 5 — bone fragment; 6 — autologous adipose tissue; 7 - adhesive composition.
A separate problem when removing craniopharyngiomas is the need to remove petrificates of different configurations, sizes and densities. Small and large “loose” petrificates can usually be completely removed; we often use an ultrasonic destructor for this. However, due to the peculiarities of sound wave propagation, an ultrasonic destructor with a curved working part has not yet been created, and because of this, the removal of dense tumor fragments located outside the direct field of view turns out to be very difficult. In 2 observations, large coral-shaped ossifications could not be removed due to close fusion with the formations of the chiasmal region and due to the fact that they did not lend themselves to either chunking or ultrasonic destruction.
Removal of the tumor from the suprasellar space and from the ventricular system determines increased requirements for hemostasis. To stop and prevent bleeding from small capillaries, we use the drug SurgiFlow. To stop bleeding from small arteries and veins, we used hemostatic gauze Surgicel and Sergicel fibrilar. To close defects in large vessels and strengthen their walls, we actively use the drug TachoComb.
Unfortunately, at present there are no “convenient” - delicate and at the same time durable bipolar coagulation instruments. For coagulation, we have to use monopolar coagulation suctions, both straight and curved in different directions.
Of particular importance when performing radical transnasal operations is reliable plastic surgery of significant defects of the skull base to prevent postoperative nasal liquorrhea. For the same purpose, we used various adhesive and hemostatic materials, used lumbar drainage, and used autologous tissues, in particular autologous tissues with preserved blood supply [4]. Currently, we consider the optimal option to be “multilayer” plastic, when a so-called “sandwich” is formed from the above materials in various combinations.
We expose the walls of drained cysts or unremoved tumor fragments to stereotactic irradiation. Depending on the size and location of the tumor, three radiation options are used:
— stereotactic radiosurgery with a total focal dose (FOD) of 10-15 Gy;
— stereotactic radiotherapy in the hypofractionation mode with a single focal dose (SOD) of 5 Gy up to a SOD of 25 Gy;
— stereotactic radiotherapy in the standard fractionation mode with ROD 1.8-2 Gy to ROD 50-54 Gy.
Stereotactic irradiation in the treatment of craniopharyngiomas has proven to be very effective. Since 2005, 120 patients have undergone stereotactic radiation at the institute. Currently, follow-up is known in 80 (66.7%) patients. A significant reduction in tumor size was detected in 22 (27.5%) patients, and in 42 (52.5%) the tumor remained stable. Only 18 (22.5%) patients had tumor progression.
Discussion
Improvements in endoscopic techniques in recent years have significantly changed the results of operations. Craniopharyngiomas extending beyond the sella have become available for transnasal excision. At the same time, the method of their removal began to resemble the general principles of transcranial microsurgery - dissection of the tumor and brain structures, microdissection of the vessels surrounding the tumor, tumor removal using an ultrasonic disintegrator. A distinctive feature of the described surgery is the almost complete absence of gross traction of the visual pathways and structures of the diencephalic region, which significantly improves the functional outcome of the operation and reduces the risks of developing severe diencephalic lesions.
As already mentioned, not in all cases it is possible to completely remove the craniopharyngioma capsule, which creates the preconditions for relapse. Analysis of the institute's material, carried out in 2000 by Zh.B. Semenova, established a high rate of recurrence of craniopharyngiomas, primarily adamantinoma-like ones, which depends on the radicality of tumor removal and its biological activity. On average, tumors recurred after total and subtotal removal in 21.5% of patients, and after partial removal in 53.2%. The recurrence rate of papillomatous craniopharyngiomas is 7.8% [5]. Similar data are presented in many series of observations and, first of all, in the generalized experience of French neurosurgeons M. Choux and G. Lena [9].
The main reason for non-radical removal is the infiltrative growth of the tumor and its prevalence. The biological activity of the tumor is of greater importance in the occurrence of tumor relapse.
In a large series of observations at the institute, the significance of various tumor growth markers (Tenascine, KI-S1, PCNALI, Ki-67, CerebB2, p53, EGFR) was studied. Only the level of Ki-67 in the tumor was significant in the occurrence of craniopharyngioma relapses.
Conclusion
What can we expect in the development of this problem in the future? First of all, further improvement of the transsphenoidal approach and its wider use for craniopharyngiomas of various locations. Obviously, clarifying the indications and optimizing radiation regimens will reduce the recurrence rate of these tumors if they are not radically removed. Generalization of the existing fragmentary data on the morphology of craniopharyngiomas as a result of studying large groups of patients, possibly as a result of multicenter studies, will allow us to identify new, more significant criteria for tumor aggressiveness.
A comment
The work, prepared by a large team of authors, is devoted to describing the basic principles of transsphenoidal surgery for craniopharyngiomas. The article reflects the stages of the long journey traveled at the institute. Over the past 8 years, there has been a radical change in approaches to the surgical treatment of endosellar and endosuprasellar craniopharyngiomas - intracapsular removal of the tumor, performed under a microscope, was replaced by radical removal of the tumor and its capsule, performed under endoscopic control. The authors demonstrated the possibility of removing tumors reaching the foramen of Monro, previously inaccessible for transnasal removal. The work presents the general principles of the technology used, the first results obtained, confirming at least its safety. The volume of the authors' material already exceeds the series of most world centers. Further improvement of surgical techniques and a detailed analysis of the results, including errors and complications, should certainly be reflected in subsequent published works.
A.Yu. Grigoriev
(Moscow)
Symptoms
Craniopharyngioma of the pituitary gland is characterized by the development of endocrine and metabolic disorders, and intracranial hypertension syndrome. Because of this tumor, the balance of many hormones in the body is disrupted: gonadotropin, LH, ACTH, STH. This leads to the development of hypothyroidism, hypogonadism, hypocortisolism, and diabetes insipidus. Over time, hypothalamic-pituitary disorders occur, such as:
- Constant feeling of thirst;
- Polyuria, enuresis;
- Developmental delays, decreased growth rates in children;
- Rapid increase in body weight;
- Increased fatigue, muscle weakness;
- Menstruation irregularities, decreased libido.
The severity of such deviations depends on the location of the craniopharyngioma, its size and the age of the patient. Early symptoms of a tumor also include visual disturbances: decreased visual acuity, development of blindness. If the tumor is located in the third ventricle and compresses its openings, intracranial pressure increases - the patient complains of a constant headache.
NB!
The intensity of manifestation of pituitary craniopharyngioma depends not only on the size and location of the tumor. If the tumor is large, but it does not compress neighboring areas, the symptoms of the pathology may be minor.
2. Symptoms of the disease
Like many brain tumors, craniopharyngioma can be asymptomatic and discovered incidentally. It begins to manifest itself only when it reaches a certain size - more than three centimeters in diameter. In this case, the tumor begins to put pressure on brain structures or interfere with the normal circulation of cerebrospinal fluid, which causes the manifestation of certain symptoms. In addition, this tumor, despite its slow growth, is quite insidious, because tends to infiltrate into the tissue of the pituitary gland (which affects the production of hormones), cerebral arteries, optic nerve and chiasm.
The symptomatic picture of craniopharyngioma may look like this:
- headaches, fainting;
- delayed growth and puberty;
- menstrual irregularities;
- decreased sex drive;
- obesity;
- dry skin;
- fatigue, hypotension, depression;
- constipation
Visit our Neurosurgery page
Diagnostics
To diagnose craniopharyngioma, several studies are performed at once. This helps determine the possible cause of the pathology, its exact location, and the degree of damage to surrounding tissues. Standard diagnosis of craniopharyngioma includes the following measures:
- Anamnesis collection, visual examination of the patient
. The doctor will learn about the symptoms that concern the person, clarify the general state of health, and the presence of risk factors; - Biochemical and general blood tests
. Determine the concentration of vital blood components; - General urine analysis
. Determines kidney function, rate of urine excretion; - Hormonal blood test
. Determines the content of biochemically active substances and identifies deviations from the norm. The test allows you to diagnose endocrine disorders; - Neurological examination
. The function of the brain, spinal cord, and nerve endings is assessed. The doctor needs to check the person’s muscle strength, memory, vision, hearing, reflexes, and coordination; - CT and MRI
. Diagnostic imaging techniques that provide accurate images of the brain. This helps determine the size and location of the tumor and what tissues it has affected. MRI when determining pituitary craniopharyngioma gives a clearer picture; - Biopsy
. The most accurate examination method for craniopharyngioma. A portion of the tumor is removed using a needle for further histological examination. This determines the exact nature of the tissues.
NB!
When diagnosing pituitary craniopharyngioma, blood and urine tests are of high diagnostic value. Your doctor will need to check your electrolyte levels to help diagnose diabetes insipidus. It is also necessary to exclude germ cell tumors, for which the levels of alpha-fetoprotein (α-FP) and beta human chorionic gonadotropin (β-hCG) are determined.
3.Diagnosis of the disease
Diagnosis of tumors is carried out using magnetic resonance imaging (MRI) and computed tomography (CT)
.
In addition, hormonal studies
and plain
radiography of the skull
. A set of studies allows us to determine the exact location and size of the tumor, its structure and the degree of infiltration into the tissue of neighboring brain structures.
About our clinic Chistye Prudy metro station Medintercom page!
Treatment
The basic treatment for pituitary craniopharyngioma is chemotherapy. It is carried out both as the main part of therapy and as an auxiliary part during surgical excision of the tumor. The radioactive drug is injected intravenously or into the spinal canal (in the case of surgical removal of a tumor, in its bed). Craniopharyngiomas cysts are filled with interferon preparations: they have a cytotoxic effect. Due to this, the process of self-destruction of tumor cells is started.
Craniopharyngiomas are prone to recurrence. And even after surgical interventions, many patients may develop a new formation within the first year. Because of this, they always undergo postoperative radiation therapy, which reduces the risk of such a consequence by 2 times. Today, the following methods show the greatest effectiveness in the treatment of pituitary craniopharyngiomas:
- Proton therapy
. Heavily charged particles are used that release all the energy into the tumor. Due to such targeted irradiation, it is possible to stop the growth of the tumor and also destroy some of the cells. The advantage of this technique is its highly precise action: the surrounding brain tissue is not irradiated; - Intracavitary radiotherapy
. This is one of the methods of radiotherapy in which the radiation source is located directly in the tumor. This avoids damage to the cranial nerves, blood vessels, pituitary gland and hypothalamus.
Therapy for pituitary craniopharyngioma in children
If pituitary craniopharyngioma is detected in children under 3 years of age, and the tumor is accompanied by the spread of numerous cysts, then a catheter is implanted in the pituitary gland area. Drainage of the cyst is organized, due to which its size is reduced. Nearby tissues and blood vessels are no longer compressed, and the symptoms of the pathology disappear.
Cyst catheterization is a minimally invasive method for treating pituitary craniopharyngioma. To increase the accuracy of the intervention, stereotactic settings are used. To remove cysts, a sclerosing agent may be injected into them. The walls of the tumor stick together, the tumor stops accumulating fluid. This technique is used exclusively in young children; in the future, more radical intervention is necessary: radiation therapy or surgical excision.
In older children, craniopharyngiomas are removed with a gamma knife. This is one of the methods of stereotactic radiosurgery, characterized by extreme targeting accuracy. High-dose radiation therapy is performed to remove the tumor. In this case, the surrounding tissues are not affected.
Types of operations to remove craniopharyngioma
Surgical treatment is the most effective method of treating cerebral craniopharyngioma
. The operation is quite complex: it has technical difficulties due to limited accessibility to the tumor. There is also a risk of damage to the pituitary gland, optic nerves, carotid arteries, and the floor of the third ventricle - all of these tissues are located in close proximity. The surgeon needs to remove all tumor tissue and not affect healthy cavities.
Radical tumor removal reduces the risk of relapse by up to 20%. In the future, postoperative radiation therapy can minimize the likelihood of future tumors. Currently, the following surgical techniques are used for pituitary craniopharyngioma:
- Surgery with craniotomy access with traditional opening of the cranial bones
. All manipulations are determined in advance using computer planning. This allows the operation to be performed as carefully as possible, preserving all surrounding tissues and formations; - Operation with transsphenoidal approach
. This is an endoscopic type of intervention. Small incisions are made under the nose and sinuses of the sphenoid bones, through which a neuroendoscope is inserted into the brain cavity. This minimally invasive intervention is easier for patients to tolerate and the rehabilitation period is shortened. But it must be taken into account that not all craniopharyngiomas are suitable for such an operation. Interventions with a transsphenoidal approach are performed only when the tumor is located suprasellar.
4. Treatment of craniopharyngioma
Treatment of craniopharyngioma
usually done through surgery. The purpose of the operation is radical excision of the tumor, which eliminates compression of the pituitary gland and normalizes its function in producing hormones.
For suprasellar localization of craniopharyngioma, surgery is usually performed via a transcranial approach using craniotomy. However, if the size and location of the tumor allow, it is possible to perform a more gentle operation using the transsphenoidal endoscopic method. This type of surgery is performed using innovative endoscopic equipment through the nasal passages.
. This intervention is less traumatic for the patient, it allows him to recover in a shorter time and reduces the risk of possible postoperative complications.
If the tumor is difficult to reach or surgery is contraindicated for the patient, treatment with stereotactic radiation therapy
, allowing extremely precise targeting of the beam gun to the tumor area without damaging adjacent tissues.
Postoperative changes after removal of craniopharyngioma
Almost all patients with craniopharyngioma experience complications that impair quality of life. Such consequences can arise either due to the tumor itself or as a result of treatment. Patients often encounter the following problems:
- Loss of vision;
- The appearance of mood swings;
- Emotional disorders;
- Memory impairment;
- Endocrine dysfunction;
- Development of metabolic syndrome;
- Pathologies of blood vessels.
The pituitary gland is the main gland in the human body. It is she who is responsible for the production of basic hormones, and also controls the work of other organs and endocrine glands. If a person's pituitary gland function is impaired, multiple problems arise: obesity, decreased bone mineral density, deterioration of the lipid profile, decreased fertility. This often occurs even in those patients who adhere to hormone replacement therapy.
Due to damage to the hypothalamus, multiple hormonal changes also occur. And this affects the quality of life. The patient begins to complain of increased appetite, his body weight rapidly increases, his behavior changes, and his personality becomes emotional. Metabolic syndrome often develops - a group of disorders accompanied by obesity, elevated levels of triglycerides and cholesterol, and high blood pressure. Metabolic syndrome significantly increases the likelihood of strokes and heart attacks.
In most cases, treatment for pituitary craniopharyngioma requires surgery or radiation therapy. After such events, the likelihood of disorders of the blood vessels of the brain increases significantly. The risk of aneurysms and stroke increases, seizures and cognitive impairment often occur.
Due to the high risk of complications associated with pituitary craniopharyngioma, the patient must be under constant medical supervision. Only timely diagnosis will make it possible to identify the deviation at the initial stages and stop it. Social and psychological assistance will help improve the patient's condition. The specialist will tell the person how to competently cope with the experience, how to get rid of anxiety and minimize the risk of depression.
Prognosis and prevention
At the moment, doctors have not developed an unambiguous system for determining the stage of craniopharyngioma. The tumor can be newly diagnosed or recurrent. This is a benign neoplasm that is not prone to spreading to other parts of the brain. Despite this, they can cause numerous abnormalities in the body’s functioning: disruption of endocrine functions, damage to the optic nerve.
The 10-year survival rate for patients with pituitary craniopharyngioma is 90%. With adequate treatment, it is possible to preserve both the quality and life expectancy of the patient. If after radiation therapy the tumor continues to progress, they are completely removed.
It is impossible to completely protect yourself from pituitary craniopharyngioma. The disease has a hereditary predisposition. The only way to reduce the likelihood of developing pathology is to prevent the exacerbation of diseases in the mother during pregnancy, avoid self-medication with medications, and protect against the influence of toxins and poisons.
conclusions
Craniopharyngioma is a benign neoplasm of the pituitary gland. Mostly occurs in children 5-14 years old. The disease develops due to disorders that occur in the fetus in the first trimester of pregnancy. In the initial stages, it is difficult to diagnose, because the pathology does not manifest itself with any symptoms for a long time. Treatment for pituitary craniopharyngioma is mainly surgical.
If you suspect pituitary craniopharyngioma in yourself or cannot recover from this disease, then feel free to contact the doctors of our medical center. They will conduct extensive diagnostics, develop an individual treatment regimen and monitor all stages of therapy.
Histological picture
1. Adamantinoma-like (about 85% of all craniopharyngiomas) - more common in patients of childhood and adolescence. They differ in polymorphism and can have a compact (10%), cystic (30%) and mixed (60%) structure.
2. Papillomatous (15% of all craniopharyngiomas) - unlike adamantine-like ones, this pathology is diagnosed more often in people in adulthood, usually at 30-40 years of age. These tumors are mostly solid, with little or no petrification