© Author: A. Olesya Valerievna, candidate of medical sciences, practicing physician, teacher at a medical university, especially for SosudInfo.ru (about the authors)
Post-traumatic encephalopathy is a complex complex of general cerebral and focal neurological disorders, combined with intellectual-mnestic and behavioral reactions in response to brain injury.
Brain damage after injury can be chronic and progressive, contributing to disability and death of the patient, but most often occurs in a relatively mild form, not life-threatening, but delivering a lot of unpleasant symptoms to the victim. Without literally disrupting life activity and self-care, such encephalopathy, however, forces the patient to systematically visit a doctor, undergo courses of treatment and change their lifestyle, and sometimes work.
Emotional disturbances create discomfort in communicating with loved ones and colleagues, insomnia aggravates the feeling of tiredness and fatigue, and any, even the most minor stress or strain can provoke a surge in psychopathological symptoms, neurosis, asthenia or depression.
An important feature of post-traumatic encephalopathy is the fact that in some cases it does not appear immediately, but months and even years later. Establishing a connection between changes in nervous activity and a previous injury can be very difficult, and if the patient hit his head 10-15 years ago, he himself may not immediately remember what happened and may not connect past events with the symptoms that have appeared.
According to some data, signs of post-traumatic encephalopathy against the background of moderate and severe brain injuries appear sooner or later in 70-80% of patients, while the severity and severity of changes depend on the treatment performed and how quickly it was started. Timely and correct diagnosis is extremely important, as well as a set of treatment and preventive measures aimed at preventing disability and death.
Causes and pathogenesis of post-traumatic encephalopathy
The main cause of traumatic brain injury is traumatic brain injury:
- Brain contusion due to falls, road accidents, blows with a blunt object (in a fight or by accident);
- Participation in contact sports (traumatic boxer encephalopathy is the most common type);
- Birth injuries in newborns.
Changes in the brain are usually diffuse in nature, caused by hypoxia and degenerative-dystrophic changes in nerve cells, impaired impulse transmission, and loss of contacts between individual groups of neurons.
In morphological terms, a decrease in the density of brain tissue, dystrophic changes in neurons, microinfarctions, loss of myelin sheaths by neuron processes, and the formation of glial nodules are considered to be a reflection of post-traumatic encephalopathy. Externally, in severe forms of the disease, hemispheric atrophy, a decrease in brain size, and an expansion of the ventricular system may be noticeable.
General information
Encephalopathy occurs due to metabolic disorders in brain cells. Regardless of the cause, the pathology follows a single scenario. First, there is a decrease in the activity of neurons, then their gradual death. Foci of dystrophy are located throughout the brain, which causes a variety of symptoms.
The damage is irreversible, but with timely consultation with a specialist and quality treatment, the patient’s condition can improve. The remaining intact neurons partially take over the function of the dead cells, and brain function is significantly improved. If the disease was caught at an early stage, the patient retains complete clarity of mind.
Make an appointment
Severity and manifestations of consequences of brain damage
Depending on the severity of brain disorders, it is customary to distinguish three degrees of post-traumatic encephalopathy:
- I - the mildest, manifested by minimal disorders, which may not be noticeable externally and during communication, but the patient himself feels tired, may sleep poorly, and be apathetic;
- II degree - signs of emotional instability appear, attention and memory decrease, insomnia, depressive disorders, asthenia, which are periodic in nature, are not uncommon;
- III degree - the most severe and unfavorable, accompanied by obvious neurological symptoms - seizures, parkinsonism, loss of coordination, paresis, a sharp decrease in intelligence, psychosis, etc.
in the photo: an example of the consequences of regular head injuries in an athlete, a professional American football player, chronic traumatic encephalopathy
The diagnosis of the disease must indicate the depth of the disorder and characteristic manifestations (paralysis, paresis, dementia, etc.). Post-traumatic encephalopathy does not have its own category in the International Classification of Diseases, but its ICD 10 code is T90.5 (consequences of a traumatic brain injury).
Sometimes you can see another code - G93.8, which includes some specified diseases of the brain and may include post-traumatic encephalopathy. The patient and his relatives do not need to know these designations, but they may appear on the certificate of incapacity for work and other medical documents.
The symptoms of post-traumatic encephalopathy are extremely diverse and fit into several syndromes:
- Hypertensive-hydrocephalic;
- Convulsive;
- Astheno-vegetative;
- Vestibulopathy and parkinsonism;
- Progressive dementia.
Depending on the severity of the injury, symptoms may be subtle or more pronounced. Manifestations will also be more pronounced in patients with existing vascular lesions (atherosclerosis, hypertension), which are more often diagnosed in older people.
The most common complaint of patients who have suffered severe head injuries is cranialgia, which is not relieved by taking the usual analgesics. With hydrocephalic syndrome, the headache occurs in the morning, and at its height, vomiting is possible, which does not make the patient feel better.
Constant headaches, loss of strength, difficulties in performing intellectual tasks aggravate the already increasing asthenia, provoke neurotic disorders, and deplete the nervous system. Characteristic sleep disturbances include insomnia, restless sleep with frequent awakenings, and daytime sleepiness.
During physical activity, dizziness is clearly manifested, although in severe forms of brain damage it, along with headaches, can be a constant concern. With concomitant atherosclerosis of the cerebral arteries, these symptoms will be even more pronounced.
Violations of the vestibular apparatus cause involuntary movements, twitching of individual muscle groups, instability of position and unsteadiness of gait, signs of parkinsonism. For example, it is difficult for a patient to start moving, but once he starts it, he can hardly stop.
A patient with post-traumatic encephalopathy needs outside help, which he has to ask for more and more often, which is why depressive syndrome increases. Mood changes, unmotivated aggression or deep despondency are common. The patient may withdraw into himself, giving up usual activities and hobbies, communication with loved ones, who become uninteresting. At the same time, many patients become hypercommunicative with strangers, to whom they describe in detail and colorfully the situation at home, their own well-being and vision of the world, which can bring a lot of problems to the family.
One of the early symptoms of brain damage after injury is a decrease in attention and memory. Patients lose logic, the ability to analyze and coherent thinking. New information is perceived and remembered with great difficulty. Slow speech with active gesticulation is typical; patients seem to answer simple questions at random, and their thoughts are confused.
Personality disorders boil down to a loss of the ability to introspect, decreased self-criticism, and lack of will. Intellectual impairment is especially severe for those people whose profession is associated with intellectual stress and concentration. In severe cases of encephalopathy, these symptoms necessitate recognition of the patient as disabled.
The emotional and volitional spheres suffer in the absolute majority of victims of traumatic brain injury. Behavior is disrupted, inappropriate behavior and actions appear, patients are whiny or euphoric, impulsive, and often aggressive towards others.
A severe manifestation of post-traumatic encephalopathy is convulsive syndrome. Convulsions can be generalized, with loss of consciousness, are not always amenable to drug treatment and themselves contribute to even greater structural changes in the nervous tissue.
Autonomic symptoms are also a frequent accompaniment of post-traumatic encephalopathy. Characterized by sweating, a feeling of heat, redness of the skin or severe pallor, tachycardia, stool disorders, and fluctuations in blood pressure.
With deep encephalopathy, patients need constant monitoring and care, but while they are able to move and act independently, relatives may suffer from their aggressiveness, litigiousness, and uncontrollable actions.
Post-traumatic encephalopathy with dementia is accompanied by a complete loss of thinking and motivation, dysfunction of the pelvic organs; many patients simply lie down, occasionally falling asleep for a short time. They often refuse to eat or lose the ability to eat, which leads to severe exhaustion that can cause death.
The diagnosis of encephalopathy cannot be made only on the basis of symptoms, because a similar clinical picture occurs in other diseases with brain damage. It is very important to establish the fact of an injury in the past, especially if more than one year has passed since it was received.
Additional diagnostic methods are MRI, CT, electroencephalography for seizures. These procedures make it possible to more quickly exclude other causes of encephalopathy, since changes in nervous tissue are often stereotyped. MRI can reveal signs of hemispheric atrophy, deepening of the grooves, expansion of the liquor spaces, areas of rarefaction and microinfarctions in the brain.
Additional methods in differential diagnosis are ultrasound with Doppler of the vessels of the head and neck, echoencephalography, biochemical blood tests, including hormone tests. Consultations are carried out with other specialists - narcologist, psychiatrist, cardiologist, urologist.
examples of brain damage in post-traumatic encephalopathy
Alarming symptoms
The main task of diagnosis is to determine the dominant syndrome, taking into account its most obvious signs. For example:
- With asthenia, the patient quickly gets tired, feels drowsy, suffers from emotional instability and constantly experiences headaches.
- Hypersthenia causes the patient to be overly nervous and irritable in relation to external influences, and hyposthenia, on the contrary, makes a person indifferent and weak.
- Pathopsychological syndrome leads to neurotic personality disorders. The patient may fall into a state of depression or hypochondria; in severe cases, even paranoia is noted. Encephalopathy also leads to impaired cognitive functions, causing a person to lose performance. In some cases, it is impossible to do without the services of a professional nurse.
- The syndrome of impaired cerebrospinal fluid dynamics is associated with the appearance of post-traumatic hydrocephalus. Due to the accumulation of fluid in the brain, a person regularly experiences headaches and nausea.
- In the presence of vegetative-dystonic syndrome, complaints of tachycardia and changes in blood pressure arise. This condition is also associated with disturbances in the functioning of the endocrine system (for example, failure of the menstrual cycle or excessive sweating).
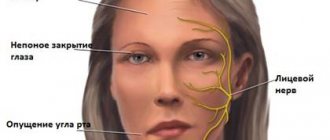
- Cerebrofocal syndrome is characterized by damage to the facial, ocular and auditory nerves. The person experiences problems with movement, even to the point of paralysis. Additionally, changes in sensitivity may occur.
- Epileptic syndrome becomes noticeable due to the appearance of seizures. Often attacks are accompanied by aggressive behavior and increased irritability.
How is post-traumatic encephalopathy treated?
The course of the pathology and the consequences for the patient largely depend on how quickly and how well qualified care is provided. It is important not only to eliminate specific symptoms, but also to ensure the maximum possible trophism and arterial blood supply to neurons. Treatment for traumatic encephalopathy includes:
- The use of neuroprotectors to protect neurons from the effects of hypoxia;
- Restoring adequate blood supply to nervous tissue;
- If possible, eliminate the symptoms of the disease - seizures, paresis, depression, etc.
Conservative therapy for traumatic damage to nervous tissue is often symptomatic and aimed at eliminating specific manifestations of the disease. Complex treatment is long-term, consists of courses repeated 1-2 times a year, and many drugs are prescribed for life.
Hydrocephalus is a common consequence of severe brain injury. In hydrocephalic syndrome, the main task of neurologists is to reduce intracranial pressure, which is achieved by prescribing diuretics (mannitol, diacarb, furosemide, glycerin). As the pressure in the skull decreases, the patient's condition improves significantly.
For convulsive syndrome, anticonvulsants are necessarily used - finlepsin, diazepam, clonazepam, etc. Their dosage and regimen must be accurately calculated by a neurologist, taking into account contraindications, which are quite serious for this group of drugs.
Neuroprotection is the most important direction of treatment, which should be started at the first signs of brain damage. Nootropics and neuroprotectors help increase the level of metabolism in neurons, have a protective antihypoxic effect, and reduce the damaging effect of free radicals on nerve cells.
Nootropics increase memory and attention, help the patient quickly adapt to intellectual stress, and increase stress resistance. The most popular drugs with this effect are piracetam (nootropil), mildronate, encephabol, Cerebrolysin, Cortexin, Semax. Actovegin is used to improve blood circulation.
Vitamins B, PP, and nicotinic acid, prescribed in courses of tablets or injections, help speed up the transmission of impulses by nerve cells and, accordingly, eliminate some intellectual-mnestic disorders.
For headaches and vestibular disorders, neurologists prescribe analgesics and non-steroidal anti-inflammatory drugs - ibuprofen, analgin, askofen. Betaserc helps combat dizziness.
Drug treatment is carried out in parallel with physiotherapy and psychotherapy. It is very important to change your lifestyle and eliminate existing bad habits. Patients are shown massage (especially with paresis and paralysis, muscle hypertonicity, pain syndrome), physical therapy under the supervision of a specialist.
To improve oxygenation, breathing exercises are prescribed; walking in the fresh air is very useful, which should become an integral component of the daily regimen of a patient with traumatic encephalopathy.
Some of the most common symptoms of brain damage after injury are mental changes, including severe depression, psychosis, and insomnia. In this regard, most patients need to work with a psychotherapist (individual or group), as well as the use of appropriate medications (rexetine, melipramine, diazepam, phenazepam, etc.). Psychotropic drugs are prescribed only by a specialist, and patients themselves can use those drugs that do not require a prescription - motherwort, valerian, sedatives and teas.
Another important step towards eliminating the manifestations of traumatic encephalopathy is a change in lifestyle. So, the patient should forever give up bad habits, if any, since nicotine and alcohol have an extremely negative effect on already suffering neurons.
Adequate, feasible physical activity, a balanced diet rich in microelements and vitamins, adequate sleep, daily walks and independent psychological training help in the fight to restore efficiency and intelligence. Patients who were engaged in intellectual work before the injury actively solve crosswords and mathematical problems, memorize poetry, try to read as much as possible so that memory, attention and intellectual abilities become acceptable for their usual level of functioning.
Surgical treatment of post-traumatic encephalopathy is not widespread, since with closed injuries diffuse damage to the entire brain often occurs. In the case of hematomas in the acute period, decompressive trepanation and drainage of the cavity with blood can be performed, but this operation is aimed more at saving life and preventing cerebral edema than at eliminating signs of encephalopathy.
Post-traumatic encephalopathy must be treated for a long time, following all the doctor’s recommendations, this is the only way to hope for positive dynamics. However, unfortunately, the patient is not always able to get rid of negative symptoms, and the pathology can cause disability, which is indicated in cases where the disease limits the ability to work. The severe consequences of brain damage prevent military service, driving a car (convulsive syndrome, for example), and working with machinery.
Therapy for post-traumatic brain injuries is aimed, rather, not at a complete cure, but at slowing the progression of the pathology. The effect may not be noticeable immediately, and many symptoms will become permanent. At the same time, you should not despair and stop taking medications or visiting a doctor. In many ways, the level of rehabilitation depends on loved ones who can help the patient cope with depression, apathy, and indifference to the environment.
The prognosis for traumatic encephalopathy depends on the degree of brain damage, response to treatment, the initial state of cerebral vessels and nervous tissue, the patient’s age and lifestyle. It can be adequately assessed only a year after the injury. With relatively mild forms of pathology, you can count on the restoration of many brain functions, ability to work and sufficient activity in everyday life.
A progressive course and severe degrees of encephalopathy can limit life activity and require the establishment of a disability group - from first to third. With the first degree of brain damage, disability, as a rule, is not established. With the second, disability group II or III is possible, while the patient can perform light and safe work or is exempt from it completely. In severe cases of traumatic encephalopathy, the patient needs to be assigned disability group I, cannot work and requires outside care and assistance.
Why does the violation occur?
As a result of TBI, pathological changes in brain tissue occur. As a result of diffuse processes, parts of the cerebral system stop working normally. Signs of encephalopathy for a doctor are as follows:
- hypoxia resulting from vascular disorders;
- changes in the nature of the meninges (fusion with each other, formation of scar tissue members);
- formation of cysts, hematomas;
- increased size of the ventricles of the brain;
- degeneration of glia and neurons.
It is worth considering that encephalopathy can progress and have a greater or lesser degree of severity. The development of the disease is influenced by several factors:
- severity of the lesion;
- the body's ability to recover;
- general health;
- nature of the injury.
Premorbid and genetic factors are also important. It is desirable that the treatment of TBI itself be timely and effective. In this case, complications can be avoided.
Possible complications
Post-traumatic encephalopathy produces various complications depending on the dominant syndrome and characteristics of the course of the disease. Schematically, the types of possible adverse reactions can be presented as follows:
- Vegeto-dystonic syndrome - hypertension and cerebral atherosclerosis.
- Psychopathological, liquorodynamic and asthenic syndromes - deterioration of cognitive functions, increased fatigue, personality disorders.
Encephalopathy significantly reduces the patient’s standard of living and does not allow him to feel like a full-fledged member of society.
Preventive measures
If encephalopathy was diagnosed on time and properly treated, the likelihood of complete healing of the patient is very high. However, a positive outcome is observed only if the brain damage was not too deep. An additional factor influencing the possibility of recovery is maintaining a correct lifestyle.
To avoid relapses and worsening of the condition, the patient should:
- follow all doctor’s recommendations during the treatment of intracranial injury;
- give up cigarettes and alcoholic beverages;
- avoid re-injury.
Athletes should stop working out during recovery, and representatives of law enforcement agencies should take a vacation.