ENMG.INFO
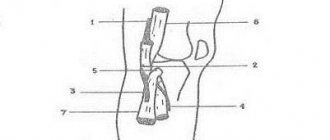
The ulnar nerve (n. ulnaris) originates from segments C8 and Th1 . In the brachial plexus it moves first as part of the lower trunk, and then as an internal bundle. At the level of the lower third of the shoulder, the ulnar nerve departs from the median nerve somewhat posteriorly, enters the medial head of the triceps brachii muscle (m. triceps brachii, caput mediale), then lies in the cubital canal (canalis cubitalis). Next, the nerve follows into the groove between the flexor carpi ulnaris (m. flexor carpi ulnaris) and the deep flexor of the fingers (m. flexor digitorum profundus). At the level of the upper third of the forearm, the ulnar nerve innervates the flexor carpi ulnaris, as well as the ulnar part of the deep flexor digitorum profundus (m. flexor digitorum profundus, pars ulnaris). In the lower third of the forearm, the posterior cutaneous branch (r. cutaneus dorsalis) departs from the nerve, which lies under the flexor carpi ulnaris (m. flexor carpi ulnaris) and exits onto the dorsum of the hand. In this place, the branch provides sensory innervation to the dorsal medial part of the hand, the dorsal surface of the fourth and fifth fingers, as well as the medial part of the dorsal surface of the third finger.
At the level of the wrist, the ulnar nerve passes through Guyon’s canal, then divides into two branches: superficial (r. superficialis) and deep (r. profundus). The superficial branch gives sensitive innervation to the skin of the eminence of the little finger, digital branches to the palmar surface of the fifth finger and the medial surface of the fourth fingers. The deep branch innervates the Hypothenar muscles (m. abductor digiti minimi, m. flexor digiti minimi brevis, m. opponens digiti minimi), mm. lumbricales III et IV, mm. interossei dorsales et palmares, as well as partially some Thenar muscles (m. abductor pollicis brevis, m. flexor pollicis brevis, caput profundum).
Muscle innervation:
- Upper and middle thirds of the forearm: Flexor carpi ulnaris (m. flexor carpi ulnaris)
- Ulnar part of the deep flexor digitorum (m. flexor digitorum profundus pars ulnaris)
- Abductor digiti minimi muscle
Sensory innervation:
- Palmar surface of the wrist: Palmar cutaneous branch of the ulnar nerve (r. cutaneus palmaris n. ulnaris) - skin of the inner part of the hand
- Connecting palmar digital nerves (nn. digitales palmares communis) – skin of the palm at the level of the IV and V fingers
- Posterior cutaneous branch of the ulnar nerve (r. cutaneus dorsalis n. ulnaris) - skin of the palm at the level of the IV and V fingers, skin of the distal phalanges of the V finger, proximal phalanges, as well as the inner surface of the distal phalanges of the IV finger, as well as innervation of the skin of the inner surface of the proximal phalanges III finger
- Atlas of Human Anatomy (1996) (Sinelnikov R.D., Sinelnikov Y.R.)
- Atlas of Human Anatomy (2003) (F. Netter)
- Atlas of Electromyography (2010) (S.G. Nikolaev)
- Human Anatomy (1985) (Prives M.G., Lysenkov N.K., Bushkovich V.I.)
- Laboratory Reference for Clinical Neurophysiology (1992) (Jay A. Liveson, Dong M. Ma)
Author: Tikhonov A.V.
Copyright protected by Digiprove
N. ulnaris (ulnar nerve)
July 14, 2009
The nerve is mixed, made up of fibers CVIII - DI roots, which then pass through first the primary lower, then the secondary internal bundle of the plexus.
When the roots CVIII - DI of the primary lower and secondary internal bundle of the plexus are affected, the nerve function suffers equally in combination with damage to the cutaneous internal nerves of the shoulder and forearm (nn. cutanei brachii and antibrachii mediales) and partial dysfunction of n. mediani, its lower leg (weakening of the flexors of the fingers, thenaris muscles), which creates a clinical picture of Dejerine-Klumpke paralysis.
The motor function of the nerve mainly consists of palmar flexion of the hand (m. flexor carpi ulnaris), flexion of the V, IV and partly III fingers (mm. lumbricales, flexor digitorum profundus, interossei, flexor digiti V), adduction of the fingers, their spread (mm. interossei) and adduction of the thumb (m. adductor pollicis), in addition, in extension of the middle and terminal phalanges of the fingers (mm. lumbricales, interossei).
With regard to the innervation of movements of the II - V fingers, the function of the ulnar nerve is conjugate with the function of the median: the first has a predominant relation to the function of V and IV, the median - II and III fingers. Sensitive fibers innervate the skin of the ulnar edge of the hand, V and partially IV, less often III fingers.
Complete damage to the ulnar nerve causes weakening of the palmar flexion of the hand (flexion is maintained partially due to the m. flexor carpi radialis and m. palmaris from the n. medianus), lack of flexion of the IV and V, and partly of the III fingers, the impossibility of bringing and spreading the fingers, especially the V and IV, inability to adduct the thumb.
Superficial sensitivity is usually impaired in the skin of the fifth and ulnar half of the fourth finger and the corresponding ulnar part of the hand. The joint-muscular feeling is upset in the little finger. Pain with damage to the ulnar nerve is not uncommon, usually radiating to the little finger. Possible cyanosis, sweating disorders and a decrease in skin temperature in an area approximately coinciding with the area of sensory disorders. Atrophy of the hand muscles with damage to n. ulnaris protrudes clearly, the depression of the interosseous spaces, especially I, is noticeable, as well as a sharp flattening of the hypothenaris.
As a result of the defeat of mm. interossei and lumbricales, the hand takes the form of a “clawed, bird’s paw”: with hyperextension of the main phalanges, bending of the middle and terminal phalanges is observed, due to which the fingers take a claw-like position. This is especially pronounced in relation to the V and IV fingers. At the same time, the fingers are slightly separated, especially the IV and mainly V fingers. Its first branches n. ulnaris spreads only to the forearms, which is why its lesion along the entire length to the elbow joint and the upper part of the forearm gives the same clinical picture.
The lesion in the area of the middle and lower thirds of the forearm leaves the innervation of m. flexor carpi ulnaris and so on flexor digitorum profundus, due to which palmar flexion of the hand and flexion of the terminal phalanges of the V and IV fingers do not suffer. But the degree of “clawedness” of the hand increases.
To determine movement disorders that occur when the ulnar nerve is damaged, there are the following basic tests: I. When clenching the hand into a fist, fingers V, IV, and partly III are not bent enough.
II. Bending the terminal phalanx of the fifth finger (or “scratching” the little finger on the table with the palm tightly fitting to it) is impossible.
III. It is impossible to adduct the fingers, especially V and IV.
IV. Thumb test: the patient stretches a strip of paper, grasping it with both hands between the bent index finger and straightened thumb, with damage to the ulnar nerve and, consequently, paralysis of the m. adductoris pollicis, adduction of the thumb is impossible, and the strip of paper is not held by the straightened thumb.
In an effort to hold the paper, the patient bends the terminal phalanx of the thumb with the help of m. flexoris pollicis, innervated by the median nerve.
“Topical diagnosis of diseases of the nervous system”, A.V.Triumfov
Read further:
Damage to roots and primary trunks
Damage to the entire brachial plexus causes flaccid atrophic paralysis and anesthesia of the upper limb with loss of the extension-ulnar, flexion-ulnar and carporadial reflexes. With high lesions of the plexus, damage to the scapular muscles and Horner's sign are associated. Damage to the CV-CVI roots or the upper primary bundle of the plexus (Erb-Duchenne palsy) leads to loss of function of the axillary (m. deltoideus), musculocutaneous (mm. biceps, brachialis) and only...
Damage to roots and primary trunks (primary plexus bundles)
The primary plexus bundles are further divided into anterior and posterior branches. From the anterior branches of the upper and middle bundles (CV, CVI, СVII) the secondary external bundle (fasciculus lateralis) is formed. From the anterior branches of the lower bundle (CVIII-DII) the secondary internal bundle (fasciculus medialis) is formed. Finally, from all the posterior branches of the primary bundles (CV, CVI, СVII, СVIII, DI, DII) the secondary posterior…
Nerves arising from the brachial plexus
N. axillagis (axillary nerve) Mixed nerve, made up of fibers of the CV, CVI and CVII roots, passing first as part of the primary superior, then the secondary posterior bundle of the plexus. When the CV-CVI roots or the primary superior bundle of the plexus (in the supraclavicular fossa) are damaged, as is observed with Erb's palsy, the nerve suffers in combination with n. musculo-cutaneus. If the secondary…
N. radialis (radial nerve)
The mixed nerve arises mainly from fibers of the CVII (partly also CV, CVI, CVIII and DI) roots, passing first as part of the primary middle plexus, then the secondary posterior bundle of the plexus. When the CVII root or primary middle fascicle is damaged, the main function of the nerve (except for the m. brachio-radialis and m. supinator) is lost in combination with partial damage to the n. mediani, its upper leg...
N. medianus (median nerve)
The mixed nerve is formed from fibers of the CV, CVI, CVII, CVIII and DI roots, passing through mainly the middle and lower primary bundles of the plexus. Subsequently, the fibers of the median nerve pass through the external and internal secondary bundles. The upper leg of the n. extending from the external bundle. mediani and from the internal bundle its lower leg merge, forming a loop of the median nerve….
Discussion
The literature contains information about a significant variety of anatomical variations of the median nerve at the level of the forearm and wrist joint, which can be divided into three groups.
The first two include different options for the origin of the recurrent motor branch in the area of the proximal and distal parts of the carpal canal, the third - a high division of the median nerve at the border of the upper and middle third of the forearm, which occurs in 1.6-2.5% of cases [5, 6 ]. A variant of the high bifurcation of the median nerve may be combined with an accessory median artery or an accessory belly of the lumbrical muscle within the carpal tunnel [5]. Significant variability in the structure of the median nerve is more characteristic of its motor branch. In most cases, it arises from the common trunk distal to the carpal ligament. However, in 23% of cases, the motor branch arises from the main trunk of the median nerve proximal to the distal edge of the carpal ligament [7]. The structure of the common palmar digital nerves is more constant. The median nerve most often divides into the common palmar digital nerves 2–3 cm distal to the edge of the carpal ligament. At this level, bundles branch off separately to the radial surface of the second finger, and the other two branches diverge at the level of the distal palmar fold, forming their own palmar digital nerves of the second and third fingers and half of the fourth finger. Sensitive cutaneous branches of the first finger arise from the median nerve at the base of the eminence of the thumb. Atypical arrangement of nerves on the fingers is extremely rare [8].
P. Amadio [1], in an analysis of 256 operations for carpal tunnel syndrome, found high division of the median nerve into branches only in 8 (3.1%) cases. In 2 out of 8 cases, after separation, the nerve branches reunited again, thus forming a loop. S. Lindley, J. Kleinert [2] in the treatment of 526 patients with carpal tunnel syndrome during open ligamentotomy in 30 (5.7%) cases encountered various anomalies of the muscles, tendons, median and ulnar nerves. Only in 2 (0.4%) cases was it a high bifurcation of the median nerve. In 1 patient, the nerve divided into radial and ulnar parts at the level of the proximal carpal ligament, and in one patient, at the level of the lower third of the forearm.
The latter variant of the structure of the median nerve was observed in our case. Judging by the zone of anesthesia on the patient’s hand (III, IV fingers), it can be assumed that the damaged “second” trunk of the median nerve is n .
digitalis palmaris communis
, innervating the surfaces of the third and fourth fingers facing each other, which separated from the main trunk not at the level of the hand, as usual, but at the level of the forearm. Damage to the ulnar nerve in our case was only within the epineurium. Therefore, sensitivity on the fifth finger and on the radial side of the fourth finger was restored quite quickly. Injury to the median nerve bundles required more time to restore sensitivity.
Thus, a very rare variant of the structure of the median nerve is its high bifurcation. A surgeon may encounter such an atypical division of the median nerve when performing surgical interventions at the level of the forearm.
Brachial plexus injuries
Damage to individual peripheral nerves and nerve plexuses.
In pediatric practice, lesions of the brachial plexus nerves are usually a consequence of pathological childbirth.
Plexus brachialis (brachial plexus)
The brachial plexus is composed of fibers of the anterior branches of the 5th, 6th, 7th, 8th cervical, 1st, 2nd thoracic spinal nerves. The upper trunk (truncus superior) of the brachial plexus is formed from the C5 and C6 spinal nerves, the middle trunk (fruncus medius) is a continuation of the C7 spinal nerve, and the lower trunk (truncus inferior) is formed from the fusion of the C8 and TI-T2 spinal nerves. The listed trunks of the brachial plexus are located in the supraclavicular fossa.
Damage to the entire brachial plexus causes flaccid atrophic paralysis and anesthesia of the upper limb with loss of the extensor-elbow, flexion-elbow and carporadial reflexes. With high lesions of the plexus, damage to the scapular muscles and the Claude Bernard-Horner symptom are added.
Damage to the C5-C6 spinal nerves or the upper trunk of the brachial plexus (Duchenne-Erb palsy) leads to loss of function of the axillary (m. deltoideus), musculocutaneous (mm. biceps, brachialis) and only partially radial (mm. brachioradialis, supinator) nerves . With radicular or very high lesions of the upper trunk, loss of function and scapular muscles (mm. supraspinatus, infmspinatus, subscapularis, serratus anterior) is associated. The ulnar-flexion reflexes are extinguished and the carporadial reflexes may be weakened.
Thus, upper paralysis is characterized by damage to the proximal part of the upper limb while the function of the hand and fingers is preserved. In this case, the distribution of the anesthetic zone occurs along the radicular (C5-C6) type on the outer surface of the shoulder and forearm.
Damage to the C8-T2 spinal nerves or the primary lower trunk of the brachial plexus (Dejerine-Klumpke palsy) causes complete loss of function of the ulnar, internal cutaneous nerves of the shoulder and forearm and partial damage to the median nerve and its lower leg.
The result is distal paralysis with predominant damage and atrophy of the small muscles of the flexors of the fingers and hand, the so-called lower plexus palsy. With a high lesion before discharge rr. communicantes (sympathetic fibers going to the eye), Horner's symptom is added. Sensitivity is impaired in a radicular (C8-T2) manner on the inner surface of the hand, forearm and shoulder.
Damage to the C7 spinal nerve or middle trunk plexus causes significant loss of function of the radial nerve and partially the median nerve.
The trunks of the brachial plexus are further divided into anterior and posterior branches. The anterior bundle (fasciculus lalemlis) is formed from the anterior branches of the upper and middle trunks (C5, C6, C7). From the anterior branches of the lower trunk (C8, T2) the internal bundle (fasciculus medialis) is formed. Finally, from all the posterior branches of the primary trunks (C5, C6, C7, C8, Tl, T2) the posterior bundle (fasciculus posterior) is formed. The names of the beams are determined by their location relative to a. axillaris.
The bundles of the brachial plexus are located in the subclavian fossa; further they form the actual nerves of the upper limb: external bundle - n. musculocutaneus and the upper leg of n. mediani; posterior bundle - n. axillaris et n. radialis and internal beam - n. ulnaris, lower leg n. mediani, nn. cutanei brachii et antebrachii medialis.
Damage to the external bundle of the brachial plexus causes complete disruption of the function of n. musculocutanei, partial - n. mediani (fibers of its upper leg, in particular m. pronator teres), and limited - n. radialis (mm. brachioradialis, supinator).
Thus, the similarity of the clinical picture of a lesion of the upper trunk of the brachial plexus and a lesion of the external bundle of the brachial plexus lies in the loss of the function of the musculocutaneous nerve in both cases and the limited loss of the function of the radial nerve.
The difference is that when the upper trunk of the brachial plexus is damaged, this combination also includes loss of function n. axillaris, which does not suffer when the external bundle of the brachial plexus is damaged, but in the latter case there is partial damage to n. mediani.
Lesions of the internal bundle of the brachial plexus and lesions of the lower trunk of the brachial plexus give a similar clinical picture, i.e., a combination of lesions n. ulnaris, nn. cutanei brachii et antebrachii mediales and partial lesions i. mediani (its lower leg). Horner's symptom in this case, as with more distal lesions, is not observed.
Damage to the posterior bundle of the brachial plexus is characterized by a combination of lesions n. axillaris et n. radialis (except for preserved mm. brachioradialis, supinator). The similarity with the clinical picture of damage to the middle trunk of the brachial plexus is the same loss of function n. radialis. The difference is that when the middle trunk is damaged, the function n. axillaris is preserved, but instead the function of n. mediani, its upper leg.
Thus, the fibers of the lower trunk of the brachial plexus become part of the internal bundle, which causes the similarity of the clinical picture when they are affected. N. radialis suffers in its main function both when the middle trunk and the posterior bundle are damaged, but in the first case (middle trunk) - in combination with partial damage to n. mediani, and in the second (posterior bundle) - with lesion n. axillaris.
Function n. axillaris falls out both when the upper trunk and the posterior bundle are affected due to the corresponding transition of its fibers.
Finally, and. musculocutaneus suffers equally when the upper trunk and the external bundle are affected, but in the first case (upper trunk) - in combination with, n. axillaris, and in the second (lower fascicle) with partial damage to n.mediani.
Nerves arising from the brachial plexus.
- axillaris (axillary nerve ). The mixed nerve is composed of fibers of the C5, C6 and C7 spinal nerves, passing first as part of the upper trunk, then the posterior bundle of the plexus.
When the C5-C6 spinal nerves or the upper trunk of the brachial plexus (in the supraclavicular fossa) are damaged, as is observed with Erb's palsy, the nerve suffers in combination with n. musculocutaneus.
If the posterior bundle is damaged (in the subclavian fossa), the function n. axillaris is disrupted together with n. radialis.
The motor fibers of the nerve innervate m. deltoideus (et m. teres minor), sensitive - the skin of the outer surface of the shoulder (n. cutanei brachii lateralis).
When n. is affected. axillaris, there is atrophy of the deltoid muscle, the inability to raise the shoulder in the frontal plane to a horizontal line and impaired sensitivity on the skin of the outer surface of the shoulder.
- musculocutaneus (musculocutaneous nerve). The nerve is mixed and is also formed from fibers of the C5-C6-C7 spinal nerves, passing through first the upper trunk, then the external fascicle of the brachial plexus.
When the C5-Cb spinal nerves or the upper trunk of the plexus (in the supraclavicular fossa) are damaged, as happens with Duchenne-Erb's palsy, it suffers in combination with n. axillaris.
If the external bundle is damaged (in the subclavian fossa), loss of function n. musculocutaneus is observed in conjunction with partial damage to I. mediani, its upper leg (weakening of pronation and palmar flexion of the hand).
The motor fibers of the nerve innervate m. biceps brachii (as well as m. brachialis et m. coracobrachialis), and sensitive - the skin of the outer (radial) surface of the forearm (n. cutanei anlebrachii lateralis).
When n. is affected. musculocutanei, atrophy of m occurs. bicipitis, the flexion-elbow reflex fades and flexion of the forearm is significantly weakened (it is completely impossible in the pronation position, since in the supination position or the average between them, flexion in the elbow joint can be carried out due to the contraction of the m. brachioradialis, innervated by the n. radialis.
Sensitivity disorders are observed on the outer (radial) surface of the forearm.
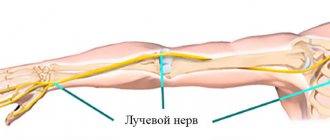
- radialis (radial nerve ). The mixed nerve arises mainly from the fibers of the C7 spinal nerves (partly from C5, C6, C8 and T1), passing first as part of the middle trunk, then the posterior fascicle of the brachial plexus.
With damage to the C7 spinal nerves or the middle trunk, the main function of the nerve (except for the m.brachioradialis et m.supinator) is lost in combination with partial damage to the n.mediani, its upper leg (weakening of pronation and palmar flexion of the hand)
When the posterior bundle of the brachial plexus is damaged, the same basic functions of n. radialis, but in combination with damage to n. axillaris.
Motor fibers n. radialis innervates the extensors of the forearm (m. triceps et m. anconeus), hand (mm. extensores carpi radialis et carpi ulnares) and fingers (mm. extensores digitorum), the supinator of the forearm (m. supinator), the abductor pollicis muscle (m. abductor pollicis longus) and so on brachioradialis, which takes part in the flexion of the forearm. Sensitive fibers innervate the skin of the posterior surface of the shoulder (n. cutaneus brachii posterior), the dorsal surface of the forearm (n. cutaneus antebrachii dorsalis), the radial side of the dorsum of the hand and partially the first, second and sometimes third fingers.
With high damage n. radialis in the axillary fossa, in the upper third of the shoulder, paralysis of the extensors of the forearm, hand, main phalanges of the fingers, and the abductor pollicis muscle occurs; flexion of the forearm (m. brachioradialis) is weakened. The reflex from the m tendon fades away. triceps and the carporadial reflex is somewhat weakened (by turning off the contraction of the m. brachioradialis). Sensitivity is lost on the dorsal surface of the shoulder, forearm, and partly the hand and fingers. The zone of sensory disorders on the hand is often significantly reduced due to the overlap of the zone with the innervation of neighboring nerves. The joint-muscular feeling does not suffer. At lower levels of damage, the nerve function suffers to a limited extent, since the higher branches are preserved, which facilitates the tasks of topical diagnosis.
When the nerve is damaged, which is very common, at the level of the middle third of the shoulder, the function of extension of the forearm and the extension-ulnar reflex (m. triceps) are preserved and sensitivity in the shoulder is not impaired.
If the lower third of the shoulder is affected, the function of the m. brachioradialis and sensitivity on the dorsal surface of the forearm (n. cutaneus antebrachii dorsalis), since the corresponding branches extend from the main trunk of the nerve higher, in the middle third of the shoulder. When a nerve is damaged in the forearm, the function of n. brachioradialis et i. cutanei antebrachii dorsalis is usually preserved; loss is limited to damage to the extensors of the hand and fingers with sensory impairment only on the hand. With damage even lower, in the middle third of the forearm, loss of motor function can be even more limited; while extension of the hand is preserved, only extension of the main phalanges of the fingers may suffer.
When the radial nerve is damaged, weakness of the wrist extensors develops, and a typical falling or drooping hand occurs.
Among the numerous descriptions of samples or tests that determine movement disorders with damage to the radial nerve, the following can be noted:
- Inability to straighten the hand and fingers.
- Inability to abduct the thumb.
- When the hands are folded together with the fingers straightened, the fingers of the affected hand are not retracted, but the bent ones seem to “slide” along the palm of the healthy, abducted hand.
- ulnaris (ulnar nerve ). The nerve is mixed, made up of fibers of the C8-T1-T2 spinal nerves, passing through first the lower trunk, then the internal bundle of the brachial plexus.
With damage to the spinal nerves C8—T1—T2 of the lower trunk and the internal bundle of the brachial plexus, the function of the nerve suffers equally in combination with damage to the cutaneous internal nerves of the shoulder and forearm (nn. cutanei brachii et antebrachii mediates) and partial dysfunction of n. mediant, its lower leg (weakening of the tenor flexor muscles), which creates the clinical picture of Dejerine-Klumpke palsy.
The motor function of the nerve mainly consists of palmar flexion of the hand, flexion of fingers V, IV and partly III (mm. lumbricales, flexor digitorum profundus, interossei, flexor digiti V), adduction of the fingers, their spread (mm. interossei) and adduction of the thumb ( m. adductorpollicis); in addition, in the extension of the middle and terminal phalanges of the fingers (t. lumbricales. interossei).
With regard to the innervation of the movements of the 1st and 2nd fingers, the function of the ulnar nerve is associated with the function of the median nerve; the first has a predominant relation to the function of the 5th and 4th fingers; the median nerve to the function of the 2nd and 3rd fingers. Sensitive fibers innervate the skin of the ulnar edge of the hand, V and partially IV, and less often III fingers.
Complete damage to the ulnar nerve causes weakening of the palmar flexion of the hand (flexion is maintained partially due to the m. flexor carpi radialis et m. palmaris from the n. medianus), lack of flexion of the IV and V, and partly of the III fingers, the impossibility of bringing and spreading the fingers, especially the V and IV, inability to adduct the thumb.
Superficial sensitivity is usually impaired on the skin of the fifth and ulnar half of the fourth fingers and the corresponding ulnar surface of the hand.
The joint-muscular feeling is upset in the little finger. Pain with damage to the ulnar nerve is not uncommon, usually radiating to the little finger. Possible cyanosis, sweating disorders and a decrease in skin temperature in an area approximately coinciding with the area of sensory disorders. Atrophy of the muscles of the hand with damage to t. ulnaris appears clearly, depression of the interosseous spaces, especially the first, as well as a sharp flattening of the hypotenor are noticeable.
As a result of the defeat of mm. interossei et lumbricalis, the hand takes the form of a “clawed bird’s paw”; with hyperextension of the main phalanges, bending of the middle and terminal phalanges is observed, due to which the fingers take a claw-like position. This is especially pronounced in relation to the V and IV fingers. At the same time, the fingers are slightly separated, especially the IV and mainly V fingers.
Its first branches n. ulnaris radiates only to the forearm, so its lesion along the entire length to the elbow joint and the upper part of the forearm gives the same clinical picture.
The lesion in the region of the middle and lower thirds of the forearm leaves the innervation of mm intact. flexor carpi ulnaris et flexor digitorum profundus, due to which palmar flexion of the hand and flexion of the terminal phalanges of the V and IV fingers are not affected. But the degree of “clawedness” of the hand increases.
To determine movement disorders that occur when the ulnar nerve is damaged when the hand is clenched into a fist, the following basic tests are available:
- When the hand is clenched into a fist, fingers V and IV, and partly III, are not bent enough.
- Bending the terminal phalanx of the fifth finger or “scratching” the little finger on the table with the palm tightly fitting to it is not possible.
- It is impossible to adduct the fingers, especially V and IV.
- Thumb test: the patient stretches a strip of paper, grasping it with both hands between the bent index finger and straightened thumb; with damage to the ulnar nerve and, consequently, paralysis of the m. adductoris pollicis adduction of the thumb is impossible and the strip of paper is not held with the straightened thumb. In an effort to hold the paper, the patient bends the terminal phalanx of the thumb with the help of m. flexor pollicis, innervated by the median nerve.
- medianus (median nerve ). The mixed nerve is formed from fibers of the C5, C6, C7, C8 and T1 spinal nerves, passing mainly through the middle and lower trunks of the brachial plexus. Subsequently, the fibers of the median nerve pass in the external and internal bundles. The upper leg of the n. extending from the external bundle. mediani and from the internal bundle its lower leg merge, forming a loop of the median nerve.
When the C7 spinal nerve or the middle trunk of the brachial plexus is damaged, the function of the median nerve suffers partly as a result of weakening of wrist flexion (m. flexor carpi radialis), pronation (mm. pronalores) in combination with damage to the radial nerve.
Almost the same loss of function n. mediani occurs when the external bundle of the brachial plexus is damaged, into which the fibers of the upper peduncle of the nerve pass from the middle trunk, but in combination with damage to the musculocutaneous nerve.
With damage to the C8-T1 spinal nerves, the lower trunk and the internal bundle of the brachial plexus (Dejerine-Klumpke palsy), they suffer in combination with damage to n. ulnaris, n. cutanei brachii el anlebrachii medialis fibers n. medianus, which make up its lower leg (weakening of the flexors of the fingers and tenor muscles).
The motor function of the nerve mainly consists of pronation, palmar flexion of the hand due to contraction of m. flexor carpi radialis el m. palmaris longus flexion of fingers, mainly I, II and III (mm. lumbricales flexor digitorum sublimis el pmfundus, flexorpollicis), extension of the middle and terminal phalanges of II and III fingers.
Sensory fibers etc. mediani innervate the skin of the palmar surface of the I, II, III and radial half of the IV fingers, the corresponding part of the palm, as well as the skin of the rear of the terminal phalanges of these fingers.
When the median nerve is damaged, pronation suffers, palmar flexion of the hand is weakened (preserved only by the m. flexor carpi ulnaris from n. ulnaris), flexion of the I, II and III fingers and extension of the middle phalanges of the II and III fingers (mm. lumbricalis, inlerossei) are impaired. . Superficial sensitivity is impaired in the hand in an area free from the innervation of the ulnar and radial nerves. Articular-muscular sensation is always impaired in the terminal phalanx of the index, and often in the second finger. Muscle atrophy with damage to the median nerve is most pronounced in the tenor area. The resulting flattening of the palm and bringing the thumb close and in one plane to the index finger create a peculiar position of the hand, which is called “monkey”.
Pain when the median nerve is damaged, especially partial, is quite intense and often takes on a causal nature. In the latter case, the position of the hand may become bizarre. Vasomotor-secretory-trophic disorders are also common and characteristic of lesions of the median nerve: the skin, especially the 1st, 2nd and 3rd fingers, becomes bluish or pale in color; nails become “dull”, brittle and streaked; skin atrophy, thinning of fingers (especially II and III), sweating disorders, hyperkeratosis, hypertrichosis, ulcerations, etc. are observed. These disorders, as well as pain, are more pronounced with partial rather than complete damage to n. medianus.
Its first branches n. medianus, like n. ulnaris, radiates only to the forearm, so the clinical picture with high damage along the entire length from the axillary fossa to the upper parts of the forearm is the same.
When n. is affected. mediani in the middle third of the forearm, in which the branches extending to mm. pronator leres, flexor carpi radialis, palmaris longus flexor sublimis, the functions of pronation, palmar flexion of the hand and flexion of the middle phalanges are not affected. With lower nerve lesions, the function of flexion of the terminal phalanges of the I, II and III fingers may also be preserved.
The main tests to determine movement disorders arising from damage to the median nerve are the following:
- When squeezing the hand and fist, fingers I, II and partly III do not bend
- Bending the terminal phalanges of the thumb and index fingers is impossible, as is scratching the index finger on the table with the hand tightly fitting to it.
- During the thumb test, the patient cannot hold a strip of paper with a bent thumb and will hold it by adducting with a straightened thumb (mm. adductor policis from retained n. ulnaris).
- cutaneus brachii medialis (cutaneous internal nerve of the shoulder ). A sensory nerve, the fibers of which arise from C8, T1, partly from T2 spinal nerves and pass through first the lower trunk, then the internal bundle of the brachial plexus and innervate the skin of the inner surface of the shoulder. When it is damaged, sensory disturbances and pain in the shoulder area occur.
- cntaneus antibrachii medialis (cutaneous internal nerve of the forearm). Sensory nerve. Innervates the skin of the inner surface of the forearm. It is formed from the C8-T2 spinal nerves.
When the nerve is damaged, sensory disturbances occur, and possibly pain in the forearm area.
Isolated lesions of these nerves are rare. Their damage is often included in the clinical picture of damage to the lower trunk or internal bundles of the brachial plexus or is observed in combination with damage to other nerves of the limb.
The main challenge that must be resolved to select appropriate treatment is to determine the level of damage as accurately and early as possible.
Indications for neurosurgical operations are clinical signs of severe upper and total paralysis, Horner's syndrome, relaxation of the diaphragm, lack of restoration of motor and sensory functions of the upper limb in infants. The most optimal age of patients for neurosurgical operations is the first year of life. For operations on the brachial plexus, the transverse supraclavicular approach and its modifications, as well as the transclavicular one, are used. The methods of choice for neurosurgical operations are external and internal neurolysis, plastic surgery and suture of nerves, neurotization
A comparison of groups of children treated only conservatively and with the use of neurosurgery showed that the latter significantly improves outcomes.