Neurolysis
- an operation during which the nerve is freed from the tissues compressing it. These can be adhesions, scars, bone calluses. Neurolysis surgery helps restore nerve conduction that has been disrupted for one reason or another. The main reason for the formation of obstructive tissues is injury and inflammation. In this case, the process affects the surrounding elements, damaging nerves, blood vessels, and soft tissues. The result is the formation of hard fibrous scars that compress the nerves and prevent impulses from passing normally through the tissues.
In what cases is it performed?
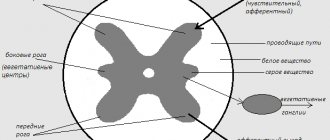
Neurolysis of the nerve is aimed at releasing it and restoring the impaired function of the limb. There is external and internal neurolysis:
- External is used when the scar has not penetrated deep into the nerve trunk.
- Internal is necessary when scar tissue grows between the fibers of the nerve that needs to be released.
There are many options depending on which nerve needs to be worked. Neurolysis of peripheral nerves is required after injuries, household or industrial injuries:
- Ulnar Nerve Area – Problems in this area are common and cause serious problems for the patient.
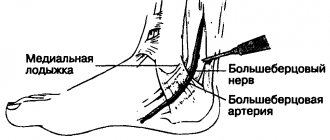
- The area of the median nerve under the knee greatly affects sensitivity.
- Radial nerve area - eliminating the problem of a hanging hand.
- Peroneal nerve area - to eliminate paralysis that prevents extension of the foot.
- Operations are also performed in the areas of the facial nerve, recurrent laryngeal nerve, etc.
Medical Internet conferences
Damage to the recurrent nerve as a postoperative complication after surgery on the thyroid gland
Kiseleva E.V.
Scientific supervisor: Doctor of Medical Sciences, Associate Professor Kuligin A.V.
GBOU VPO Saratov State Medical University named after. IN AND. Razumovsky Ministry of Health of the Russian Federation
Department of Emergency and Anesthesiology and Resuscitation Care
The majority of thyroid lesions require surgical treatment, one of the common complications (20%) of which is injury to the recurrent laryngeal nerve.
Purpose of the study. Optimization of diagnosis of damage to the recurrent laryngeal nerve in the postoperative period in patients after surgery on the thyroid gland from the position of an anesthesiologist
Materials and methods. Articles and reports of doctors involved in the diagnosis of intraoperative damage to the recurrent nerve during surgery on the thyroid gland were analyzed. An analysis of diagnostic methods for the identified complication was carried out.
Results. According to the literature, the frequency of this complication varies widely from 0.2 to 15%. Of the data provided by surgeons, it was 3.7%, otolaryngologists - 4.2%, anesthesiologists - 5.7%. In 15%, the identified complication required a tracheostomy. The most common injury to the recurrent nerve was observed during thyroidectomy. Most cases of damage to the recurrent nerve are not diagnosed intraoperatively, and suspicion arises in the immediate postoperative period, with the development of a characteristic clinical picture. Patients complained of difficulty breathing, phonation disturbances, and difficulty speaking. The reliability of these data was influenced by which specialist made the diagnosis of this complication: the operating surgeon, otorhinolaryngologist, or anesthesiologist-resuscitator, as well as based on the clinical picture alone or using instrumental research methods, the diagnosis was established. Treatment of the resulting complication proceeded according to standard generally accepted methods, ending in 77% with complete recovery of patients, but depended on the degree of nerve damage.
Conclusions. An analysis of the literature studied shows that the diagnosis of damage to the recurrent nerve in 80% of cases occurs after surgery and awakening of the patient. The diagnosis is based on the developing clinical picture. Treatment of the identified complication depends on the degree of nerve damage and the severity of clinical symptoms. To optimize the diagnostic search for damage to the recurrent nerve, it is necessary to improve intraoperative diagnostics on the part of the anesthesiologist and otorhinolaryngologist.
Carrying out the operation
The operation is carried out in several stages:
- Introduction of anesthesia.
- Opening the connective tissue with a scalpel along the entire length of the nerve.
- Detection of fiber bundles, excision of the scar between them.
- Access to the nerve is open, it is isolated from the surrounding tissues.
- The scarring area is determined by palpation. The scar is found and removed.
- Excision can be carried out only over the nerve, bypassing the sides, to avoid damage to blood vessels and other structures.
- Application of miniature sutures.
- Placement of the nerve into the resulting muscle space.
- After these manipulations, the tightness disappears, and previously lost sensitivity appears.
Method of microsurgical plastic surgery of the recurrent nerve
The invention relates to medicine, namely to surgery. Intraoperative monitoring and neurolysis of the recurrent nerve are performed. If there are epineural lesions or it is impossible to ensure complete neurolysis of the recurrent nerve, its resection is performed. Next, the vagus nerve is cut off, the site of excision is determined based on the required length of the vagus nerve for anastomosis with the distal end of the resected recurrent nerve. By rotating the vagus nerve, it is passed in a heterotopic direction to the distal end of the resected recurrent nerve. An anastomosis is performed between the recurrent and vagus nerves using an epineural suture. The method expands the arsenal of means for plastic surgery of the recurrent nerve.
The proposed invention relates to medicine, in particular to surgery, and concerns a method for microsurgical plastic surgery of the recurrent nerve.
Damage to the recurrent nerve is a very serious and most common complication during operations, for example, on the thyroid gland, and can also be a consequence of nerve damage during tumor processes. Even unilateral damage to the recurrent nerve can be accompanied by dysphagia (impaired swallowing). In this case, food may be thrown into the trachea, which is fraught with the development of complications from the lungs (pneumonia, bronchitis). The appearance of a pathological cough, also associated with the reflux of gastric juice into the larynx, is often noted. All these complications are usually compensated by the intact recurrent nerve on the other side. Operations performed on both lobes of the thyroid gland (so-called thyroidectomy or strumectomy) are dangerous due to bilateral nerve damage with bilateral paralysis of the vocal folds, which leads to impaired spontaneous breathing and requires the imposition of a permanent tracheostomy.
Damage to the recurrent nerves, according to the average statistical data of Russian authors, ranges from approximately 2% to 23%, and according to foreign literature, from 1% to 13%. Unilateral laryngeal paralysis occurs in approximately 4% of patients, and bilateral paralysis occurs in 1%. Injury to the recurrent nerve during hemithyroidectomy occurs in 1-4% of patients, after subtotal resection of the thyroid gland - in 3% of patients, after thyroidectomy - in 5-7%.
Basically, traumatization of the recurrent laryngeal nerves is associated with the release of the latter from the neurovascular bundle and surrounding, including scarred, tissues.
Despite the above data, identification of the recurrent nerves during surgical interventions is performed in only 5% of all operations performed in the world. There are and are used various methods for monitoring the recurrent nerves, which today are considered the most advanced and sensitive and can significantly reduce the percentage of postoperative complications. Methods for monitoring recurrent nerves do not make it easier for surgeons to isolate them from scar tissue and mobilize them from tumor nodes in the thyroid gland. The question also remains open of what to do in the event of a violation of the integrity of the nerve.
The use of microscopes can be considered the most effective way to identify the recurrent nerves, allowing the microsurgical method to isolate and carry out neurolysis of the recurrent nerves and, during surgery, simultaneously perform reconstruction in case of damage to the recurrent nerve with the formation of neural anastomoses.
Among the methods for restoring the integrity and conductivity of peripheral nerves, the following methods can be distinguished:
— plastic surgery of the nerve using tubage from an arterial allograft (G.N.Akuev, G.S.Kokin, I.Chumasov, L.I.Kolosova, etc. J. Issues of neurosurgery. No. 6, 1988, p. 32-36) ;
- suturing of opposite nerves (G.S. Kokin, I.S. Morozov, F.S. Govenko. Zh. Issues of neurosurgery. No. 6, 1988, p. 52-54);
— “neurotization of facial muscles using the methods of Ballance, Khitrov” (A.E. Gutsana, reference book “Maxillofacial operations”, 1997, pp. 121-123);
— autotransplantation (E.I. Zlotnik, E.A. Korotkevich. Zh. Issues of neurosurgery. No. 5, 1986, p. 52-58).
However, each of the above methods has disadvantages:
- wrapping the suture line or tubage with an arterial allograft (omentum, fascia, etc.) to increase the tightness of the anastomosis is fundamentally vicious, since it disrupts the blood supply to the nerve, causes an inflammatory reaction of surrounding tissues and creates additional sources of scarring around the nerve, which significantly complicates regeneration process (G.N. Akuev, G.S. Kokin, E.I. Chumasov, L.I. Kolosova and others. J. Issues of neurosurgery. No. 6, 1988, pp. 32-36; I.D. Kirpatovsky , E.D. Smirnova, “Fundamentals of microsurgical techniques”, 1978, p.107);
- autotransplantation in case of injury to peripheral nerves creates the problem of choosing a donor nerve that is adequate in length, diameter, structure and the appearance of a neurological defect in connection with its removal (E.I. Zlotnik, E.A. Korotkevich. Zh. Issues of Neurosurgery. No. 5, 1986, pp.52-58). For example, when performing cross autoplasty of the facial nerve, most surgeons who used cross facial anastomosis note that the need to use long (13-17 cm) autografts is a negative factor, and the regeneration process may be ineffective due to impaired revascularization of autografts and their scarring.
We consider the method of plastic surgery of the recurrent nerve to be the closest to the proposed method for the purpose of rehabilitation of vocal and respiratory disorders after surgical interventions, proposed by E.I. Trofimov. and others (Trofimov E.I. et al., Correction of persistent vocal and respiratory disorders after surgical interventions on the thyroid gland. Thyroid cancer and endemic goiter: materials of an interregional conference with international participation. Yekaterinburg, 2007, p. 137-138) . This method includes, among other things, monitoring and neurolysis of the recurrent nerves during surgery.
However, the known method has a number of disadvantages: for example, even if neuromonitoring of the recurrent nerves is carried out in practice, it is not always possible to isolate the recurrent nerve from scar and tumor tissues without damaging it, which, in turn, leads to disturbances in vocal and respiratory function in patients with postoperative period.
The technical result of the proposed method is the possibility of performing microsurgical plastic surgery of the recurrent nerve in order to restore vocal and respiratory function, as well as increasing the effectiveness of the intervention through the use of anastomosis between the vagus and recurrent nerve. The use of the vagus nerve for the purpose of microsurgical plastic surgery allows plastic surgery to be performed if necessary, resection of the recurrent nerve along almost its entire length, since when using the method, the excess length of the vagus nerve is straightened. In addition, the proposed method allows you to create a shorter reflex arc, and due to the possibility of moving the vagus nerve, perform anastomosis in any required location.
The method we propose is as follows.
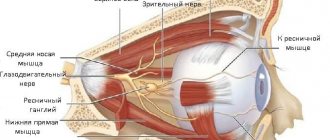
When performing a surgical intervention, for example, aimed at removing the thyroid gland, or its lobe, or removing lymph nodes, intraoperative monitoring and neurolysis of the recurrent nerve are carried out. If there are epineural lesions or it is impossible to ensure complete neurolysis of the recurrent nerve, its resection is performed. Next, the vagus nerve is cut off, the site of excision is determined based on the required length of the vagus nerve for anastomosis with the distal end of the resected recurrent nerve. By rotating the vagus nerve, it is carried out in a heterotopic direction, that is, in a direction that is unusual/non-physiological for this nerve, to the distal end of the resected recurrent nerve, directing the axon to the area of the vocal cords. An anastomosis is performed between the recurrent and vagus nerves using an epineural suture.
The above method can be used in patients undergoing both primary and repeated surgical interventions, including the method can be used in patients who have previously received other types of treatment for the underlying disease (for example, radiation therapy) or for the correction of voice and vocal disorders. /or respiratory function.
The advantages of the proposed method over previously known ones are as follows:
- in order to restore nerve function, and therefore respiratory and vocal function, reinnervation of the larynx is used using the vagus nerve;
- the use of the vagus nerve seems to be the most “physiological”, because anatomically, the recurrent nerve is a branch of the vagus nerve and after an anastomosis between the recurrent nerve and the vagus, the body does not need to “get used to”;
- the use of the vagus nerve makes it possible to perform an anastomosis in the required place, that is, it allows one to calculate the required location for resection of the vagus nerve so that the nerve can be “brought” in the most optimal way (in any case in a heterotopic direction) to the distal end of the resected recurrent nerve;
— when using the proposed method, a shorter reflex arc is formed;
— the intersection of one of the vagus nerves allows you to preserve the basic functions controlled by the vagus.
The possibility of implementing the proposed method can be confirmed by the following clinical example.
Example. Patient Shkunkov V.F., 64 years old, was undergoing inpatient treatment in the microsurgery department of the P.A. Herzen Moscow Scientific Research Institute of Orthography since 10/12/07.
Clinical diagnosis: thyroid cancer with metastases to the lymph nodes of the neck on the right. Condition after combined treatment in 1968. Relapse with metastases to the paratracheal lymph nodes.
Morphology No. 3123/07p puncture of a formation in the bed of the right lobe - papillary thyroid cancer.
Anamnesis: from the anamnesis it is known that regarding a goiter of the thyroid gland in the hospital named after. Botkin in March 1968, an operation was performed in the following volume: strumectomy of the thyroid gland (according to discharge). Histological examination revealed papillary thyroid cancer. Sent to MNIOI named after. P.A. Herzen, where, due to the non-radical nature of the operation, a plan for combined treatment was developed. At the first stage, RT with SOD 35 Gy was performed. At the second stage, an operation was performed including hemithyroidectomy on the right, resection of the left lobe of the thyroid gland, lymphadenectomy on the neck on both sides (according to discharge). At the beginning of 2007, he noted the appearance of hoarseness. Was treated conservatively without effect. Due to the increasing severity of hoarseness, I turned to the Moscow Research Institute of Orthopedics named after. P.A. Herzen.
Upon admission: upon examination: hoarseness is noted, there are no breathing difficulties. There are old postoperative scars on the neck on the right, left and below. Against the background of scar changes without additional formations.
Ultrasound: in the right paratracheal region there is a hypoechoic zone 17×14×15 mm, the structure is heterogeneous, the contours are unclear. In the pretracheal region, an oval-shaped zone with clear contours is visualized, indistinguishable from thyroid tissue.
CT: a CT examination of the chest organs pretracheally identifies a single lymph node up to 1.0 cm. No focal or infiltrative changes were found in the lung tissue.
When examining the neck, the left lobe and isthmus are structurally unchanged. In the bed of the right lobe, a nodular formation measuring up to 1.2 cm is detected paratracheally. Conclusion: The CT picture is suspicious for a relapse in the bed of the right lobe of the thyroid gland or metastasis to the paratracheal lymph node.
FBLS: upon examination, immobility of the larynx on the right. All elements of the larynx are differentiated - without pathology.
The clinical situation was discussed at an interdepartmental consultation with the participation of surgeons, radiologists and chemotherapists. Taking into account the examination data, the amount of previous treatment, the histological structure and extent of the tumor process, it is recommended: surgical treatment.
The following surgery is planned: reoperation on the thyroid gland, lymphadenectomy of the anterosuperior mediastinum.
The patient's consent for the operation was obtained. There are no contraindications to the operation.
On November 7, 2007, the patient underwent reoperation on the thyroid gland: thyroidectomy. Resection and microsurgical plastic surgery of the recurrent laryngeal nerve on the right. Removal of lymph nodes and tissue of the anterosuperior mediastinum.
Under the ETN, a skin incision was made on the anterior lower surface of the neck according to Kocher with excision of the old postoperative scar. The skin flap is separated upward. The anterior muscles of the neck are cut. During the audit: the thyroid gland is represented by the left lobe, pyramidal lobe, isthmus and part of the right lobe; in the pyramidal lobe a nodular formation up to 1 cm in diameter is determined; in the right tracheoesophageal groove, a metastatically changed lymph node up to 2.5 cm in size with infiltrative growth around it is determined, involving the right recurrent laryngeal nerve in the infiltrate. Upon further inspection, a metastatic lymph node up to 1.5 cm in diameter was revealed in the pretracheal area.
Considering the involvement of the right recurrent laryngeal nerve in the process and the right-sided paresis of the right half of the larynx, it is recommended: resection of the right recurrent laryngeal nerve with microsurgical plastic surgery. The thyroid gland with its pyramidal lobe, a metastatic lymph node in the right tracheo-esophageal groove with resection of the right recurrent laryngeal nerve were removed using a single block, sharp and blunt. The right vagus nerve was isolated and separated for 4 cm and cut off at the intersection with the subclavian vein. The vagus nerve is rotated and carried in a heterotopic direction to the distal end of the recurrent nerve resection, the axon is directed to the region of the vocal cords. Using microsurgical technique, an anastomosis was performed between the vagus and recurrent laryngeal nerves on the right. The left recurrent laryngeal nerve was isolated and traced along its length. Using video endoscopic technology, para- and pretracheal lymph nodes and tissue of the anterosuperior mediastinum were removed. Careful hemostasis. The wound is sutured in layers, leaving 2 tubular drainages in the bed of removed tissue.
A follow-up examination was performed 3 months after the operation. Vocal and respiratory function has been completely restored.
Thus, the proposed method can significantly improve the possibilities of postoperative rehabilitation of functions controlled by the recurrent nerve, including the vocal and respiratory nerves, by performing microsurgical plastic surgery of this nerve with an anastomosis between the recurrent and vagus nerves.
A method of microsurgical plastic surgery of the recurrent nerve, including intraoperative monitoring and neurolysis of the recurrent nerve, characterized in that the recurrent nerve is resected, the vagus nerve is cut off on the same side where the recurrent nerve was resected, rotating the vagus nerve is carried out in a heterotopic direction to the distal end of the resected recurrent nerve, and an anastomosis is performed between the vagus and recurrent nerves.
Rehabilitation after neurolysis
Recovery after the intervention begins with the restoration of sensitivity and the cessation of painful sensations. This happens by relieving pressure on the nerve. All other functions are restored somewhat more slowly. The sooner the operation is performed, the easier the rehabilitation will be. After the operation, gradually:
- The functionality of the nerve improves or is completely restored.
- The pain disappears.
- The ability to feel is restored.
- Sweating returns to normal.
Examination before reconstruction surgery
Electromyography
Electromyography is a research method based on such an indicator as the difference in bioelectric potentials arising in the patient’s muscles.
It is used for a comprehensive assessment of damage to the neuromuscular system, as well as the condition of the nerve and the speed of impulse transmission along it, and damage to the nerve by one or another disease. It can be performed either using needle electrodes inserted into the muscle or using cutaneous electrodes.
MRI neurography
MRI neurography is an examination using MRI technology that provides a three-dimensional image of the main peripheral nerves and allows you to determine to what extent and how they have been damaged. It was invented as a way to reliably supplement electromyography data.
MRI neurography uses special software and equipment with the highest resolution.