Features and classification
One of the known variants of cardiomyopathy is ventricular dilatation.
Expansion of cavities occurs in many patients for no apparent reason. As a result, the superficial function of the myocardium is disrupted, which leads to a rapid increase in its size. The appearance of dysfunction is associated with a decrease in the strength of contractions of the muscular wall of the ventricles. At the same time, there is a decrease in the release of blood into the aorta. During the examination of some patients, the thickness of the heart wall does not change when the cavities are dilated. The following options for dilatation of the left ventricle of the heart are distinguished:
- tonogenic;
- myogenic.
With tonogenic dilatation, expansion of the heart cavity is noted due to increased blood flow to them and increased pressure. The myogenic form is characterized by an irreversible change in the volume of the chamber. It appears against the background of elongation of fibers and their stretching with a simultaneous lack of contractility.
The latter variant of dilatation is most often combined with a decrease in wall tone. It is divided into primary and secondary. The first form develops with myocarditis in acute or chronic stages, cardiosclerosis caused by atherosclerosis. During primary expansion, the cavity grows uniformly in size. The function of myocardial contraction is significantly reduced. The pulse and heart rate become weak and difficult to feel.
The secondary form occurs against the background of established myocardial hypertrophy. The size of the heart is significantly increased in comparison with the primary one.
There are many factors that have a negative effect on the myocardium, but there are certain conditions that contribute to dilatation of the left ventricular cavity:
- Pathology associated with damage to the myocardium itself.
- Excessive load.
Some patients are characterized by an asymptomatic course of the disease against the background of complete health. Over time, if it is impossible to compensate for the condition, signs of the disease appear. This is typical for dilated cardiomyopathy. Other causes are inflammation, arterial hypertension, which over time make the muscle wall weak. This condition leads to loss of elasticity and excessive extensibility, which leads to dilatation of the cavity.
Overload of the left chamber of the heart occurs when the functioning of the valve that opens into the aorta is disrupted. The narrowing creates an obstruction to the flow of blood, which over time leads to stretching of the heart tissue and dilatation of the cavity.
This condition is observed in people with defects in which a large volume of blood enters the ventricle.
Left atrium
The left atrium has a cylindrical shape, its volume in newborns is 4-5 cm3, by the end of the year it reaches 10-14 cm3, by 7-9 years 24-32 cm3, by 18-25 years - 90-135 cm3. The size of the left atrium depends on age. In children under 1 year of age, the anteroposterior size is 0.8-1.7 cm, in children under 6 years old - 0.8-2.2 cm, under 12 years old - 1.0-2.2 cm, under 17 years old - 1.1-2.2 cm. The width of the left atrium in children under 1 year of age is 1-1.17 cm, in children under 6 years old - 1.1-2.1 cm, 7-12 years old - 1.3- 2.1 cm, 13-17 years old - 1.5-2.3 cm.
One-dimensional echocardiography of the left atrium
In one-dimensional mode, the anteroposterior size of the left atrium is visualized in the IV standard position. In this position, the ultrasound beam crosses the area of the left atrium adjacent to the atrioventricular orifice.
Semiotics of the left atrium
Increased left atrium diameter
- Patent ductus arteriosus.
- Ventricular septal defect.
- Mitral valve insufficiency.
- Mitral valve stenosis.
- Supravalvular mitral ring.
- Restrictive cardiomyopathy.
- Hypertrophic cardiomyopathy.
Decrease in left atrium diameter
- Left ventricular hypoplasia syndrome.
- Total anomalous drainage of the pulmonary veins.
- Compression of the left atrium by an extracardiac mediastinal tumor.
- Large atrial septal defect.
- Myxoma of the left atrium.
- Tetralogy of Fallot.
- Ebstein's anomaly.
- Double origin of the great vessels from the right ventricle.
Increased excursion of the posterior wall of the left atrium
Associated with an increase in transmitral blood flow in various physiological and pathological conditions.
- Mitral valve insufficiency.
- Initial stages of hypertension.
- Hyperkinetic cardiac syndrome.
- Sports heart.
Additional echoes in the left atrium cavity
- Supravalvular mitral ring.
- Left atrial thrombus.
- Separation of tendon threads from the anterior mitral leaflet.
- Separation of tendon threads from the posterior mitral leaflet.
- Myxoma of the left atrium.
- Floppy mitral valve.
- Mobile bacterial vegetations of the mitral valve.
Two-dimensional echocardiography of the left atrium
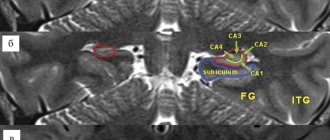
The left atrium is studied in several sections: parasternal section of the long axis of the left ventricle, in the projection of 4 chambers from the apex and from the epigastric approach. Pay attention to the shape of the chamber (normally it should be oval), the presence of intracavitary formations, and the relationship with the left ventricle.
Right ventricular dilatation
One of the reasons for the expansion of the cavity is considered to be insufficient functioning of the valve apparatus. A similar condition is typical for patients who have suffered endocarditis or rheumatism, where damage to the leaflet structures was a complication. Dilatation of the right ventricle occurs in the absence of the pericardium, which occurs in some patients.
The result of this pathology is gradually stretching of the muscle fibers. The altered septum between the atria leads to dilation of the artery in the lungs. An increase in pressure in this vessel indicates an increase in pressure in the cavity of the right ventricle.
Defects also negatively affect the chamber of the heart. They contribute to increased pressure in the pulmonary artery. This process ends with dilatation due to a deficiency of compensatory functions of the body.
Interventricular septum
Functional anatomy of the interventricular septum
The interventricular septum separates the left ventricle from the right, has a complex spherical structure, and makes up 1/3 of the total mass of the ventricles. The radius of curvature of the septum is the same as that of the free wall of the left ventricle. On both the left and right ventricular sides, the septum has a triangular shape (Fig. 67). In functional and morphological terms, the septum is divided into 4 sections: inflow (inlet), outflow (outlet), trabecular and membranous portions. The first three sections form the muscular part of the septum. The membranous part of the septum forms the medial wall of the left ventricular outflow tract: on the side of the right ventricle, the anterior and septal leaflets of the tricuspid valve are attached to it. The inflow section forms the medial wall of the inlet tract of the left and right ventricles, respectively, the outflow section of the IVS forms the outflow tract of the left and right ventricles. Between the inflow and outflow sections is the trabecular part of the septum.
One-dimensional echocardiography of the interventricular septum
In a one-dimensional study, the interventricular septum is visualized as a strip of linear echo signals separating the cavity of the right ventricle from the left. During systole, the septum moves towards the posterior wall of the left ventricle and thickens. The nature of the movement and the thickness of the partition in one-dimensional mode are determined in the first standard position (Fig. 68).
Fig.67
Scheme of the functional and morphological sections of the interventricular septum from the right (a) and left (b) ventricles.
1 - inflow section (in let), 2 - outflow section (out let).
Along with this, the fraction of systolic thickening of the IVS is calculated: F IVS = { (Tc - Td) / T } * 100%
, where
Fig.68
Scheme of normal movement of the interventricular septum.
F IVS - fraction of systolic thickening (in %), Tc - IVS thickness in systole, Td - IVS thickness in diastole (cm, mm). Normally, F IVF ranges from 30 to 80%.
Semiotics of the interventricular septum:
Hypertrophy of the interventricular septum
Fig.69
Hypertrophy of the interventricular septum (diagram). An increase in diastole thickness of the septum by more than 5 mm in children under 1 year of age, more than 8 mm in children under 3 years of age, and more than 10 mm in children over 3 years of age. It can occur from the right and left ventricles or be isolated (Fig. 69).
Causes of right-sided IVS hypertrophy
- Pulmonary hypertension (primary, secondary).
- Open atrioventricular canal.
- Tetralogy of Fallot.
- Isolated pulmonary artery stenosis.
- Eisenmenger syndrome.
Causes of left-sided IVS hypertrophy
- Arterial hypertension.
- Hypertrophic cardiomyopathy (obstructive, non-obstructive).
- Athletic heart (hypertrophy of the interventricular septum in athletes).
- Aortic stenosis (subvalvular, valvular, supravalvular).
- Restrictive cardiomyopathy (cardiac amyloidosis, cardiac hemochromatosis, endocardial fibroelastosis).
Causes of isolated IVS hypertrophy
- Idiopathic hypertrophic subaortic stenosis.
- Initial stages of arterial hypertension.
- Intramural tumor of the IVS.
Pseudohypertrophy of the IVS:
- Incorrect orientation of the IVS (with anomalies in the position of the heart) or violation of the research technique (visualization of the septum at a large scanning angle).
- Parietal thrombus.
- Longitudinal trabeculae along the interventricular septum.
- Intracavitary tumor adjacent to the interventricular septum.
- Bacterial vegetation on the septum.
Hypokinesia of the interventricular septum
Fig.70
Hypokinesia of the interventricular septum (diagram). Normally, the systolic excursion of the IVS is 4-9 mm) (Fig. 70).
- Carditis, cardiomyopathies.
- Conditions associated with volume overload of the right ventricle (cor pulmonale, ASD).
- Congestive heart failure.
Hyperkinesia of the interventricular septum
Fig.71
Hyperkinesia of the interventricular septum (diagram). Increase in systolic excursion over 10 mm (Fig. 71).
- Mitral insufficiency of any etiology.
- Hyperkinetic cardiac syndrome (mitral valve prolapse, vegetative-vascular dystonia).
- Conditions associated with volume overload of the left ventricle (PDA, VSD).
- Small pericardial effusion.
Paradoxical movement of the interventricular septum
Fig.72
Variants of paradoxical movement of the interventricular septum.
The following types of paradoxical movement of the IVS are distinguished (Fig. 72):
Type A
- the septum moves in the opposite direction during systole (concordant with the posterior wall of the left ventricle) (Fig. 73);
Type B
- (otherwise referred to as variable motion) at the beginning of systole, the septum moves paradoxically, then has a flattened backward movement.
Fig.73
Paradoxical movement of the interventricular septum in atrial septal defect. Types A and B of paradoxical motion are usually combined with volume overload of the right ventricle. A close relationship between the degree of volumetric overload and the type of movement of the IVS has not been established, however, in practice, type A movement corresponds to a greater degree of overload.
Passive paradoxical movement of the IVS
— throughout the entire systole, the septum makes a slow forward movement, while its systolic thickening is practically absent
Abnormal movement with left bundle branch block
- this variant is manifested by rapid diastolic movement back at the beginning of systole, then the septum moves as in type A paradoxical movement.
The main conditions accompanied by paradoxical movement of the IVS:
- Volume overload of the right departments:
- Atrial septal defect (primary, secondary).
- Abnormal drainage of the pulmonary veins (partial, complete).
- Ebstein's anomaly.
- Pulmonary valve insufficiency.
- Open atrioventricular canal.
- Tricuspid valve insufficiency.
- Congenital absence of the pulmonary valve.
- Fistula of the right coronary artery into the right ventricle.
- Idiopathic dilatation of the pulmonary artery.
- Left ventricular hypoplasia syndrome.
- Anomalies of the cardiac conduction system:
- Wolff-Parkinson-White syndrome type B.
- Left bundle branch block.
- Ventricular arrhythmias.
- Pacemaker in the right ventricle.
- Pericardial pathology:
- Congenital partial absence of the pericardium.
- Constrictive pericarditis.
- Idiopathic aneurysm of the right atrium.
- Pleuropericardial adhesions.
- After heart surgery:
- After suturing or repair of VSD.
- After radical correction of tetralogy of Fallot.
- After mitral valve replacement.
- After aortic valve replacement.
- Other reasons:
- Corrected transposition of the great vessels.
- Arrhythmogenic right ventricular dysplasia syndrome.
- Tumors of the right ventricle.
- Dyskinetic segments with anomalies of coronary circulation.
- Hypertrophic cardiomyopathy with left ventricular outflow tract obstruction (LVOT).
- Dilated cardiomyopathy.
- Endocardial fibroelastosis.
Symptoms
Moderate expansion of one or two chambers in the heart may not manifest itself for a long time. Often, pathology is discovered by chance, during a routine examination or treatment of another disease. Severe dilatation of the cavity leads to a decrease in pumping function, which leads to the appearance of signs of heart failure or arrhythmia. These include the following:
- Palpable palpitations.
- Dyspnea.
- Blueness of the nasolabial triangle, lips, earlobes, fingertips.
- As the severity of the course worsens, cyanosis spreads to the skin.
- Swelling in the arms and legs.
- Memory impairment.
- Fatigue and weakness that persists after rest.
- The appearance of discomfort when lying down.
- Dizziness.
- Headache.
- Feeling of interruptions in the heart.
Shortness of breath in the compensation stage appears only with excessive physical exertion. With gradual wear and tear of the myocardium, the condition worsens. Shortness of breath begins to bother you with slight exertion, and then at rest.
With chronic exposure to unfavorable factors, a change occurs in the myocardium, which leads to a gradual expansion of the cavity and thickening of the walls. Dilatation of the left ventricle of the heart in the absence of timely therapy increases the risk of complications. Most often, thrombosis and fibrillation of the ventricles or atria are observed.
In some patients, the valve apparatus is affected, which is manifested by expansion of the ring, deformation of structures and ends in the formation of acquired heart disease.
After the transition from the stage of compensation to decompensation, fluid appears in the abdominal cavity (ascites), and the size of the liver increases (hepatomegaly). The skin of such patients becomes damp and cold to the touch. Systolic blood pressure decreases. Tachycardia is noted.
When auscultated, wheezing is heard in the lungs. Determination of the boundaries of the heart shows cardiomegaly (increase in heart size), the rhythm is disturbed.
results
The majority in both groups were men, but in contrast to the group of patients with normal pancreatic size, men were more common in the group with pancreatic dilatation. Patients in this group showed a tendency toward older age (Table 1).
Table 1. Comparative characteristics of clinical, functional and laboratory parameters of patients with coronary artery disease without myocardial infarction, depending on the presence of pancreatic dilatation Note. Here and in the table. 2: data are presented as mean ± standard deviation or number of patients (in%). SBP—systolic blood pressure; DBP—diastolic blood pressure; FC - functional class; NYHA - New York Heart Association; nd - statistically insignificant differences.
The groups did not differ in the frequency of smoking, alcohol consumption, levels of SBP and DBP, the frequency of detection of arterial hypertension, diabetes mellitus, hypothyroidism and heredity burdened with ischemic heart disease. The average BMI in both groups corresponded to obesity, but in patients with a dilated pancreas it was statistically significantly higher. Patients with RV dilatation more often demonstrated a higher (III) FC of CHF according to the New York Heart Association (NYHA) classification, as well as NRPS with less frequently detected severe (III-IV) FC of exertional angina. There were no intergroup differences in basic laboratory parameters and coronary angiography data. When analyzing EchoCG parameters in patients with dilated RV, higher indices of the linear dimensions of the heart and LV myocardial mass were revealed with no statistically significantly different index of the thickness of the interventricular septum and a tendency towards a lower index of thickness of the posterior wall of the LV. The groups did not differ in the LV asynergia index; the LV ejection fraction was lower in the group with an enlarged RV. Dilatation of the left ventricle, a decrease in its contractility, as well as significant mitral regurgitation and signs of atherosclerotic lesions of the aorta were more often detected in patients with dilatation of the right ventricle (Table 2).
Table 2. Comparative characteristics of echocardio-, electrocardio- and angiographic parameters of patients with coronary artery disease without myocardial infarction, depending on the presence of RV dilatation Note. * — degree of coronary lumen stenosis >75%.
According to the results of multivariate analysis, an independent relationship with RV dilatation was demonstrated by a decrease in myocardial contractility, male gender, NRPS, significant mitral regurgitation, an increase in the FC of CHF and BMI, as well as a decrease in the FC of angina pectoris (Table 3).
Table 3. Parameters independently associated with pancreatic dilatation in patients with coronary artery disease without myocardial infarction
Causes
Dilation of the chamber in the left ventricle often occurs under the influence of several provoking factors. This condition is directly related to the patient’s age, heredity, and the presence of excess body weight. The reasons that negatively affect the myocardium are:
- Congenital heart defects. Exposure to unfavorable environmental factors occurs already during pregnancy. If the lesion becomes extensive, the fetus dies. In the case of a slightly pronounced lesion, a defect is formed.
- Inflammatory diseases, which include myocarditis, pericarditis, endocarditis. The risk group includes children and adolescents, in whom cases of this pathology are often recorded.
- Chronic diseases of the cardiovascular system. These include arterial hypertension, angina pectoris, ischemia.
- Metabolic syndrome, the basis of which lies in the presence of excess body weight and diabetes mellitus in the patient.
- Chronic pathology of lung tissue.
- Diseases of the kidneys, endocrine and hematopoietic systems.
- Genetic predisposition.
- Autoimmune disorders.
One of the common factors of dilatation is chronic intoxication with alcohol and nicotine.
This group also includes side effects from medications. Pheochromocytoma is the most common endocrine pathology. It is a benign or malignant form of tumors. It is characterized by excessive production of adrenaline.
Forecast
Every patient with left ventricular dilatation, already knowing what it is, must follow all medical recommendations. With this diagnosis, early diagnosis and initiation of treatment are important. In advanced forms, there is a high probability of developing heart failure. In these same patients, the valve apparatus is deformed, which leads to mitral insufficiency. This diagnosis significantly affects the quality of life and reduces its duration. The prognosis for patients is unfavorable.
The average survival rate for left ventricular dilatation is 10 years. If the course is asymptomatic, then life expectancy is on average 5 years. Patients with chronic heart failure observed in the hospital survive up to 50% of those admitted.
It is important for each patient to remember that the first symptoms are not considered normal and require a set of diagnostic procedures. Timely treatment will reduce the risk of complications, and treatment will prolong life for many years.
Materials and methods
Of the 16,839 patients included in the “Registry of Coronary Angiography Operations” [5] from 1998 to 2013, patients with stenosis of >75% of the lumen of at least one coronary artery, without acute or anamnestic myocardial infarction, without congenital and acquired heart defects: 75 patients with RV dilatation and 1134 without it. The transverse size of the pancreas in the parasternal position was 26 mm or less [6]. For a clearer division of the groups, patients with pancreatic dilatation included patients with a pancreatic size of 30 mm or more; patients with a slight enlargement of the pancreas (>26 and <30 mm) were not included in the study. A clinical, comprehensive echocardiographic examination was performed (one-dimensional, two-dimensional, Doppler echocardiography using Imagepoint NX ultrasound devices, Agilente Technologies, Phillips, USA; Vivid 3, 4, 7, 9 Systems, Vingmed-General Electric - Horten, Norway), determination of lipid composition of blood serum, Holter monitoring, selective coronary angiography according to Judkins (1967) (angiographic complexes Diagnost ARC A, Poly Diagnost C, Integris Allura, Phillips, Holland). Linear echocardiography (EchoCG) parameters were indexed to height; myocardial mass, calculated using the Devereux formula, to the body surface area [7]. Echocardiographic syndromes were diagnosed according to standard criteria: the LV was considered dilated when its end-diastolic diameter index was more than 32 mm/m2 in women and more than 33 mm/m2 in men [2], LV systolic function was reduced when the LV ejection fraction was less than 50%, hemodynamically significant mitral regurgitation (≥II degree) - with an effective area of the regurgitant orifice ≥0.2 cm2, regurgitant volume ≥30 ml [8].
Statistical processing of data was carried out using a package of applied statistical programs (SPSS Inc., version 17.0). Indicators are presented in the form M
±
SD
_
The distribution of variables was determined using the Kolmogorov–Smirnov test. To compare values with their normal distribution, t
; for a non-normal distribution, the nonparametric Mann-Whitney test was used.
When analyzing qualitative indicators, Pearson's χ2 test was used. Differences at p
<0.05 were assessed as statistically significant. Multivariate analysis was performed - binary logistic regression analysis with calculation of odds ratio (OR).