Diabetes mellitus is one of the most serious health problems in the world. One of the main complications of diabetes is a blood vessel disease called diabetic angiopathy. Impaired nutrition of the nerve trunks leads to the development of another problem in patients with diabetes - neuropathy.
Diabetic angiopathy
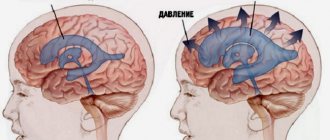
Diabetic angiopathy is a vascular lesion that occurs in people with diabetes. In diabetes, cholesterol and calcium gradually accumulate in the walls of the arteries, which leads to their obstruction and disruption of the blood supply to the tissues.
Diabetic angiopathy is divided into two main types: microangiopathy (damage to small vessels) and macroangiopathy (damage to large main arteries), and there is often a combination of both.
Macroangiopathy develops in the vessels of the heart and lower extremities, being essentially their malignant atherosclerosis.
Microangiopathy most often manifests itself in damage to the arteries of the eyes (retinal damage - diabetic retinopathy) or kidneys (diabetic nephropathy).
Diabetic neuropathy
Diabetic neuropathy is a type of nerve damage that can occur when the vessels in the nerve trunks are affected. Diabetic neuropathy most often develops in the nerves of the legs and feet.
Depending on the affected nerves, symptoms of diabetic neuropathy can range from pain and numbness in the extremities to complete loss of sensation in the feet and hands, with the development of lesions and purulent complications.
Diabetic neuropathy is a very common complication of diabetes. However, it is often possible to prevent diabetic neuropathy or slow its progression through strict blood sugar control and a healthy lifestyle.
Causes of diabetic angiopathy and neuropathy
It is known that diabetes mellitus causes hormonal and metabolic disorders, which cause the deposition of cholesterol plaques and inflammatory changes in the walls of blood vessels, which leads to the development and clinical manifestations of diabetic angiopathy. However, not all diabetics complain of manifestations of angiopathy. This complication of diabetes depends not only on the hormonal background of a particular patient, but also on his genetic characteristics.
Diabetics with high blood pressure, smokers, and alcohol abusers have more pronounced and malignant manifestations of diabetic angiopathy.
Long-term exposure to high blood sugar can damage fine nerve fibers, causing diabetic neuropathy. The main cause of nerve damage in diabetes is considered to be microangiopathy of the vessels supplying the nerves. Their blockade in diabetic angiopathy leads to a deficiency of oxygen and nutrients in the nervous tissue and to the death of nerve fibers.
Causes
Inflammatory disease of peripheral nerves can be triggered by various factors:
- hypothermia;
- infectious diseases - influenza, measles, herpes, brucellosis, etc.;
- injuries accompanied by damage to nerve fibers;
- vascular diseases;
- lack of vitamins in the body;
- intoxication of exogenous and endogenous nature.
Often neuritis develops in the musculoskeletal canals. Their natural narrowness, due to anatomical features, may predispose them to the formation of inflammatory processes.
Another common cause of neuritis is compression of the peripheral nerve by surrounding tissues. This condition can be provoked by sleeping in an uncomfortable position, prolonged maintenance of an unnatural body position, which creates a load on individual organs, or mechanical pressure.
Types of diabetic angiopathy
Diabetic nephropathy develops when the small arteries of the kidneys are damaged and leads to disruption of their function, up to the development of severe renal failure. Diabetic nephropathy is manifested by the appearance of protein in the urine, severe arterial hypertension, and increased levels of creatinine and urea in the blood.
Diabetic retinopathy develops when the retinal arteries are damaged. It is characterized by changes in the vessels of the fundus and hemorrhages in the retina. Can lead to retinal detachment and complete blindness.
Angiopathy of the lower extremities in diabetes mellitus develops through four stages:
- The first stage has no clinical symptoms, however, when examining the vessels, thickening of the arterial walls and their calcification can be detected.
- The second stage is manifested by the appearance of pain when walking over a certain distance (intermittent claudication)
- The third stage is characterized by the appearance of pain in the legs at rest, especially when lying horizontally. If you lower your legs, the pain decreases significantly.
- The fourth stage is manifested by the appearance of trophic ulcers and necrosis on the legs, and diabetic gangrene often develops. This condition is called diabetic foot syndrome.
Diagnostics
The presence of the median nerve is indicated by the following results of functional tests:
- with the palm pressed to the table, the patient cannot make scratching movements with the 2nd finger;
- when the affected hand is clenched into a fist, bending the first three fingers is most difficult;
- the patient is unable to place the little finger and thumb on the same plane.
Additionally, various electrophysiological procedures may be prescribed. In each individual case, the neurologist working with you at the Health Workshop clinic will draw up an individual list of required examinations.
Types of diabetic neuropathy
There are four main types of diabetic neuropathy. Most develop gradually, so this complication may not be noticed until serious problems arise.
Peripheral polyneuropathy
Peripheral neuropathy is the most common form of diabetic neuropathy. First, problems with sensitivity develop in the legs, then signs of neuropathy may appear in the arms. Symptoms of peripheral neuropathy are often worse at night and may include:
- Numbness or decreased ability to feel pain or changes in temperature.
- Tingling or burning sensation.
- Sharp pain or cramps.
- Increased sensitivity to touch - for some people, even the weight of a sheet can be excruciating.
- Muscle weakness.
- Loss of reflexes, especially in the ankle.
- Loss of balance and coordination.
- Serious foot problems such as ulcers, infections, strains and bone and joint pain.
Autonomic neuropathy
The autonomic nervous system controls the heart, bladder, lungs, stomach, intestines, genitals and eyes. Diabetes can affect the nerves in any of these organs, which can cause:
- Problems with urination - urinary retention or incontinence due to damage to the autonomic innervation of the bladder.
- Constipation or uncontrolled bowel movements.
- Slowing of gastric emptying (gastroparesis), leading to nausea, vomiting, bloating and loss of appetite.
- Difficulty swallowing
- Impaired potency in men
- Vaginal dryness and other sexual disorders in women
- Increased or decreased sweating
Diabetic amyotrophy
Diabetic amyotrophy affects the large nerves of the limbs, such as the femoral and sciatic nerves. Another name for this condition is proximal neuropathy, which most often develops in older people with type 2 diabetes.
Symptoms usually occur on one side of the body and include:
- Sudden, severe pain in the hip or buttock
- Thigh muscle atrophy
- Difficulty getting up from a sitting position
Mononeuropathy
Mononeuropathy involves damage to a specific nerve. The nerve may be in the face, torso, or leg. Mononeuropathy is also called focal neuropathy. Most often found in older people.
Although mononeuropathy can cause severe pain, it usually does not cause any long-term problems. Symptoms gradually decrease and disappear on their own after a few weeks or months. Signs and symptoms depend on the specific nerve affected and may include:
- Double vision due to damage to the oculomotor nerve
- Facial paralysis with facial asymmetry
- Pain in the lower leg or foot
- Pain in the lower back or pelvis
- Pain in the anterior thigh
- Pain in the chest or stomach
- Weakness in the hand, with damage to the nerves of the brachial plexus.
Causes of peripheral neuropathy
The most common cause of peripheral neuropathy is diabetes. Other reasons include:
- taking certain medications, including certain types of chemotherapy. For more information, see the Chemotherapy section below;
- lung cancer;
- multiple myeloma;
- alcohol abuse;
- some other forms of cancer (for example, induced neuroleukemia).
If you have any of these possible causes of peripheral neuropathy, tell your doctor or nurse. Tell them what medications you are currently taking, including over-the-counter medications, and what medications you have taken regularly in the past.
Sometimes there is no obvious cause for peripheral neuropathy.
chemotherapy;
Some common types of chemotherapy drugs can also cause peripheral neuropathy. Below we list them and the symptoms that these drugs can cause.
- Bortezomib, carfilzomib May cause numbness, pain, or burning in the legs or arms.
- May cause difficulty in spatial positioning of arms and legs. This is called position sensitivity. This can cause you to slip out of your shoes or slippers if they are not laced or closed to the middle of the top of your foot.
- May cause problems with feeling the shape of an object in your hand or handling small objects.
- May cause problems in sensing the difference between heat and cold.
If you use any of these drugs, you may also have trouble performing activities that require muscle strength and coordination. For example, you may have difficulty moving your foot from the gas pedal to the brake pedal while driving. Some patients also describe sensations of muscle spasms, heaviness, swelling that is not actually there, and weakness in the arms or legs.
Some of these symptoms may improve (weaken) during the first 6 to 18 months after treatment.
to come back to the beginning
Diagnosis of neuropathy and angiopathy
The diagnosis of diabetic neuropathy is based on symptoms, history, and clinical examination. During the exam, your doctor may check your muscle strength and tone, tendon reflexes, and sensitivity to touch, temperature, and vibration.
Additional diagnostic tests:
- Nerve conduction studies. This test checks how well the nerves in the arms and legs conduct electrical signals.
- Electromyography (EMG). Often performed in conjunction with nerve conduction studies, electromyography measures the electrical discharges produced in your muscles.
- Quantitative sensory testing. This non-invasive test is used to evaluate how responsive nerves are to vibration and temperature changes.
- Vegetative testing. The reaction of blood pressure in different body positions and the ability to sweat are assessed.
Symptoms of peripheral neuropathy
Many people with peripheral neuropathy have changes in sensation in their toes, feet, fingers, hands, or face. These sensations may not extend beyond the wrist or ankle.
Symptoms of peripheral neuropathy vary depending on which peripheral nerves are affected. Sometimes only one type of nerve is affected. Most often, more than one type is affected, so you may experience more than one symptom.
- If sensory nerves are affected, you may experience a "pins and needles" or "electric shock" sensation. You may also feel cold, tingling, tingling, or burning sensations in your arms and legs. Some people become very sensitive to touch, while others feel numb.
- If your motor nerves are affected, you may experience muscle weakness, spasms, and twitching. You may also lose balance and coordination. This may make it difficult to walk, drive, or handle small objects (such as a pen or shirt buttons).
- If your autonomic nerves are affected, your heart may beat faster or slower than normal. You may also sweat more or less than usual and notice bowel and bladder problems.
Be sure to discuss your symptoms with your doctor or nurse. They can suggest ways for you to relieve these symptoms.
Symptoms of peripheral neuropathy may come on suddenly or develop slowly. They may come and go or appear to a greater or lesser extent at certain times. Depending on what caused peripheral neuropathy, symptoms may subside over time or last your entire life.
to come back to the beginning
Treatment of diabetic angiopathy
Compensation for diabetes mellitus is the basis of treatment for diabetic angiopathy. It is necessary to reduce blood glucose levels to normal values using glucose-lowering drugs; in severe cases of diabetes, it is necessary to use insulin therapy.
If objective signs of arterial damage (narrowing, calcification) are detected, it is advisable to constantly take angioprotectors (Vessel Due F), antithrombotic drugs (aspirin, Plavix), and vitamins.
Signs of severe angiopathy, with circulatory disorders in organs and limbs, should be the reason for active surgical treatment. In case of damage to the arteries of the leg, heart and kidneys, it is advisable to restore blood circulation using endovascular surgery methods (angioplasty and stenting). This will prevent the development of severe complications such as gangrene, myocardial infarction, and renal failure.
Diabetic angiopathy is a very dangerous disease that can be fatal. When the first symptoms of angiopathy appear, a patient with diabetes should immediately visit an experienced doctor specializing in this problem.
Doctors' forecast
Statistics are not encouraging with cases of 100% recovery from optic nerve neuropathy. Optical pathology is partially eliminated with early diagnosis and timely treatment. Ideally, you can count on no recurrence of the disease in the future. Visual acuity will never correspond to the norm, but a person will still be able to see. The situation is worse with the chronic form of optic neuropathy, in which the progression of the disease is steadily increasing.
Prevention of relapse in the form of neurodegeneration will help smooth out the symptoms of the pathology. The patient needs to undergo ongoing maintenance therapy under the supervision of several specialists.