The simplest single-celled organism, Naegleria Fowler, usually lives in fresh water bodies with warm water. During bathing, this parasite can enter the human body through the nasal cavity, then through the olfactory canal it enters the brain area. As a result, this organism causes such a rare but very dangerous pathology as amoebic meningoencephalitis.
During this pathological process, damage to nerve cells, necrosis of the meninges, as well as swelling and hyperthermia of the brain are observed. As a result, the formation of purulent exudate around the bulbs occurs. This disease usually has a poor prognosis, often accompanied by death. Each person exhibits different symptoms, their intensity and severity depends on the degree of damage to the nervous system. Therefore, it is imperative to know the main causes and symptoms of this disease so as not to become infected with this terrible pathology.
This is what amoebas look like
Features of the disease
The causative agent of this disease is the amoeba naegleria; this protozoan organism belongs to the group of eukaryotes or nuclear unicellular organisms of the flagellar type. This simple organism lives in stagnant waters of ponds, reservoirs, and pools with insufficiently chlorinated water. This type of organism lives mainly in soils with high humidity.
The causative agent of amoebic meningitis is a facultative protozoan, which means that the amoeba can live quietly in the environment, and if it enters the human body, it will further parasitize inside the human body.
An amoeba can live for a long time in a cyst, in a protective shell. This usually happens when unfavorable living conditions arise, for example, if a reservoir is drained. The microbe can live inside the cyst for several years, and it can easily tolerate temperatures up to 45 degrees. In this state, the body can endure wind over long distances; cysts with microbes are often found in air conditioner humidifiers, in chlorinated or unboiled drinking water. But it is worth noting that this organism becomes dangerous when it enters the flagellar stage.
If you drink water that contains the causative agents of amoebic meningitis, the microbes will simply be digested in the stomach. The main period during which the process of infection by the parasite occurs is considered to be summer time, the height of the swimming season. The pathogen can enter the body even if air is inhaled at this time.
This is how the amoeba gets into the brain
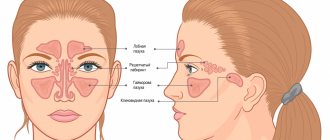
The amoeba moves into the brain area according to the following scheme:
- the pathogen enters the nasal cavity along with dirty water;
- further, it penetrates into the olfactory nerve;
- after this, the parasite penetrates the brain area, its membrane and all parts - the cerebellum, brain stem and the upper parts of the spinal cord.
Symptoms
Amebic meningoencephalitis can also occur in people with excellent health. Almost anyone, both adults and children, can become infected with this terrible pathology. The incubation period is from 2 to 10 days.
Typically, amoebic meningitis appears within 7 days after infection; during this period the following symptoms may be observed:
- Pain in the throat area.
- A dry cough may appear.
- Problems with smell.
- The appearance of vomiting, which does not bring relief.
- Migraine.
- There may be an increased degree of excitability.
- High body temperature.
These symptoms usually appear in other diseases, so this pathology can easily be overlooked or attributed to another disease. For this reason, examination of amoebic meningitis at the initial stage is quite difficult. Patients may think that this is a simple cold, for this reason they may not come to the doctor for a long time for diagnosis. After just 10 days, the following disorders of a neurological nature may be observed:
- increased tone of muscle fibers in the back of the head;
- the occurrence of seizures;
- problems with consciousness;
- manifestation of visual hallucinations;
- epileptic seizures;
- the occurrence of blindness;
- hearing problems, complete deafness may occur;
- coma state.
Amoeba in an approximate state
In the subsequent period, the causative agent of the disease, amoeba naegleria, begins to actively develop and multiply. In the course of its life, it quickly eats brain cells, for this reason, if treatment is not carried out in a timely manner, this can lead to death. It is worth noting that the mortality rate from this pathology is very high; patients cannot be saved in 90% of cases. The main reason for the increased mortality is that this disease is quite difficult to diagnose because the clinical signs are similar to those of bacterial meningitis. Often death occurs within 3–7 days after the first signs of this disease appear.
Meningoencephalitis: ICD code 10
ICD-10 is a normative document with a generally accepted statistical classification of medical diagnoses that is used in healthcare.
According to the international classification, meningoencephalitis is included in the following codes:
- G04.2 - Bacterial meningoencephalitis and meningomyelitis, not elsewhere classified;
- G05 - Encephalitis, myelitis and encephalomyelitis in diseases classified elsewhere. Includes: meningoencephalitis and meningomyelitis.
Granulomatous form of amebic meningoencephalitis
What causes granulomatous type meningitis? The causative agent of this form is still the same - amoeba naegleria, but only the routes of infection occur through contact and airborne droplets. The parasite enters the human body through the pores of the skin and the mucous layer. This type of disease develops quite slowly, the first symptoms may appear several weeks or even several months after infection. This pathological process mainly affects people with a weakened immune system, as well as people with chronic diseases.
Amoebic meningitis in the granulomatous form has the following characteristic features:
- Weakness of the muscle fibers of one part of the body.
- Seizures of an epileptic nature.
- Disorder of consciousness.
- Changes in behavior may be noted.
- A large number of ulcers and nodes with a dense structure may appear on the surface of the skin.
- Increased tone of muscle fibers in the back of the head.
During this pathological process, hyperthermia and headaches do not occur. When performing CT and MRI, multiple lesions that resemble embolic infarctions may be noted on the image.
Brain damage determined by various hardware studies
Amoebic keratitis
Amoebic keratitis is an infection of the cornea caused by Acanthamoeba sp., typically occurring in contact lens wearers.
Acanthamoeba sp. may cause chronic and progressive keratitis in the normal host. The main risk factor (85% of cases) is the use of contact lenses, especially if you swim in the lenses or if you use non-peryl lens solution. Some infections are the result of damage to the cornea.
The lesions are typically very painful and give the sensation of a foreign body. Initially, the lesions have a tree-like appearance resembling herpes simplex keratitis. Later, patchy stromal infiltrates and sometimes a characteristic ring-shaped lesion appear. There is usually preexisting uveitis. Vision deteriorates.
The diagnosis is confirmed by analysis of scrapings from the cornea using Giemsa staining or tricolor staining and test culture on special media. A test culture test for the virus is done if herpes is suspected.
Diagnostic features
Since this pathology is quite dangerous and the patient’s death can occur at almost any time, it is important to diagnose this disease immediately after the first symptoms appear.
Features of examination at the primary stage of amoebic meningitis:
- to identify primary amoebic meningoencephalitis, bacterioscopy of fluid in the spinal cord and bacteriological blood culture are performed;
- if the patient has this pathology, then an increased level of red blood cells, protein, leukocytes will be found in his cerebrospinal fluid, and a reduced concentration of glucose will also be noted;
- Microscopic diagnostics of the liquid is required to determine the presence of mobile microorganisms.
During amoebic meningitis, the greatest damage occurs to the gray matter of the brain. Necrosis of nerve tissue is also observed; a large number of vegetative forms of parasites may be present around the arteries.
The main affected areas may be the diencephalon region and its periphery, or the posterior cranial fossa, which is located in the brain stem area.
Additionally, a lumbar puncture is performed during diagnosis. Increased cerebrospinal fluid pressure is usually noted during this test. The fluid may have a hemorrhagic structure with pronounced neutrophilic pleocidosis.
When collecting information when taking an anamnesis, you must tell the doctor whether you have recently swum in bodies of water. If patients have immunodeficiency, the damage may affect the lung area and skin.
However, in most cases, an accurate diagnosis is usually established after the death of the patient.
Encephalitis
Encephalitis (inflammation of the brain) is one of the most common clinical manifestations of acute neuroviral infections.Introduction
The causative agents of encephalitis can be viruses (measles, rubella, groups of herpes viruses, arbo-, adeno-, enteroviruses, etc.), bacteria (meningococci, mycobacterium tuberculosis, streptococci, etc.), fungi, protozoa. Encephalitis in children should be distinguished from encephalic reactions, which are based on transient dyscirculatory disorders leading to edema and swelling of the brain.
The selectivity of brain damage in encephalitis is to a certain extent due to the neurotropism of the pathogens. Viruses enter the body through airborne droplets and alimentary routes, as well as through mosquito and tick bites, and penetrate the central nervous system when the permeability of the blood-brain barrier is disrupted. When a virus interacts with the body, the following phases are distinguished: adsorption of the virus on cell membrane receptors; virus reproduction (maturation of viral particles) in the cells of parenchymal organs; viremia, which develops as viral particles enter the bloodstream and is based primarily on the interaction between viral antigens and the body’s immune system. In the presence of a certain pathology of the immune system, the permeability of the blood-brain barrier is disrupted, and viruses enter the central nervous system, are adsorbed on cell membranes, penetrate neurons or glial cells, where they reproduce. In this case, it is possible both the destruction of cells with the development of necrotic foci (acute infection), and their relative safety without change or with a change in the genetic code. Constant components of the pathogenesis of encephalitis are edema and swelling of the brain, which can lead to displacement and herniation of the brain stem and damage to vital structures. An essential link in the pathogenesis of many encephalitis is an allergic reaction. In particular, autoantibodies are produced in the body of patients in response to the destruction of brain tissue. Oligodendroglial cells are especially sensitive to this reaction, which leads to demyelination.
There is no generally accepted classification of encephalitis. Currently, they use a classification according to which the group of primary encephalitis caused by the direct effect of the virus on the affected cells includes arboviral (tick-borne and mosquito) encephalitis, as well as encephalitis that does not have a defined seasonality (enteroviral, herpetic, adenoviral, rabies encephalitis ), and epidemic encephalitis. The group of secondary encephalitis includes all infectious-allergic encephalitis (parainfectious, vaccination, etc.), in the pathogenesis of which the leading role belongs to various antigen-antibody complexes or autoantibodies that form an allergic reaction in the central nervous system, as well as a group of demyelinating diseases of the nervous system (acute disseminated encephalomyelitis, Schilder's disease). A special group includes bacterial and rickettsial encephalitis (typhoid, syphilitic), as well as malarial and toxoplasmosis. It is customary to distinguish polioencephalitis with damage to the gray matter of the brain and leukoencephalitis with damage to the white matter. Diffuse damage to the gray and white matter of the brain is called panencephalitis.
The clinical picture of encephalitis includes a combination of general cerebral and focal disorders, although in each individual case one of them may predominate. Clinical manifestations of encephalitis in the acute period depend to a certain extent on the tropism of the pathogen, the predominant localization of lesions and the characteristics of pathogenesis. Damage to more highly organized structures causes particularly severe and persistent changes that can affect all further development of the brain. Therefore, the consequences of encephalitis in children are more pronounced and widespread than in adults.
Primary encephalitis
1. Epidemic encephalitis (lethargic, Economo encephalitis). The name “epidemic” is associated with the widespread epidemic of this encephalitis in 1916-1927. in Europe; Sporadic cases are currently being reported. A slight increase in incidence in winter has been established.
Etiology and pathogenesis. The causative agent is unknown, but the viral nature is confirmed by clinical and morphological parameters. The pathogen is transmitted by airborne droplets, the incubation period is 21-30 days. In the acute stage, pathomorphological changes are of a pronounced inflammatory nature and are localized mainly in the gray matter around the cerebral aqueduct and the nuclei of the hypothalamus. In the chronic stage, changes are predominantly degenerative in nature and are localized in the subcortical nuclei and neurons of the cerebral cortex.
Clinic. Typical clinical manifestations are fever, somnolence and diplopia (Economeau's triad). Fever does not exceed 38-39°C. Drowsiness is combined with stuporous consciousness, but usually the patient can be awakened to eat. Having woken up, he is available for contact, but quickly falls asleep again. In the neurological status, paresis of the oculomotor nerves in the form of ptosis, paralysis of accommodation, miosis, internuclear ophthalmoplegia comes to the fore, and sometimes “doll eyes” syndrome is observed. Vestibular disorders are common, which gave rise to the identification of the form of the same name. Children are characterized by the development of various hyperkinesis (choreiform, athetotic, myoclonic and mixed). In the prepubertal and pubertal periods, hypothalamic disorders in the form of hypersalivation, hyperhidrosis, facial greasiness, and menstrual disorders are also quite common. Psychomotor agitation, a delirious state with delirium are possible, and therefore the “psychosensory” form of the disease is distinguished. Paresis of the limbs is usually not observed, the cerebrospinal fluid is without characteristic changes, and an increased glucose content is noted.
The duration of the acute stage is up to 2-3 months. During the recovery period, asthenia and emotional instability are observed. Classic hypersomnic ophthalmoplegic syndrome of epidemic encephalitis has been rare in recent years; vestibular and influenza-like forms are more often described. The course of all forms of epidemic encephalitis is relatively favorable. Subsequently, some patients develop parkinsonism, usually it occurs within the first year after the acute period, sometimes immediately after it. There is a decrease in motor activity, emotional inertia with intact intelligence, and akinetic-rigid syndrome is typical. Children are also characterized by endocrine-metabolic disorders in the form of delayed physical development, weight loss, obesity, and adiposogenital dystrophy. General cerebral disorders often develop with a decrease in intellectual and mental functions and motor restlessness.
Treatment is pathogenetic, aimed at combating intracranial hypertension, edema and swelling of the brain. B vitamins, immunostimulants are prescribed, and during the period of convalescence - nootropic and anticholinesterase drugs.
2. Eastern tick-borne encephalitis is a disease that primarily affects the medulla oblongata and the cervical enlargement of the spinal cord.
Etiology and pathogenesis. The range of eastern tick-borne encephalitis coincides with the range of the forest tick - Ixodes persulcatus (Far East, Siberia, Urals, Urals, North-West of the European part of Russia). The tick is a reservoir and carrier of the virus. Infection occurs through tick bites (transmissible route) or through consumption of infected goat's milk (alimentary route). Spring-summer seasonality is determined by the biological development cycle of the forest tick. The virus is neurotropic, infecting neurons of the motor cortex of the brain stem and spinal cord. As with other viral infections, virus penetration into the central nervous system is preceded by viremia. The incubation period ranges from 4 to 21 days. Clinical manifestations reflect not so much the stages of virus reproduction as the reaction of the macroorganism to the influence of viral antigens.
Clinic. The onset of the disease is acute. A severe headache appears, fever increases to 39-40°C. Consciousness is impaired (stupor, stupor, coma), and sometimes generalized convulsive seizures appear. Already in the first days, meningeal syndrome is clearly defined. In the cerebrospinal fluid, lymphocytic pleocytosis (150-200.109/l) and a slight increase in protein content are noted. In the blood - leukocytosis, lymphopenia and eosinopenia, ESR up to 40 mm/h. Typically, patients are adynamic, groaning from severe headaches. Against the background of general cerebral disorders, flaccid paresis and proximal-type paralysis quickly form. The picture of upper polioencephalitis or poliomyelitis is typical, and the asymmetry of paresis always remains. Approximately 20% of patients develop pyramidal hemiparesis. There are meningeal, polioencephalomyelitis, cerebral and erased forms.
Diagnostics. Epidemiological data (endemicity of the outbreak, season, sources of infection) are important for diagnosis. The etiological diagnosis is confirmed by virus isolation and serological studies, in particular hemagglutination, complement fixation and neutralization reactions.
Treatment. In the first 3-5 days, the effect is achieved by using human gamma globulin prepared from the serum of those who have recovered from the disease. The dose, depending on age, is 1.5-3 ml for 5-7 days. As a rule, patients should be hospitalized in intensive care units to carry out a set of measures aimed at reducing intoxication, feverish reaction, reducing edema and swelling of the brain. During the period of convalescence, mediators, biogenic stimulants, Cerebrolysin, and nootropic drugs are prescribed. Mortality - 18-25%. In 2-4% of cases, a progressive course of the disease with the development of Kozhevnikov epilepsy syndrome is observed.
3. Western tick-borne encephalitis (two-wave meningoencephalitis) is characterized by predominant damage to the meninges, a two-phase course and a favorable outcome. The range of western tick-borne encephalitis coincides with the range of the pasture tick Ixodes ricunus (Karelian Isthmus, Baltic States, Belarus, Ukrainian Polesie, Urals). The routes of infection are the same as for eastern tick-borne encephalitis. An epidemiological feature is the predominant risk of infection on pastures and when caring for livestock. The proportion of nutritional outbreaks when consuming goat's milk is very high.
Etiology and pathogenesis. The virus has a tropism for glial cells. Neuronal damage is secondary and occurs due to the immunopathological reaction of nervous tissue to virus-induced antigens. Regardless of the route of infection, the virus first multiplies in the internal parenchymal organs and only after 4-10 days it gradually accumulates and multiplies in the brain.
Clinic. The disease begins with chills and intense headache. Appetite disappears, dizziness and insomnia appear. For the first 3-5 days, the fever does not exceed 38°C. In the neurological status, 12-15% of patients show signs of irritation of the meninges, but inflammatory changes in the cerebrospinal fluid are not detected. Then the listed disturbances fade away, the temperature returns to normal. After 6-12 days, after the interfebrile period, headache and vomiting develop again. Against this background, a picture of moderately severe diffuse meningoencephalitis unfolds. The two-phase course is the leading clinical and pathogenetic feature of Western tick-borne encephalitis. Meningeal syndrome is pronounced. Moderate cell-protein dissociation is observed in the cerebrospinal fluid. General cerebral disorders manifest themselves in the form of stupor, sometimes a short-term stuporous state. Reflex asymmetries (pyramidal hemisyndromes) are usually observed. Various cerebellar and extrapyramidal manifestations are more clearly defined already during the period of convalescence. In 4-6% of cases, paresis of the limbs develops in the form of focal myeloradiculoneuritis with almost complete restoration of range of motion. There are general infectious, meningeal, meningoencephalitic and meningoencephalomyelitis clinical forms. A progressive course is not observed.
When diagnosing, first of all, attention is paid to the endemicity of the outbreak, the season and routes of infection. For laboratory diagnosis, the same methods are used as for the diagnosis of eastern tick-borne encephalitis.
Treatment. The main therapeutic measure in the initial period is detoxification. In the second phase of the fight against intracranial hypertension and cerebral hypoxia, the therapeutic effect is achieved with lumbar puncture. During the period of convalescence, B vitamins, biogenic stimulants, and nootropic agents are indicated.
4. Herpetic encephalitis is an acute brain injury caused by the herpes simplex virus, usually type 1 (HSV-1), less often type 2 (HSV-2). Most researchers consider it as a complication of herpes infection.
Epidemiology. Herpetic encephalitis accounts for 11.5% of acute encephalitis. Young children are more likely to get sick. The incidence is sporadic, some researchers indicate an increase in the spring. The infection can be transmitted by droplets and contact.
The uniqueness of the pathogenesis of herpetic encephalitis is due to the fact that infection can occur before or at the time of birth of the child. By about 9 years of age, the vast majority of children experience a latent herpetic infection, so the development of herpetic encephalitis is caused by an exacerbation of the latent infection. Much less often it occurs as a result of an initial encounter with the virus. The herpes simplex virus penetrates the central nervous system through the nerve trunks or hematogenously, in particular through the olfactory nerves, since the process is predominantly localized in the frontotemporal regions and the brain stem. In recent years, hematogenous dissemination of the virus has become increasingly recognized. No less importance is attached to immunopathological reactions, primarily to disorders of cellular immunodeficiency.
Classification. In addition to typical necrotizing encephalitis, pseudotumor and stem forms are distinguished. Encephalomyelitis and generalized herpetic infection with predominant damage to the central nervous system have also been described.
Clinic. The characteristic triad of herpetic encephalitis is an acute febrile onset, the development of Jacksonian-type seizures and impaired consciousness, usually developing after a short-term respiratory infection. Sometimes the sudden development of seizures and loss of consciousness precedes the fever. Focal manifestations occur in the form of paresis of the oculomotor nerves, hemiparesis and various aphasias. In the first 3-5 days of the disease, the composition of the cerebrospinal fluid may be normal. Subsequently, lymphocytic pleocytosis (30-400.109/l) and increased protein content (up to 1.32 g/l) are detected. Leukocytosis is detected in the blood (up to 20.109/l) with a band shift, lymphopenia and high ESR. Comatose state is an unfavorable prognostic sign. Mortality before the use of antiherpetic chemotherapy drugs reached 70-75%, currently it is 20-25%. The proportion of residual effects in the form of convulsive seizures, persistent intellectual impairment of a stationary and progressive nature is high. Infants also develop hydrocephalus and decortication of the brain. The clinical diagnosis is verified by virological and immunological studies aimed at detecting the HSV antigen and specific antibodies, including class J immunoglobulins in blood serum and cerebrospinal fluid.
Treatment. Patients suffering from herpetic encephalitis are hospitalized in intensive care units due to the risk of respiratory distress and dysphagia. The antiviral chemotherapy drug acyclovir (Zovirax, Virolex) is widely used in tablets and ampoules, which for comatose states is prescribed at 10-15 mg/kg per administration every 8 hours. The course of treatment is 7-12 days. At the same time, interferons and immunomodulators are prescribed, as well as corticosteroids (dexamethasone or dexazone, 1-2 mg/kg every 6 hours). The course of treatment is 6-8 days.
5. Cytomegalovirus encephalitis is a rare manifestation of cygomegaly and is characterized by severe brain damage with high mortality and disability.
Etiology and epidemiology. Cytomegalovirus is antigenically related to other herpesviruses. The reservoir of the virus is humans. The virus is released into the external environment with saliva, milk, and urine. However, transplacental transmission of the virus is leading, causing the development of prenatal infection. The frequency of cytomegalovirus encephalitis in children is 2-3% among other forms of acute encephalitis.
Clinic. Cytomegalovirus encephalitis occurs as productive necrotizing meningoencephalitis. Typical manifestations are hypertensive-hydrocephalic syndrome, attacks of clonic-tonic convulsions, and a diffuse increase in muscle tone. The process is characterized by generalization with hepatolienal syndrome and renal failure. Against this background, a bacterial infection occurs. Patients die within 1-2 years.
6. Enteroviral encephalitis is a group of multiseasonal lesions of the central nervous system caused by intestinal viruses of the Coxsackie and ECHO group.
Etiology and epidemiology. The most common viruses that affect the central nervous system are Coxsackie viruses A9, V3, B6, and ECHO viruses (2nd, 11th, 24th, etc.). Viruses are isolated from feces, but can be isolated from nasopharyngeal swabs, cerebrospinal fluid, blood and, in fatal cases, from brain tissue. The source of the infection is the patient, so the infection can be spread by airborne droplets and food. The increase in incidence in countries with temperate climates occurs in the summer-autumn period. The incubation period ranges from several days to 2-3 weeks.
Pathogenesis. After the virus multiplies at the site of entry and then in the lymph nodes, viremia develops with subsequent penetration of the virus into the central nervous system. By analogy with other viral encephalitis, autoimmune reactions play an important role.
Clinic. Enteroviral encephalitis develops acutely in the first 1-3 days, general infectious disorders prevail - fever, headache, lethargy. Fever can occur in two waves with an interval of 1 to 3 days. During this period, general cerebral and meningeal symptoms develop - photophobia, pain in the muscles of the back and abdomen, nausea, and increased headache. In the neurological status, meningeal symptoms are noted, most often stiff neck muscles. In young children, the disease primarily manifests itself as clonic-tonic convulsions, stupor or psychomotor agitation. There are cerebellar, stem and hemispheric forms. The cerebellar form is characterized by a predominance of ataxia of varying severity; movements of the limbs are asynergic and accompanied by intentional trembling. Stem syndrome is expressed in paresis of the oculomotor nerves (diplopia, convergence weakness) and vestibular disorders (nystagmus, dizziness, vomiting). Hemispheric syndrome is characterized by Jacksonian-type seizures, after which hemiparesis develops. In young children, after a series of seizures, stupor or transient coma occurs. Changes in the cerebrospinal fluid are minor; in half of the cases it remains normal. Acutely onset encephalitis usually has a favorable course.
Treatment. Dehydrating agents and interferon are used. In severe cases, corticosteroids and anticonvulsants are indicated.
Secondary encephalitis
Secondary include encephalitis, which occurs mainly during exanthemal infections (parainfectious, post-exanthemal), accompanied by various rashes on the skin and mucous membranes.
1. Measles encephalitis. Measles most often affects children under 5 years of age. The frequency of damage to the nervous system in them is 0.4-0.5%, and in adolescents it is slightly higher. The source of infection is the patient, the transmission route is airborne, the infectious period lasts 8-10 days.
Etiology and pathogenesis. Most researchers adhere to the infectious-allergic genesis of measles and other exanthematous encephalitis, which occurs with predominant damage to the white matter of the brain. The development of encephalitis does not always coincide with the clinical manifestation of measles. Subclinical brain lesions (EEG changes, cerebrospinal fluid pleocytosis) are observed in almost half of measles patients. The possibility of a direct effect of the measles virus on the central nervous system cannot be excluded, as evidenced by its isolation from the brain of individual patients. It should also be borne in mind that subacute sclerosing panencephalitis, also caused by a measles-like virus, is why measles infection of the central nervous system can occur in both acute and chronic forms, similar to a slow viral infection.
Clinic. The typical development of measles encephalitis occurs towards the end of the rash (3-5 days), when the temperature returns to normal. Suddenly, a new rise in temperature occurs and the general condition of the child changes. Drowsiness, adynamia, sometimes psychomotor agitation, then stupor or coma appear. Convulsive seizures are common at an early age. Psychosensory disturbances and hallucinatory syndrome are possible. Focal symptoms vary in localization: hemi- and paraparesis, hyperkinesis, cerebellar disorders. Damage to the optic nerves can reach amaurosis. In most cases, inflammatory changes in the cerebrospinal fluid are also detected in the form of moderate cell-protein dissociation. When the spinal cord is involved in the process, a picture of encephalomyelitis develops. The identification of various symptom complexes is very arbitrary. The prognosis of measles encephalitis depends on the period of measles during which they occur. The worst prognosis is for encephalitis that occurs in the prodromal period: gross organic disorders of the central nervous system remain. Mortality reaches 25%. Encephalitis that occurs during the convalescence phase of measles has a relatively favorable course. Encephalopathies and encephalitic reactions in the form of fever and cerebral manifestations that occur in young children at the onset of measles should be distinguished from measles encephalitis. Short-term convulsions and scattered neurological symptoms are transient and fade away as intoxication decreases.
Treatment. There are no specific treatments for measles encephalitis. Prednisolone and other corticosteroids are prescribed parenterally for 2-4 weeks at a rate of 2-3 mg/kg body weight, desensitizing and dehydrating agents, B vitamins, nootropic drugs. Those who have recovered from measles encephalitis need clinical observation.
2. Chickenpox encephalitis is a rare but severe complication of chickenpox in children.
Etiology and pathogenesis. The causative agent is the varicella zoster virus. Impaired immune reactions play an important role in pathogenesis. The presence of specific antibodies in the early stages of the disease does not prevent the development of chickenpox encephalitis and generalization of the infection, which indicates an infectious-allergic process.
Clinic. Typically, chickenpox encephalitis develops against a background of generalization of the rash, high fever and lymphadenitis. General cerebral disorders appear - lethargy, adynamia, headache, dizziness, vomiting; rarely - generalized convulsions, febrile delirium. Focal paresis is transient. Meningeal symptoms develop in a third of patients. Lymphocytic pleocytosis is observed in the cerebrospinal fluid. Sanitation occurs gradually, no earlier than the 3-4th week from the onset of the disease. In some cases, liquor meningitis syndrome occurs. With the subacute development of chickenpox encephalitis, ataxic and hyperkinetic syndromes are more clearly defined. The first occurs due to damage to the cerebellar structures (nystagmus, intention tremor, loss of coordination). With the progression of disorders, a peculiar dissociation appears between the severity of general infectious manifestations and neurological status, however, starting from the 7-10th day, the process stabilizes, and neurological disorders regress. Pyramidal insufficiency (hemisyndromes, pathological reflexes) persists more persistently. Along with meningitis, children develop encephalomyelitis and gangliopolyradiculoneuritis. The mortality rate for chickenpox encephalitis is 10-12%.
Treatment. First of all, the antiviral drug acyclovir (Zovirax, Virolex) is prescribed in tablets or intravenously, as in the treatment of herpetic encephalitis. Corticosteroids and immunoglobulin are recommended.
3. Rubella encephalitis. The source of infection is a patient with rubella, the route of transmission is airborne droplets.
Etiology and pathogenesis. The infectious period begins 2 days before the rash, the peak of contagiousness decreases with the extinction of the rash. Neurological manifestations in these cases can occur on the 3-4th day of the rash, but sometimes precede them. CNS lesions in congenital rubella can be caused by direct exposure to the virus, as confirmed by its isolation from the cerebrospinal fluid. Encephalitis due to acquired rubella is rare, usually in young children, and is characterized by a severe course and high mortality. In this case, the rubella virus cannot be isolated. The infectious-allergic nature of encephalitis is assumed. It has also been established that the rubella virus can cause progressive panencephalitis.
Clinic. The onset is acute, with the appearance of headache, high fever; characterized by disturbances of consciousness up to deep coma. In the clinic, generalized clonic-tonic convulsions, hyperkinesis of various types, cerebellar and autonomic disorders are noted. Epistatus may develop. Damage to the meninges is permanent. In the cerebrospinal fluid there is moderate pleocytosis with a predominance of lymphocytes, a slight increase in the amount of protein. There are forms of rubella lesions of the central nervous system: meningeal, meningoencephalitic, meningomyelitis and encephalomyelitis. The course of the disease is usually severe. Convulsions may be of a status nature, and disturbances of consciousness may last a week or more. Rubella encephalitis can develop with or without the classic Gregg triad for congenital rubella (cataracts, heart defects, deafness). With acquired rubella in older children, the clinical manifestations are similar, but develop less rapidly. Sometimes the picture of cerebellar ataxia comes to the fore. There are also cases with a chronic course of the process. The laboratory test for diagnosing rubella encephalitis is the presence of high titers of antibodies in the blood serum. Mortality reaches 20%. Death occurs in the first week of illness.
Treatment. There is no specific therapy. The main measures should be aimed at eliminating edema and swelling of the brain (corticosteroids, Lasix, cryoplasma); nootropic drugs are used during the period of convalescence.
4. Encephalitis due to pertussis-diphtheria-tetanus vaccination. It has been established that the DTP vaccine (adsorbed, prepared from killed pertussis microbes and concentrated tetanus and diphtheria toxoid) has a number of side effects, increases the sensitivity of animals to biogenic amines, changes the function of the sympathetic-adrenal system, and can cause various allergic reactions - Quincke's edema, false croup, urticarial rashes. The pertussis component of the vaccine is the most reactive, as it has residual toxicity.
Clinic. Neurological complications occur in the first 24-72 hours after vaccination. The range of clinical manifestations is very wide: collapse or circulatory shock, anaphylactic shock with convulsions, encephalic reactions, encephalopathy, encephalitis. It is characterized by a piercing, monotonous cry at high notes, which can last 1-3 hours or more. It is assumed that it is associated with liquorodynamic disturbances, causing severe headaches. Crying may precede the development of more severe neurological disorders. During collapse, the child suddenly seems to go limp, does not move, turns pale, profuse sweat appears, and sometimes there is a drop in pulse and blood pressure. Convulsive syndrome in some children is one of the components of anaphylactic shock, which usually occurs immediately after vaccination. Typically, seizures are the main symptom of an encephalic reaction and occur at normal or low-grade fever. Repeated, difficult-to-control convulsions may be a manifestation of post-vaccination encephalitis, which begins on the 3rd day after vaccination with high fever, repeated vomiting, and psychomotor agitation. The course of encephalitis is severe, with high mortality and a significant number of residual effects.
Treatment. When neurological symptoms appear, vaccination is stopped. Desensitizing, dehydrating, and for convulsions, anticonvulsant therapy is prescribed. Corticosteroids are used. Those who have recovered from the disease should be monitored at the dispensary. Children with a history of cerebral insufficiency of intra- and postnatal nature must be vaccinated with ADS or ADS-M vaccines, since the latter have little reactogenicity.
5. Encephalitis due to measles vaccination is a rare complication. In fatal cases, cerebral edema is noted, sometimes a picture of Reye's syndrome.
Pathogenesis. The possibility of neurotropism of the measles virus is assumed, but the main role is played by an allergic reaction.
Clinic. Characterized by a violent febrile reaction up to 39-40 C, vomiting, and attacks of tonic-clonic convulsions. Isolated cases of focal encephalitis, meningitis, and cerebellar ataxia have also been described. The prognosis for post-vaccination measles encephalitis is favorable.
Treatment. If seizures occur, phenobarbital is prescribed in minimal doses and desensitization.
6. Encephalitis due to rabies vaccinations. Most often they occur with a picture of encephalomyelitis or myelitis.
Pathogenesis. The main role in the pathogenesis of CNS damage belongs to the allergic reaction of the nervous tissue to repeated administration of the antigen. The assumption of an atypical form of rabies is unlikely, since Negri bodies typical for rabies are never found in the brain.
Clinic. The onset is acute or subacute. The clinical picture is determined by the level of the lesion: with cervical localization, spastic tetraparesis or paralysis occurs; with damage to the thoracic region - lower paraparesis. In older children, focal myelitis is typical. The functions of the pelvic organs are disrupted, and conduction sensitivity disorders occur. When the roots are involved, encephalomyeloradiculoneuritis develops. In more severe cases, there is a rapid and steady increase in neurological symptoms similar to Landry's ascending palsy. The cerebrospinal fluid shows slight lymphocytic pleocytosis and increased protein content. At a later date, protein-cell dissociation is detected. The course is severe, recovery is slow. In severe myelitis, spastic paraparesis often remains. Mortality reaches 15-20%.
Treatment. Hormone therapy and repeated injections of hyperimmune anti-rabies gamma globulin are carried out. Care is extremely important - prevention of pulmonary complications and trophic disorders.
Liana LORINA, Candidate of Medical Sciences. Department of Nervous Diseases and Neurosurgery, Ryazan State Medical University. I.P. Pavlova.
Treatment
Usually, rarely does anyone survive until treatment; many patients die within 5–7 days when infected. This is due to the fact that many people confuse this pathological process with other diseases and, because of this, go to the hospital late.
During the treatment of amoebic meningitis, antibiotic and antifungal agents are used. The most effective include:
- Metronidazole;
- Miconazole;
- Amphoterecin B;
- Rifampicin;
- Aminazine.
During the first period of treatment, drugs are administered intravenously in large dosages. Then they begin to be injected under the membranes of the brain, but the dosage of the drugs is reduced. During therapeutic therapy, anti-Negleria immune serum or monoclonal antibodies are often used.
It is worth considering that the disease develops rapidly, so the clock counts. The doctor should quickly carry out the necessary treatment using the above medications. It is under no circumstances recommended to treat it at home, only in a hospital under the supervision of a specialist.
You should not use various folk remedies to treat the disease, only special medications. If the patient still managed to survive after this pathology and was transferred to further outpatient treatment, then in these cases the following recommendations must be followed:
- Be sure to drink a lot and eat well.
- The room should always be in twilight.
- Taking vitamin complexes.
- Maintaining bed rest.
- Performing physiotherapeutic procedures.
Preventive measures
This pathology is considered dangerous and very scary, so you should protect yourself in advance from contracting this disease. In this case, it is worth remembering several important recommendations that will help avoid infection with amoebic meningoencephalitis:
- you should refrain from swimming in warm, stagnant bodies of water, especially with dirty water, which are not subject to sanitary control;
- It is better to protect your nose while diving - to do this, you can hold it with your hands or put a special clothespin on it;
- if you have to work in the garden or in a vegetable garden with wet soil, then you need to wear a mask and gloves on your hands;
- after working with wet soil, be sure to clean your hands and rinse them well; you also need to clean out all the dirt from under your nails;
- monitor children’s hygiene, do not allow them to pick their noses with dirty fingers;
- It is worth considering that amoeba cysts have increased vitality, so it is necessary to periodically clean air conditioner humidifiers;
- You should only drink boiled water.
Nose clips
Infection with amoebic meningoencephalitis can affect absolutely anyone. For this reason, it is important to follow preventive recommendations. These rules will help not only prevent infection, but also protect against unpleasant consequences that may arise from this pathology. Even if a person manages to be cured, he may still remain disabled for life. To prevent this from happening, you should carefully monitor where you swim in the summer, be sure to use protective equipment when working with the soil, as well as perform regular house cleaning and air conditioning cleaning.