When alcohol is consumed in reasonable doses, it is not a bad habit. It’s part of life, part of culture, entertainment, sometimes even a forced necessity (try not to drink at a corporate party after the CEO’s toast)! Unfortunately, sometimes alcohol is combined with taking some medications, and this can be dangerous.
In this article we will discuss whether alcohol is combined with one of the most used sleeping pills - Donormil.
Express test:
Assess how you feel during the day to determine the severity of your sleep problems
special instructions
You should be aware of the possibility of drug interactions:
- The effect of drugs is enhanced in combination with other sedatives (neuroleptics, barbiturates, etc.).
- Taken together with M-anticholinergics leads to side effects such as urinary retention, dry mouth, and thirst.
- Drinking alcohol during therapy leads to a pronounced increase in sedative effect, and the development of hallucinations is likely.
You should remember the need to count the sodium salts contained in the medicine (more than 400 mg in 1 tablet) for persons with limited salt intake. During therapy, work with moving mechanisms and work that requires increased mental concentration should be limited.
Use of the drug Donormil in the treatment of sleep disorders of moderate and mild severity
Smulevich A.B., Pavlova L.K., Zheleznova M.V.
The prevalence of sleep disorders is difficult to fully assess, since not all those suffering from it go to doctors, but try to cope with it on their own or with the help of traditional medicine. Some surveys estimate that up to 20% of middle-aged people in the population require examination for sleep disorders.
Sleep disorders can lead to temporary or long-term disability and are often the cause of non-standard and emergency situations, which determines their medical and social significance [2]. In the DSM-IV, insomnia is defined as a deficiency in the quality and quantity of sleep necessary for normal daytime activities, and in the ICD-10, insomnia, hypersomnia and sleep rhythm disturbances collectively mean “primarily psychogenic conditions with an emotionally caused disturbance in the quality, duration or rating questionnaire subjective characteristics of sleep”, which took into account such indicators as time of falling asleep, duration of sleep, number of night awakenings and dreams, quality of sleep and morning awakening. The questionnaire was filled out twice - before the start of treatment with Donormil and on the 15th day of therapy. The criterion for the effectiveness of the drug was considered to be an increase in the sum of points on all points of the questionnaire to at least 24 points at the end of therapy in the patient’s subjective assessment;
Patients had complaints of sleep disturbances even before the start of treatment; their duration varied from 3 months to 3 years (on average - 9.5±6 months). The majority used all kinds of means to treat insomnia (from herbal and physiotherapy to hypnotics), but assessed the treatment as insufficiently successful (lack of the expected effect, post-somnia disorders).
The number of “bad nights” per week over the past 3 months averaged 5.62±1.48. At the same time, 31 patients had a history of spontaneous sleep disturbances, and 11 had situationally determined ones (upcoming exams, anxiety for loved ones, work conflicts, etc.).
The drug was prescribed in doses from 7.5 to 30 mg in tablet or soluble form over 30 minutes. before going to bed for 15 calendar days. If there was no effect within 5 days, the course of treatment was stopped. Donormil was not prescribed simultaneously with tranquilizers; the evening intake of other drugs was postponed to 18.00.
Research results
The main results of the study make it possible to evaluate the effect of Donormil on sleep disorders of various origins.
42 of 61 (68.8%) patients completed the study. The positive effect of therapy recorded in this part of the patients allowed them to be classified as responders.
When analyzing the psychopathological manifestations that determine the symptoms of insomnia in this part of the observations, it turned out that the structure of the syndrome that dominates the clinical picture among responders is heterogeneous. In most cases, we are talking about depressive (53.1%) and anxiety-phobic syndromes (4.3%), but there have been cases of reduction of symptoms of insomnia that developed within the framework of hypochondriacal (17.6%) and astheno-apathetic (25%) disorders respectively.
The data presented in Table 1 also show that patients classified as responders, not only according to syndromic characteristics, but also in nosological assessment, belong to different categories. According to this criterion, respondents are distributed as follows: personality disorders (PD) - 52.4%, low-progressive (psychopathic-like) schizophrenia - 28.6%, cyclothymia - 19%.
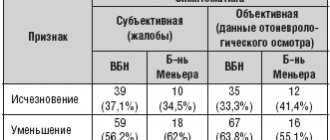
Let us now consider the data on the effectiveness of the studied drug, which, as established during the study, in the case of a positive response to therapy, affects the following sleep parameters.
Acceleration of falling asleep was recorded in the majority (31 out of 42 - 73.8%) of patients, and in this parameter the differences obtained during therapy compared with the initial ones were statistically significant (p < 0.05).
Although all other differences become significant (p<0.05) only in the summary assessment, it is found that Donormil improves the quality of sleep, increases its depth and reduces the number of dreams. Moreover, even in cases of nightmares, the majority of these patients (9 out of 14) stopped complaining of painful dreams.
Donormil also improves the quality of morning awakening: patients noted that they woke up rested, alert, and did not experience drowsiness, fatigue, or the desire to lie in bed.
However, as the data obtained indicate, the drug has virtually no effect on the number of night awakenings (out of 12 patients, only 2 noted a decrease in the frequency of night awakenings and 1 patient stopped expressing this complaint).
To the assessment of the effectiveness of Donormil already outlined above, it should be added that the drug has a favorable tolerability and safety profile. Adverse events recorded in 9 patients (21.4% of the total number of responders) were limited to complaints from 3 inpatients about short-term (no more than 30 minutes) morning lethargy and drowsiness, and outpatients (6 observations) additionally reported difficulties in inclusion in work activity. These effects are reduced during the first 5 days of taking the drug alone or by reducing the dose to 7.5 mg.
To try to answer the question of what parameters the ineffectiveness of Donormil correlates with, let us compare the already discussed calculations obtained for responders with statistical indicators for non-responders.
Let us immediately emphasize that the answer to the question posed is not limited to formalized characteristics and cannot be obtained without assessing clinical data.
And, indeed, when compared using formalized characteristics, it turns out that for most of the parameters identified in the tables under discussion, there are no statistically significant differences between responders and non-responders (19 observations). The exception is hypochondriacal syndrome, which is prevalent (albeit at the level of a statistical trend) among non-responders.
This statistical situation correlates with the clinical concept of hypochondria (primarily “sleep hypochondria” - Schlafhypohondie [13], identified in half of non-responders, whose condition during syndromic qualification was determined within the hypochondriacal syndrome), as a pathology resistant to therapy. If we take into account that in these cases we are talking not so much about sleep disorders, but rather about a paranoid struggle to restore its “ideal” quality within the framework of hypochondriacal schizophrenia, which occurs with aggravation of the signs of the defect, then the phenomena of therapeutic resistance will be deduced from the severity of the condition, determined by both for syndromic and nosological classification of the disorder.
The comparatively more pronounced degree of severity of depression in non-responders (despite the absence of statistically significant differences) is evidenced as formalized (on the Hamilton scale, the severity of depression was in 8 of 9 of these cases at least 24.8 ± 3 points versus 14.2 ± 3.6 in responders) and clinical data. Depression in these cases (diagnosed in 5 cases) is characterized by the dominance of signs of negative affectivity with the phenomena of alienation of the feeling of sleep. Detecting an affinity for negative disorders, the latter become chronic, prone to relapse, and resistant to therapy [9]. Insomnia in these cases is one of the anesthetic phenomena in the structure of negative affectivity, and accordingly one cannot expect a complete reduction of the disorder during therapy.
And finally, the data obtained allow us to assert that within the limits of insomnia itself in non-responders (despite the fact that in these cases no statistical or clinical differences from responders were identified), therapeutically resistant phenomena include intrasomnic disorders with frequent awakenings and difficulties in subsequent falling asleep . The use of Donormil for 5 days in these cases, as in other non-responders, is not accompanied by a reduction in sleep disturbances.
In conclusion, it is necessary to emphasize the following. The use of Donormil is effective for sleep disorders of moderate and mild severity that develop as part of personality disorders, affective pathology of the cyclothymic level or low-progressive (psychopathic-like) schizophrenia. Treatment of sleep disorders with Donormil is not accompanied by any adverse events or aftereffects.
Taking into account the data obtained in this study on the high effectiveness and safety of the drug Donormil, it can be recommended to a wide range of patients with sleep disorders that develop as a result of the pathology of the “minor” psychiatry.
Literature
1. Adamenko R.Ya. Treatment of insomnia in patients with chronic cerebrovascular insufficiency. Journal of a practical doctor No. 5, 2001, Kyiv.
2. Aleksandrovsky Yu.A., Avedisova A.S., Pavlova M.S., Gorinov A.A. Modern psychopharmacotherapy of psychogenic sleep disorders. A manual for doctors. - M.: Ministry of Health of the Russian Federation, 1998. - 24 p.
3. Vein A.M. Sleep disorders, main pathogenetic mechanisms, methods of correction. 1995. p. 6-12.
4. Vein A.M. Report on a study of Donormil in patients with insomnia. M. Center for Somnological Research, 1997, p.7.
5. Gorkov V.A., Rayushkin V.A., Churilin Yu.Yu. Pharmacological hypnotics: history and comparison. New medical technologies. - 2001; 6:39-40
6. Kolyadenko V.G., Purishkina O.P. Zastosuvannya Donormilu in complex Tepanii dermatological diseases. Faces of Ukraine.1998, No. 3, p. 38.
7. Levin Ya.I., Kovrov G.V. Some modern approaches to the treatment of insomnia. Magazine "Attending Physician", No. 04, 2003 // Open Systems Publishing House
8. Chekman I.S. Biochemical pharmacodynamics. K. Health, 1991. 201 p.
9. Smulevich A.B. Depression and comorbid disorders, 1997. 307 p.
10. Balogh A. Drug for the treatment of sleep disorders-review. Z Arztl Fortbild Qualitatssich. 2001 Jan;95(1):11-6.
11. Hausser-Hauw C., Fleury B., Scheck F., Pello JY, Lebeau B. Effet sur l'architecture du sommeil et effet residue d'une price de 15 mg de doxylamine chez le volontaire sain. Sem. Hop. Paris, 7-14 September, 1995.
12. Ermanni R., Ganzoni E. Doxylaminsuccinat bei Schlafst?rungen. Ars. Medici Nr. 4/90.
13. Peters U., W?rterbuch der Psychatrie und medizinischen Psychologie. M?nchen, 1971.
14. Schadeck B., Chelly M. et al. Efficacite comparative de la doxylamine (15 mg) et du zolpidem (10 mg) dans le traitement de l'insomnie commune. Une etude controlee versus placebo. Sem. Hop. Paris, 18-25 April, 1996.
Patient reviews
Sometimes people feel the negative effects of taking alcohol and Donormil together immediately, the very next morning. Sometimes it’s the other way around: they even like the enhanced effect and don’t experience any discomfort. It all depends on the characteristics of the body!
Rate this review:
Yesterday I returned from my birthday. Naturally, alcohol, emotions, all that... I couldn’t fall asleep right away and therefore took Donormil. How bad I felt this morning! My head was spinning and I felt nauseous. I couldn’t go to work in this state. By evening it had barely passed.
And one more:
Donormil is a good thing, but slow! A friend advised adding 50g of cognac to the sleeping pills. Full compatibility! I like it.
No matter how you react to such a “mixture” here and now, remember one thing: if you regularly combine sleeping pills with alcohol, there will definitely be consequences. It's better not to allow this to happen. Ask any doctor, he will confirm this.