Raynaud's disease is one of the most mysterious diseases that affects about 5% of the world's population. It was first described in 1862 by French physician, scientist and educator Maurice Raynaud , who observed a girl suffering from sudden attacks of numbness in her limbs. Based on an analysis of five similar cases, the author concluded that these symptoms belonged to a new, previously unknown disease, and described in detail all its symptoms.
The disease manifests itself as sudden attacks of spasm in the small arteries of the arms and/or legs, and sometimes in other peripheral parts of the body - the tip of the nose and ears. As a result, blood ceases to flow in sufficient quantities to the cells of these parts of the body, leading to the development of so-called ischemia (bleeding). As a rule, this is preceded by hypothermia or severe stress. As the disease progresses, it can eventually lead to a serious complication - gangrene of the fingers.
Most often, the disease occurs in residents of cold climates and mainly affects middle-aged people (40-50 years old). Raynaud's syndrome occurs 4 times more often in women than in men.
1 General blood test
2 Diagnosis of Raynaud's syndrome
3 Diagnosis of Raynaud's syndrome
When talking about this disease, we mean two types of pathology: Raynaud's disease and Raynaud's syndrome .
Raynaud's disease is considered an independent disease with an unknown cause.
Raynaud's syndrome may be a manifestation of any other underlying diseases. When they talk about Raynaud's phenomenon, they most often (in most patients) mean Raynaud's syndrome. And only 15% of patients have an independent disease with the same name.
A mandatory sign of this disease is symmetrical damage to the limbs.
Causes of Raynaud's syndrome
Raynaud's syndrome can be a consequence of the following diseases and factors:
- various autoimmune connective tissue pathologies (systemic scleroderma, rheumatoid arthritis, systemic lupus erythematosus);
- inflammatory diseases of blood vessels - systemic vasculitis (granulomatosis or Wegener's disease, polyarteritis nodosa, drug-induced vasculitis, cryoglobulinemic vasculitis);
- blood diseases (thrombophlebitis, thrombocythemia, cryoglobulinemia, leukemia);
- diseases of the endocrine system (pathology of the adrenal glands and thyroid gland);
- hypothermia, stress, emotional overstrain;
- long-term use of medications that have a vasoconstrictor effect (migraine medications).
Treatment
When symptoms of Raynaud's disease appear, treatment can be divided into two groups - conservative and surgical. Conservative methods include the use of vasodilators (eg, phentolamine). Drug therapy for Raynaud's disease continues throughout the patient's life. It should be noted that with long-term use of these drugs, complications inevitably occur. When attacks of vasospasms of the extremities become insensitive to vasodilators, surgical treatment of Raynaud's disease is recommended - sympathectomy. It involves removing or stopping the nerve fibers of the sympathetic trunk that cause spasms of the arteries. Endoscopic sympathectomy is considered the least traumatic type of surgical treatment for Raynaud's disease. During it, the patient, under general anesthesia, has a clip applied to the sympathetic trunk in the chest or neck area. An important component of the treatment of Raynaud's disease is limiting the patient's contact with provoking factors. If there is a high negative emotional load, you should take sedatives. If you need to come into contact with a cold and damp environment, you should dress warmer than usual, especially carefully insulate your hands and feet.
Symptoms of Raynaud's disease
Symptoms of the disease can begin quite suddenly, for example, after doing laundry or washing dishes in cold water, walking in the cold, sometimes after exposure to stress. Most often, 2-5 fingers and toes are affected, in more rare cases - other protruding parts of the body: ears, nose, chin and even tongue.
The attack is manifested by a sharp pallor of the fingers, they become white and very cold, then the skin color acquires a bluish tint, and after the end of the attack, the fingers become purple-bluish and painfully hot and swollen.
Over time, attacks become more frequent, can occur for no reason, and their duration increases to 2 hours.
Due to poor nutrition of the skin, the pads of the fingertips become flattened, the skin becomes dry, begins to peel, and hard-to-heal ulcers may appear around the nails. In severe cases, tissue necrosis can also begin - dry gangrene.
Examination of capillaries (capillaroscopy) in patients suffering from Raynaud's syndrome often does not reveal significant changes.
Clinical picture
Rhine disease belongs to the group of vegetative-vascular pathologies and is characterized by paroxysmal nature. Against the background of vascular spasms, the blood supply to the extremities, and sometimes to the areas under the knees, the tip of the nose, chin, and ears, is most often disrupted. The pathological condition is not considered rare, since the syndrome is observed in 5% of adults on the planet.
The pathological condition can be provoked by stress, psychological tension, decreased ambient temperature and other factors. The syndrome can also develop against the background of:
- Endocrine disorders.
- Alcoholism and other addictions.
- Disorders of hematopoietic processes.
- Spinal diseases.
- Autoimmune diseases.
- Finger injuries.
A characteristic feature of the pathological condition is the symmetry of symptoms. Most often, the syndrome develops as follows:
- The extremities gradually become cold.
- There is pain, aching and burning in the arms and legs.
- The skin turns pale and appears blue.
Diagnosis of Raynaud's syndrome
Since Raynaud's syndrome often occurs against the background of rheumatic and autoimmune diseases, laboratory research methods aimed at identifying them become important. The following types of tests are taken (for more details, see rheumatological examination):
- general blood test (increased ESR, decreased hemoglobin, leukopenia and thrombocytopenia are important);
- biochemical blood test (with Raynaud's syndrome, significant changes, as a rule, are not detected);
- coagulogram;
- general urine analysis;
- immunological blood tests (level of immunoglobulins, rheumatoid factor, cryoglobulins, various autoantibodies, for example, antinuclear antibodies, antibodies to DNA).
1 Treatment of Raynaud's disease
2 Reflexology (acupuncture)
3 Treatment of Raynaud's disease
Diagnostics
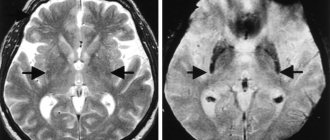
A patient with Raynaud's syndrome is referred for consultation with a rheumatologist and a vascular surgeon. In case of Raynaud's syndrome, changes in the distal parts of the arteries can be detected by angiography of the peripheral vascular bed, which identifies areas of uneven stenosis and total vascular obstruction, the absence of capillary networks and collaterals. Capillaroscopy of the nail bed and anterior surface of the eye reveals morphological changes in the microvascular pattern, indicating impaired perfusion. Laser Doppler flowmetry, used to assess peripheral microcirculation, reveals defects in the metabolic and myogenic regulation of blood circulation, a decrease in veno-arterial reactions and sympathetic activity. In the period between attacks with Raynaud's syndrome, a cold test can be used to provoke vasospasm and assess the state of blood flow.
Treatment of Raynaud's disease
Modern medical capabilities make it possible, if not to cure completely, then to significantly reduce the severity of the symptoms of Raynaud's disease. They use medication, physiotherapy, reflexology (acupuncture). Treatment of diseases that lead to the development of symptoms of Raynaud's syndrome is important.
Measures to prevent exacerbation of Raynaud's disease:
- to give up smoking;
- prevention of hypothermia (try not to overcool your hands, feet and face, dress according to the weather, make sure your shoes are dry, wear mittens in winter, etc.);
- adherence to sleep and rest patterns.
Highly qualified rheumatologists at MedicCity will help you cope with the manifestations of various rheumatological diseases. Our clinic diagnoses and treats rheumatoid arthritis, ankylosing spondylitis, reactive arthritis, gout, osteoarthrosis, osteoporosis, Sjogren's disease, systemic lupus erythematosus, systemic vasculitis, dermatomyositis, systemic scleroderma, rheumatism, etc. The most modern treatment methods are used. Trust the professionals!
Stages of the disease
An attack of Raynaud's syndrome, in most cases, lasts 15-20 minutes, after which the blood supply is restored. In this case, the skin immediately becomes purplish-red, which is associated with reactive hyperemia.
The severity of the signs of Raynaud's syndrome depends on the stage of the pathology:
- The first stage is angiospatic. It is characterized by short attacks (up to a couple of minutes), which occur as a response to exposure to low temperatures or psychogenic effects. The person becomes cold and pale, and also experiences a slight tingling sensation, minor pain and a slight burning sensation. When exposure to irritating factors ceases, the condition quickly recovers. As the disease progresses, attacks become more frequent.
- The second stage is angioparalytic. It is diagnosed approximately six months after the onset of the first attacks. The duration of attacks increases to an hour, and susceptibility to low temperatures also increases. Additionally, attacks are accompanied by cyanosis of the skin and swelling of the tissues. The pain becomes more intense. The intervals between attacks are shortened. It may take several years for the condition to stabilize.
- The third stage is trophoparalytic. It develops approximately 1–3 years after the onset of the disease. Symptoms during attacks are pronounced. Additionally, trophic disorders appear on the skin: ulcers, conflicts, etc. Deterioration in the condition of the nails may also occur. Intolerance to exposure to low temperatures increases. Constant pain leads to physical exhaustion. In severe cases, the fingers and toes become thicker and take on a bluish tint. Their mobility is impaired. With the development of trophic changes, there is a risk of tissue necrosis.
Causes
The main role in the development of the disease is a predisposition to it, including hereditary one. Among the diseases and risk factors that predispose to the development of Raynaud's disease, the following conditions should be distinguished:
- Episodes of hypothermia of the extremities, trauma to the fingers.
- Endocrinological disorders.
- Psycho-emotional overload.
- Vibration disease, labor associated with vibration.
- Rheumatological pathology.
- Migraine.
3. Symptoms, diagnosis
The disease usually manifests itself at the age of 20-30 years; cases of primary diagnosis in children or people over 50 years of age also occur, but much less frequently.
The clinical picture of neurovascular spasm must be considered in the context of a specific stage, since it varies significantly at different stages.
So, at the beginning of the course of Raynaud's disease/syndrome, the color changes paroxysmally and in strict situational dependence (in fact, the skin becomes discolored, then acquires a cyanotic tint) and the temperature of the fingers decreases. As vasculature (blood supply) is restored, appearance and temperature are also restored, but the patient may feel characteristic “pins and needles”, numbness of the phalanges, and pain is less likely to be felt.
In many cases, Raynaud's disease is limited to these symptoms, but if it progresses, the clinical picture changes. The duration of attacks can reach several hours; the capillaries of the tip of the nose, the edges of the ears, and the edges of the lips are involved in a spastic state. Cyanosis (blueness) of the fingers is accompanied by pain and swelling. The first signs of dystrophy appear, i.e. persistent disorders of tissue nutrition: blisters, peeling, small scars, etc.
The first two stages usually take a total of up to five years and are most often accompanied by an increase in neurological symptoms (headaches, sleep disturbances, etc.). Then necrosis (death) begins, the skin of the fingers turns black, characteristic trophic ulcers appear, when infected (and in the absence of adequate help, for example, in cases of persistent obscurantist self-medication), gangrene can develop.
There are fairly clear criteria for diagnosing Raynaud's disease/syndrome; in addition, the symptoms are quite obvious and specific. However, in most cases, a thorough comprehensive examination is still required - primarily for the purpose of differential diagnosis with other diseases and clarification of the primary/secondary nature of the pathology (i.e., identifying or excluding previously undiagnosed systemic background diseases that could occur, for example, in mild or asymptomatic form and practically does not bother the patient). A hypothermic test is performed, laboratory blood tests are prescribed, and sometimes examination of the capillaries of the nail bed is indicated and advisable.
In some cases, symptoms can be reduced depending on age-related hormonal changes, in others they steadily worsen.
About our clinic Chistye Prudy metro station Medintercom page!
Symptoms
The duration of an attack in Raynaud's disease ranges from a few minutes to several hours. The area of color change is usually clearly limited.
Signs:
- pale, bluish skin;
- numbness of fingers;
- burning, bursting pain;
- soft tissue necrosis, ulcers;
- deformation of the fingers and nail plate.
At first, the attacks are short-lived, but over time they become more frequent, and the damage becomes more obvious.
Stages of the disease
There are three phases of Raynaud's disease:
- Pale skin, numbness, tingling, pain, decreased temperature in the extremities.
- Blueness, pain.
- Swelling and redness, decreased pain.
The third stage is considered the most dangerous, in which ulcers and necrotic areas of the skin may appear.
Amen's test
1) Amen's test to detect occlusion of the branches of the radial artery or ulnar artery distal to the wrist. The patient clenches his fist to force the blood out of the hand. The doctor clamps the ulnar and radial arteries. The patient unclenches his fist, the hand remains pale. The doctor stops compressing the radial artery while continuing to compress the ulnar artery. If the radial artery distal to the site of clamping is patent, the hand quickly turns pink. If the patency of the radial artery is impaired, the hand remains pale. The patency of the distal branches of the ulnar artery is examined in the same way.