Doctors call obsessive-compulsive personality disorder a mental health disorder characterized by a high level of anxiety in the patient. Obsessive (obsessive) ideas are constantly repeated, cause disturbing emotions (disgust or anxiety), a person is not able to control them. Many people suffering from obsessive-compulsive disorder realize that the images or thoughts are a product of their mind, they are unreasonable or excessive. However, obsessions are not resolved through reasoning or logical thinking.
The Yusupov Hospital has created comfortable conditions for the treatment of patients suffering from obsessive-compulsive disorder.
What it is?
Obsessive-compulsive disorder is a category of mental disorders that can affect not only adults, but also children. It is characterized by the appearance of:
- Obsessive thoughts and specific behavior in character. Otherwise it is called obsession. They are repeated with regularity, and no one is able to control them and cope with them on their own.
- Actions that are quite tiresome are compulsions. They are compulsive actions and manipulations of behavior or thoughts that are repetitive in nature. They are a kind of response to obsessions, since by performing certain rituals, the patient relieves a high level of anxiety for a short period of time (as if he calms down).
OCD in children
Most often, the disorder manifests itself in children during adolescence. The incidence rate up to 12 years is 1%.
Its causes are gene mutations, infectious diseases, disorders in the metabolism of neurotransmitters, features of the development of the central nervous system, as well as the costs of education, the atmosphere in the family and relationships in society.
Thus, overly strict upbringing, excessive demands on the child, strict moral principles, violence and quarrels in the family, and a religious cult contribute to the development of obsessive-compulsive neurosis.
OCD is mostly manifested by anxiety and fears. For preschoolers, the most common type of OCD is phobias, for children 6–8 years of age – compulsions. And teenagers are most often overcome by obsessions.
Common manifestations of OCD in childhood and adolescence are:
- Thoughts about cleanliness. Children constantly wash their hands and wipe door handles, including in public spaces.
- Fears of harm - getting sick with a dangerous disease, going to hell, hurting someone.
- Counting - chewing food a certain number of times, counting objects. Example: I need to count to 30, and then my grandfather will not die.
- Thoughts about safety. Checking the door, iron, gas, spitting over my shoulder 3 times - then nothing bad will happen.
- Symmetry. Children arrange books, notebooks, and clothes in a certain sequence, by size, and color.
- Thoughts about your appearance. At the same time, teenagers spend too much time in the bathroom or in front of the mirror.
- Children double-check their homework or class assignments many times, afraid of making a mistake. Or they do it very slowly.
- Constant, annoying repetition of certain questions that require answers: Will I be late? Will the bus definitely come? Could we have a tsunami?
Children are frightened by their obsessive thoughts and actions, so they try to hide them from others. They become withdrawn, nervous, anxiety increases, and school performance decreases.
Origin
The intense pace of life that has developed in the modern world creates stressful situations for a person every day. Some are able to overcome them quite successfully, others fall into their trap, from which it is almost impossible to get out on your own. As a result, such individuals develop stress changes or depression and a depressed mood.
But this is the main reason, the development of which can be pushed by accompanying external and internal factors, such as:
- Hereditary predisposition. Numerous medical scientific studies have confirmed the fact that OCD is inherited. This means that people with a family history of people susceptible to this syndrome are much more likely to develop this pathology. But only nature is transmitted through genes, while a group of symptoms can be completely different. For example, a mother has a pathological tendency to wash her hands, fearing to remain dirty all the time. Whereas the daughter may demonstrate a fear of improper communication with people and the consequences of this.
- Features of the structure of the nervous system. This biological parameter also plays a significant role. If a patient's brain lacks neurotransmitters that should have been developed before the age of 23, it will lack components such as dopamine and serotonin. And they play a decisive role in creating a feeling of satisfaction. Thus, the individual at the biological level is deprived of the opportunity to receive satisfaction from life - as a result of which a stable stressful state arises. It would seem that even from minor failures, which under normal conditions are perceived adequately, persistent negativism is formed in such individuals.
Certain living conditions may also contribute to the formation of the disease. These include:
- anxiety due to separation anxiety experienced in childhood;
- inclinations to submit;
- an overwhelming sense of perfectionism, pushing for constant improvement and achieving goals at any cost;
- a sense of dedication and commitment while performing work activities;
- high levels of individual morality;
- punishments in childhood that sharply limited freedom of expression;
- ardent resistance to any changes that arise along the path of life;
- a negative attitude towards all risks, no matter what they are associated with;
- an increased level of sensitivity, which forces the patient to react emotionally to any actions that occur;
- development of ambivalence.
Also, psychiatrists and psychologists agree that studying can accompany the development of the syndrome. But it happens when a person experiences in childhood:
- restrictions during training – a sense of perfectionism and increased responsibility is achieved and formed;
- when a person suffering from this type of disease acted as a teacher or educator;
- restrictive and strict religious upbringing, and education, which forces even thoughts about negativism or negative actions to be equated with committing such actions - as a result of which the person and his nervous system become constantly tense, the level of responsibility increases, leading to stress;
- excessive moral education, with the formation of sharp boundaries that are strictly forbidden to cross;
- the formation of a certain type of belief;
- increasing the level of responsibility - the individual takes on too many factors for which he is responsible, although in fact he does not have the ability to cope with this;
- attempts to completely and absolutely control the flow of one’s own thoughts;
- attaching too much importance to a wide variety of thoughts, actions and events;
- inability to tolerate uncertain situations in life.
Considering all of the above, it is clear that one of the most basic reasons causing obsessive-compulsive disorder is specific behavioral patterns and character with increased anxiety, responsibility and morality in combination with genetic predisposition and unfavorable living conditions. Although, sometimes being overly comfortable can also push one towards pathology.
Mild and severe forms of OCD
Almost all of us have had “magical thinking” to varying degrees. It is a normal stage in the development of the psyche of children, partially remaining with us in adulthood. A black cat crossing the road, or relatives spilling salt on the table, force us to perform certain rituals, after which we simply forget about what happened.
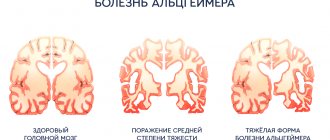
With progressive OCD, these actions help only briefly relieve anxiety and tension from obsessive thoughts. Unfortunately, severe forms of this disorder can lead to disability and disability due to the development of an imbalance of serotonin, an important neurotransmitter in the brain.
Symptoms
OCD is a mental disorder that can only be diagnosed by a medical specialist. Only a psychotherapist or psychiatrist can give a final conclusion. To accomplish this, a variety of methods are used.
There are certain symptoms of OCD that indicate the presence of the disease. Those suffering from the disorder can detect them on their own or with the help of family and friends:
- Many begin to bargain with their own conscience and subconscious. Convince yourself of the presence of symptoms of a non-existent disease or re-check the closure of the tap, rearrange things, check the door, then the problem will disappear. In fact, there is a movement in a circle. Obsessive rituals only strengthen specific sensations in the brain, forming an image of a dangerous picture that really takes place.
- The need to perform repetitive manipulations and actions increases many times over. But there is a certain “but” here. If a healthy person has the habit of washing their hands several times for no apparent reason, this does not mean at all that they have OCD. Perhaps he is simply afraid of getting infected and getting sick. Then you need to be aware of whether there is a willingness to give up repetitions for a certain amount of remuneration. If so, then it's just a bad habit. Otherwise, this is really a deviation that requires psychological help or psychotherapy.
- It is difficult to convince an individual that there is no threat. They are attached to their fears, so no amount of belief helps them become more confident. They are ready to counter any admonitions with the phrases “yes, but...”. The result is anxieties that continue to torment and torment the soul, which only intensify over time even when the fears are not realized.
- A clear awareness of when it started and how long it lasts. Control is not weakening at all.
- An overwhelming feeling of anxiety. But it must be borne in mind that it has an established basis. True, in a healthy situation a person is able to overcome these factors. He knows how to control and suppress them. Whereas a person suffering from OCD cannot do this on their own.
Despite the symptoms and signs, there is absolutely no need to despair. These deviations can be corrected. This is done through specialists who need to be contacted on time and in specialized clinics. They can be found on the Internet, and on the site you can know all the necessary situations.
It is worth remembering that the sooner help is accepted, the faster and more effectively it will be possible to get rid of the problem.
The symptoms may be alarming, but the final diagnosis is made exclusively by a specialist who can determine obsessive-compulsive disorder based on the symptoms present and prescribe adequate treatment.
It is important to understand that there are differences between normal and pathological thoughts. They do not lie in the content itself, but in the patient’s attitude towards them.
According to recent studies, in the vast majority of cases, that is, 90% of the adult population, there are thoughts that are of a fixated nature. They concentrate too much attention, but do not suffer from cognitive behavioral disorders.
What happens during the pathological process? What dependencies are formed and to what extent, and how do they affect health? The significant difference is that a trigger (trigger - irritant or so-called trigger) gives rise to the appearance of obsessions in the form of involuntary thoughts. The process is still poorly controlled by the individual himself, which is why anxiety manifests itself in him. But the body, trying to avoid self-destruction, causes compulsive manipulation. They consist of repeating the same rituals.
An interesting fact is that the fears that the patient experiences do not come true only for the reason that the individual triggers compulsive actions. And the absence of a negative manifestation does not mean that fears are unfounded or that the person is innocent.
Compulsion has a short spectrum of manifestation - it is designed to smooth out fears or reduce the level of discomfort. If the disease is not treated, then in the long term, compulsive behavior maintains fears and a vicious circle arises, which can lead to the persistent formation of the disease.
Analogies of OCD can be drawn with panic attacks and conditions, as well as agoraphobia.
Forms of the disease
Obsessive-compulsive neurosis manifests itself in 2 main forms – obsessions and compulsions.
Obsessions are annoying thoughts that regularly visit a person. However, he cannot control them or get them out of his head. In one case, they are periodic and do not overly absorb a person’s consciousness, in the other, they terrorize him almost all the time. At the same time, the person tries hard to overcome them, to get them out of his head, but nothing comes of it.
For example, a girl is overcome by the idea that she might be seduced by a woman and become a lesbian. Because of this, she tries not to let women touch her.
Such obsessions manifest themselves in several categories:
- doubts. In this case, the patient constantly questions his actions and seeks confirmation of their correctness in everything. At work, while fulfilling his duties, he asks to be rechecked. When leaving the house, he returns several times to make sure that the gas is closed;
- fear. A person is afraid that he will not be able to perform any action correctly or will do something dangerous for him. This includes fear of public speaking;
- attractions. A person's desire to commit an obscene or dangerous act. For example, when a passionately loving mother has a pathological desire to kill her child. Or a respectable, moral girl has a super-urge to commit depraved acts. The peculiarity of such drives is that they are never realized;
- memories. Images of a past event, lyrics of a song, phrase, etc. constantly pop up in a person’s mind;
- thoughts. Implausible thoughts about an important event that has happened. This often happens to parents who have lost a child. Disbelief that he was dead or the belief that he was buried alive may prompt them to exhume the body.
Obsessions also include meaningless philosophizing. This is a process of fruitless thinking, without specific goals and results. For example, while walking down the street, a person may reason about whether a red car will pass by. If so, what shade will it be: light or dark? Where she is going, will she turn or go straight. How many people will be in the car, what brand will it be, etc.
Such philosophizing differs from reasoning in the critical attitude of the patient himself to it.
Some experts also include phobias in this group - a pronounced, hypertrophied fear of something. The most common:
- cancerophobia – fear of getting cancer;
- Cardiophobia – heart disease;
- algophobia – fear of pain;
- thanatophobia – fear of death;
- nyctophobia – fear of the dark;
- phobophobia – fear of fear;
- Panophobia is the fear of everything in the world.
Obsessions do not affect the patient’s logical thinking. In addition, some try to fight such obsessive thoughts. In case of active opposition, a person can take actions in defiance of obsessive thoughts. If he has doubts about a locked door and is tempted to go back and double-check it, he deliberately does not return and follows in the designated direction.
In case of passive opposition, a person tries to switch to other thoughts or actions.
Compulsions are obsessive actions that appear regardless of a person’s will. At the same time, he is accompanied by an irrepressible desire to perform them repeatedly in such a way that they acquire the character of a ritual. If the patient tries to refuse to commit them, then he develops anxiety and a feeling of fear. They will accompany him until the person completes the ritual.
The girl is forced to press the switch 3 times. At the same time, she is sure that if she stops doing this, something terrible will happen.
Examples of compulsions also include pathological overeating, excessive exercise - several hours several times a day, and by fairly slim people whose physical form does not require it. They play sports so much because they simply have an irresistible need for it. Having completed the ritual, they calm down, but the next day the impulse to train returns.
Workaholism, the need to constantly do some kind of work and not sit idle, is also classified as compulsions.
Obsessive actions can visit a person in one instance, or can be combined in several forms. Thus, there is a well-known story of one girl whose obsessive-compulsive disorder first appeared at the age of 10. It all started with a craving for symmetry, to achieve which she cut her eyelashes repeatedly. Then came the need to count steps, wash hands many times, and avoid cracks in the road. Gradually, self-traumatic rituals were added: cutting, burning, etc.
But most often, compulsions and obsessions occur simultaneously, forming obsessive-compulsive disorder.
It all starts with the emergence of an obsessive, frightening thought. For example, about the accumulation of pathogenic bacteria on the hands, which can cause a terrible, fatal illness. A person is looking for a way out of the situation, how to avoid this. He begins to wash his hands, and not like a normal person: before eating, when he comes home from the street, and several more times between “normal” washings. Several dozen times. But it’s not just the banal thing of washing your hands with soap.
Before performing the ritual, a person decides how many times he should soap his hands. 2 times 3 sets, but not 3 times. 3 is the Holy Trinity, there is no need to involve it in such a banal matter. Then it’s better to do 5 times 5 repetitions. He lathers his hands 5 times, rinses and repeats the action 4 more times. This brings relief for a while, but soon the annoying thought arises again. And the person begins to wash his hands again a certain number of times. At the same time, he understands the absurdity of the situation, but is unable to refuse it.
Treatment Methods for Obsessive Compulsive Disorder
The best results are shown by a combination of medication, in combination with psychological behavioral therapy, which allows you to practice normal behavior skills. So, if you use EPR - exposure with the prevention of reactions, you can achieve not just temporary relief, but a radical improvement in the quality of life and getting rid of an undesirable manifestation.
Considering all the features of OCD treatment, it is worth noting the following specific effects from each type and technique:
- EPR technique. Its essence lies in the fact that an adult or teenager is specifically immersed in an existing problem. In this way, his anxiety is deliberately increased, and subsequently techniques are used that help make sure that such obsessive states are still wrong. A psychologist or psychiatrist who is involved in treatment must necessarily monitor the absence of compulsion rituals. Naturally, they do not prevent this physically, but do it on a psychological level. This is the only way to cope with discomfort and anxiety. This technique is most often used in combination with cognitive therapy and behavioral analysis. This helps to further reduce the significance of the obsession, reduce the level of anxiety and eliminate excessive responsibility.
- It can also be treated with medications. In this case, the doctor prescribes antidepressants, but it is necessary to take into account the fact that the effectiveness of such drug therapy is only a maximum of 40%.
Therefore, most experts recommend treating obsessive-compulsive disorder using combined techniques, regardless of how old the person actually suffers from the symptoms. But taking into account the possible use of one or another group of medications at a certain age stage.
Causes of OCD
Until now, scientists have not fully figured out why this disorder occurs. However, there are a large number of theories that interpret its development in their own way.
Most experts are inclined to believe that obsessive-compulsive disorder is caused by a disruption in the production of neurotransmitters, in particular serotonin. Its reuptake increases and, as a result, the remaining amount of the transmitter is not enough to transmit the nerve impulse to another nerve cell.
PANDAS theory suggests that staph infection may play a role in the development of OCD. This happens when the antibodies produced against staphylococcus destroy not only microbes, but also nerve cells.
In addition to staph infections, obsessive-compulsive disorder occurs due to other immune responses, chronic diseases, and TBI.
For example, a 17-year-old boy grew up like an ordinary teenager. As is customary with most young people, he was fond of sports, or rather football. During this time, he suffered a concussion six times. The last time triggered chronic OCD in a guy. Now he is forced to open and close the car door 5-6 times in a row before he gets in or out of it, goes down and up the stairs several times, walks past mirrors, and opens the door indoors. The boy's mother claims that the disorder had a noticeable effect on his condition. He became nervous, aggressive, impatient and hot-tempered. The atmosphere in their family deteriorated significantly. The young man's relationship with his other brothers deteriorated.
Heredity also plays an important role in the occurrence of OCD. It has been established that for individuals whose parents suffered from mental illnesses, the risk of developing obsessive-compulsive disorder neurosis increases. Relatives’ addiction to alcohol, which provokes alcoholic psychosis, is also important.
For OCD, there is such a thing as comorbidity, that is, when one patient has a combination of several interrelated diseases. Likewise, OCD can appear against the background of depression, bipolar, panic disorders, etc.
Being a mental illness, a special role in its manifestation is given to the upbringing and formation of a child’s character with anancastic traits. Such a personality is characterized by an excessive desire for perfection, she is overcome by constant doubts and delving into details. She is stubborn and always stands her ground.
Mental trauma or severe shock can trigger the development of OCD.
Development of the disease and prognosis if not treated
When the essence of this condition is considered, it is classified as one that is at the intersection of obsession, phobias and mania. All this makes it possible to conclude that this deviation is a very serious pathology, which cannot be eliminated on its own. In order to return to a normal course of life, the participation of a qualified doctor, psychotherapist or psychologist is necessary. But more often, help will be needed from both of them.
In support of these words, we can cite the facts that in some countries of the world people suffering from obsessive-compulsive disorder are classified as disabled and unable to perform various manipulations that benefit society as a whole, and therefore are assigned health benefits. That is, in fact, they are equated to the group of disabled people, however, no one limits their ability to get out of this condition, since the disease can become reversible - and this is one of the important factors that must be taken into account. That is, no one restricts the right to lead a normal lifestyle and does not isolate him from the community.
You can get rid of this pathology, and it is advisable to do this at the earliest possible stages. Then the symptoms go away quite quickly, in contrast to those situations when the condition is excessively triggered.
Complications include:
- Obsessive-compulsive disorder is a rather complex pathology of personal development and formation. It is formed under the pressure of neuroses. Therefore, if the problem is ignored, negative aspects and sensations in neurology increase. Deterioration of cognitive functions, neurotic reactions, restless sleep, emotional instability, etc. may be observed.
- Pathological conditions also include persistent fears that change behavior and perceptions of existing reality. These are more complex stages compared to the first group of symptoms.
- Inability to contact others.
- Depression can lead to suicide attempts.
Analyzing the general condition of the vast majority of patients who did not receive medical care on time, we have to testify that they cease to be full members of society.
They cannot normally perform functional duties at work, are unable to contact their family and maintain full-fledged family relationships with relatives without causing psychological damage to them. That is why, in order to eliminate all unpleasant symptoms, reduce the level of doubt, and also increase social adaptation, it is imperative to seek qualified help and not try to get rid of the problem on your own.
If we talk about the time frame during which the disease most often occurs, then there is no pattern. Neurosis with possible pathological deviations occurs in both young children and the elderly. Thus, according to some statistical parameters, among children the syndrome can occur, depending on the country and living conditions, 1 time per 200-500 population. Whereas in adults it is standard everywhere and is approximately 1 in 300.
Moreover, the clinical picture in the overwhelming majority appears the same. Most often it is expressed in the form of fear. So, it is most actively formed when there is contact with other people or objects. Fear of getting your hands dirty from dirty objects or from shaking hands is the most common fear of OCD diagnosis. In this case, the patient experiences a regular need to wash his hands. If he cannot do this, then it ends up being stressful for him. At first, this may be considered simply excessive cleanliness. But, later, during development, it acquires a pathological character, demonstrating itself more and more powerfully and alarmingly. At the same time, a teenager or adult experiences suppressed emotions if he is unable to perform the ritual.
The opinions of others can also become obsessive. A person suffering from obsessive-compulsive disorder feels that people are behaving in unusual ways. They can spend an entire day wondering if they were given their hand a few seconds too late.
These periods may initially occur occasionally, but, in the absence of main treatment methods, they will become more frequent and worse, driving the individual into an increasingly difficult existence. His positive emotions begin to be suppressed, as a result of which the physical component begins to suffer.
What needs to be done after finishing treatment?
The duration of treatment, including medication, is determined individually. Once appropriate treatment has been completed, it may be indicated to repeat the skills and exercises learned during CBT.
As with other mental disorders, it may be helpful to take care of general mental hygiene and health—concern for your overall development, developing stress management and problem-solving skills, developing positive interpersonal relationships, avoiding the use of psychoactive substances (drugs, alcohol), proper nutrition, physical activity. An important issue is also the acquisition of the ability to recognize signs of relapse of the disorder and prompt pharmacological and/or psychotherapeutic intervention when it occurs.
A detailed algorithm of action is determined by the doctor, selecting it for each patient.
Diagnosis of pathology
The only way to correctly diagnose is to contact a doctor who is a specialist in the relevant field. At the same time, doctors use a variety of techniques for obsessive-compulsive disorder, for example, differential diagnosis and various testing methods.
The simplest way for specialists to diagnose is to use the Yale-Brown test. Such tactics help not only to establish the presence of a deviation, but to effectively determine the severity of the course.
How is the disorder treated?
Today, there are several treatment options that have proven themselves, depending on the degree and form of development of the disorder.
The most effective way to combat the disease is cognitive behavioral psychotherapy. It allows you to teach the patient to manage their symptoms, anxiety levels, and understand the connection between thoughts and emotions. Psychoanalytic psychotherapy also leads to successful results. With its help, the main causes that led to the development of the disorder are identified and “worked through.”
Severe forms require contact with a psychiatrist and medication support, after which treatment must be continued as part of psychotherapy.
Survey
If obsessive-compulsive neurosis is suspected, the doctor conducts an examination, survey, and psychological testing. If a psychosomatic disease is detected, the patient is referred for consultation to specialized specialists (hepatologist, gastroenterologist, otolaryngologist, cardiologist, etc.).
The presence of a disorder is indicated by regularly occurring obsessions lasting at least one hour a day. They change a person’s life, make it incomplete, interfere with their ability to perform work duties and study.
Among the diagnostic criteria of the disease:
- increased sweating;
- hand tremors;
- nervous tic;
- involuntary twitching of facial muscles;
- increased tendon reflexes.
If there is a suspicion of organic brain pathology, an MRI or CT scan is performed.