The parietal lobe of the human brain occupies a fairly large part of the brain and consists of the inferior parietal lobule, superior parietal lobule and posterior central gyrus. Neoplasms in the parietal lobe of the brain pose a great danger to the patient, not only due to the disorders they cause, but also due to symptoms and subsequent death without adequate treatment.
Treatment of tumors in the parietal lobe of the brain in clinics in Germany, Israel, Austria, the USA and Switzerland is aimed at stopping the development of the tumor, as well as eliminating the general symptoms of the disease as much as possible.
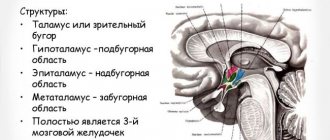
General information about the parietal lobe
The parietal lobe is a part of the cerebral hemisphere that is located behind the central sulcus.
The posterior border runs along the parieto-occipital sulcus and borders the occipital lobe. On the sides, the parietal lobe is limited by the Sylvian fissure. This structure of the cerebral hemisphere has the following main grooves:
- postcentral, which in turn is divided into upper and lower;
- interparietal.
The intersection of these grooves is called the helix, or star.
In the anterior part is the postcentral gyrus. The other two gyri are the superior parietal and inferior parietal, which are located horizontally.
Causes and risk factors
Cancer and benign dysplasia can form in the brain at any age, but the likelihood of developing pathology increases as you get older. The overall peak incidence occurs in the seventh decade. The tumor process develops more often in men than in women.
The main causes of brain glioma are the following:
- exposure to ionizing radiation (radiation is the main risk factor);
- genetic prerequisites due to heredity;
- damage by oncogenic viruses;
- head and cervical brain injuries;
- bad habits.
Important. There is no specific prevention against brain cancer. Minimizing risk factors, a healthy lifestyle, quality nutrition, regular exercise and a calm emotional background reduces the likelihood of developing a tumor process.
What fields are included?
In total, the parietal lobe of the brain has nine fields.
The first three fields, which are 1, 2 and 3, are primary sensorimotor fields. They are located in the vertical gyrus of the parietal lobe (postcentral). The fourth field is the primary motor cortex. Areas 5 and 6 are secondary somatosensory and motor areas, respectively. The seventh field, which is located in the upper part of the parietal lobe, is the tertiary motor cortex. Field 39, in turn, is responsible for analyzing written speech. The main function of field 40 is reading comprehension, as well as ensuring the reading process. This part of the brain is characterized by the presence of the following centers:
- - responsible for recognizing the position of the body and individual organs in space;
- sensitivity center – analyzes information about any changes in the environment;
- center of praxia – responsible for performing complex actions;
- vocabulary center – helps in recognizing letters and other signs;
- calculus center - responsible for carrying out numerical calculations in the mind.
Symptoms of a parietal lobe tumor
Early focal symptoms of temporal tumors are the following:
- disorders of superficial and deep sensitivity (contralateral hemianesthesia or loss of sensitivity on the opposite side of the body);
- astereognosis (loss of the ability to recognize familiar objects by touch with closed eyes; Greek a - prefix of negation; stereos - solid, spatial);
- autometamorphopsia, or disturbances in the body diagram - the patient’s own body or its individual parts are perceived as changed in size, deformed (Greek autos - himself; meta - after; morphe - form; opsis - vision). Disorders of the body diagram often occur when the posterior parts of the superior and middle parietal gyri are damaged. If the parietal-occipital cortex is damaged, allometamorphopsia (Greek allos - different, different) can occur - a violation of the perception of spatial characteristics of objects in the external world - they are seen enlarged, reduced in size, ugly.
When the neurons of the superior and middle parietal gyri are stimulated, somatic hallucinations occur when the body or part of it is perceived by the patient as a completely different object (dot, cloud, paragraph, snake, mechanical device, etc.).
The multifaceted functional role of the parietal lobes of the brain when they are damaged is manifested by a number of other disorders.
When neurons in the posterior central gyrus are stimulated, phenomena of sensory hyperesthesia (hypersensitivity) and various imaginary sensations on the opposite side of the body may occur. This, for example, is a pain syndrome that is not associated with any local pathology. Probably, these are also senestopathy - extremely painful and pretentious pathological sensations with their unusual localization (Latin sensus - sensation, feeling; pathos - illness, suffering). For example, a 10-year-old boy complains of the sensation of hot wires under his scalp.
When the cortex of the superior and middle parietal gyri is damaged in the area adjacent to the posterior central gyrus, autotopagnosia occurs - loss of the ability to recognize parts of one's own body. For example, with his eyes closed, the patient cannot show where his arm, leg or head are located, what position they are in, or what movements they are performing.
With a tumor of the parietal-frontal cortex of the dominant hemisphere, spatial hemiagnosia (Greek hemy - half; gnosis - knowledge) is observed - loss of the ability to distinguish between the left and right halves of space. For example, it is not determined on which side the source of sound or pain is located. Such a patient can only read text on the right side of the page and copy only the right side of the image. Being paralyzed, he is not aware of the fact of paralysis on the left side of the body - the Anton-Babinsky symptom. In hemisomatognosia, an even more serious disorder, the ability to simultaneously recognize the fact of left-sided paralysis, central blindness and central deafness is lost.
When the damage is localized in the area of the parieto-occipital cortex of the subdominant hemisphere, visual-spatial agnosia develops - loss of the ability to form a location plan, estimate the distance between objects, difficulties arise in recognizing the time from a dial, and difficulties arise in working with contour maps. In relatively mild cases of the disorder, the patient cannot learn to navigate in an unfamiliar area; in more severe cases, he gets lost even in familiar places, for example, he is unable to find a kitchen or toilet in his apartment.
Thus, in Alzheimer's disease, due to the parieto-occipital atrophic process, the ability to navigate in well-known places is lost, which is why patients cannot find their way back home, forget the entry point to a long-known store, or wander in search of a relative's house located nearby.
With allesthesia (Greek allos – different, other; aesthesis – sensation, feeling), the localization of stimuli in the external world and/or in one’s own body is disrupted. Thus, an object located in front is perceived as being located behind, behind the back. The localization of bodily sensations, in particular those associated with emotions, is disrupted. Thus, mental pain during depression is localized not in the heart, as patients with vital depression usually show, but in the groin, hip or lower back - Minor's symptom.
Irritation of neurons in the posterior central gyrus and adjacent areas of the parietal cortex can result in the appearance of a variety of hallucinations: tactile, kinesthetic, temperature, vibration, visceral, pressure and weight hallucinations. All these types of sensitivity, as well as sensitivity to pain, are found to be represented in the parietal cortex. In addition, irritation of the posterior gyrus cortex forms the clinical picture of Jackson's sensory epileptic seizures. During such attacks, various sensory disturbances occur, in particular paresthesia, pain or a feeling of numbness on the other side of the body in accordance with the topic of excited neurons.
When the cortex of the right parietal-occipital region (in right-handed people) is damaged, agnosia for faces and their images occurs - prosopagnosia (Greek prosopon - face). At the same time, the patient can recognize a person by his voice, smell or clothing.
Bilateral damage to the cortex of the inferior parietal lobe and occipital cortex leads to the development of gaze paralysis (the term is not entirely accurate), or Balint's symptom - the loss of the ability to perceive the connection between several simultaneously and visually presented stimuli: the patient usually perceives only one fragment of the whole, without being able to combine all its constituent fragments into a complete and recognizable image of the object. For example, if he is presented with a cross, then he sees both lines that make it up separately from each other, but cannot connect them or show the point of intersection. On the clock he sees the dial and hands isolated from each other, which is why he is not able to find out the time of day from the clock. He sees the glasses, but perceives their constituent elements separately from each other. According to other data, Balint's symptom occurs with right-sided damage to the parietal cortex in right-handed people. There is also a parietal variant of agnosia, in which the ability to associate impressions in the order of time of their occurrence is lost, therefore, when reporting certain events, the patient confuses their sequence.
The development of apraxia, i.e., the loss of automated skills and abilities, is associated with right-sided damage to the parieto-occipital cortex (in right-handed people). This, for example, is the loss of the ability to dress, shave, tidy up your hair, use a spoon, fork, or toothbrush. At the same time, motor function and muscle tone are not impaired. The development of kinesthetic apraxia is explained by damage to the areas of the parietal cortex immediately adjacent to the posterior central gyrus. It is assumed that kinesthetic apraxia occurs due to a lack of information from muscles, ligaments and joints, which leads to movement disorders in the corresponding part of the body on the affected side - the latter become uncertain, inaccurate, incomplete. Motor acts of a high degree of complexity are especially affected.
Damage to the cortex of the inferior parietal gyrus of the dominant hemisphere is manifested by alexia - loss of the ability to read, loss of the skill to recognize and combine writing signs into meaningful sentences (Greek a - prefix of negation; lexis - word, expression). With literal alexia, memory for the meaning of letters is lost, with asyllabia - syllables, with verbal alexia - words (Greek litera - letter; syllabe - syllable; verbum - word). Alexia in combination with agraphia is most often associated with damage to the cortex of the posterior part of the angular gyrus of the parietal lobe of the dominant hemisphere, when recognition of graphemes (Greek graphe - outline), especially similar in their spelling, suffers.
Loss of the ability to count, or acalculia, occurs when the posterior cortex of the inferior parietal gyrus of the dominant hemisphere is damaged. The patient, who is quite literate, is deprived of the ability to count objects, add, subtract, divide and multiply. Sometimes only one arithmetic operation appears.
Return to Contents
What is he responsible for?
The main function of this brain structure is to analyze information about space.
It is thanks to the parietal lobe that a person can determine the position of body parts and other objects, sizes, and proportions.
In addition, it is responsible for the analysis of oral and written speech, the perception of texts, verbal memory, as well as gaze control.
There are centers where analyzers are located that are responsible for the sensitivity of the skin, limbs and head. Thanks to this, a person can feel pressure on these organs, any changes in the temperature of the external environment, a feeling of goosebumps.
At the bottom of this brain structure are the praxis centers. Their main role is for a person to perform certain actions that are purposeful. This may include eating, running, dressing, and other activities.
Diagnostics
After an oral conversation and a physical examination (coordination, mental state, work of analyzers and other external signs are studied), the patient is examined using:
- tomography (CT, MRI, PET);
- ultrasound diagnostic methods (echoencephalography);
- EEG (electroencephalogram);
- angiography of cerebral vessels;
- ophthalmological examination;
- scintigraphy and others.
The most reliable method is biopsy (tissue collection is performed when cancer is removed or stereotactic biopsy). Histological analysis of tissue samples gives a complete picture of the type of neoplasm and all its features.
Organic brain damage
Symptoms of organic brain damage in children
The main sign of organic brain damage in children is psychoorganic syndrome. This condition is expressed in a violation of three aspects of brain function at once.
- Problems with memory - the child does not remember new information well and loses some of what has already been learned (partial amnesia). Moreover, with OPM, unreal (invented) memories may appear.
- Decreased intelligence - such children have difficulty concentrating, their thinking is impaired, and they have difficulty oriented in space.
- Affective disorders and reduced neurodynamics - children with organic brain lesions constantly experience weakness, dizziness and headaches, they are susceptible to depression and irritability. Children often display inappropriate emotions and “out-of-control” behavior.
- Delayed speech and intellectual development is another symptom of organic brain damage, which is characterized by impaired cognitive activity. This condition is not congenital, like mental retardation, but acquired. The functions of a child's damaged brain begin to disintegrate. Sometimes the developmental delay is so severe that the child cannot learn to care for himself.
There are also a number of focal symptoms , which depend on the area of the brain in which the disorders are localized.
Frontal lobe – facial and ocular muscles are paralyzed, the sense of smell is impaired and words are difficult to pronounce, difficulty performing purposeful movements, strange behavior on the verge of euphoria.
The parietal lobe is a violation of sensitivity, the inability to perform purposeful, meaningful actions, as well as the inability to learn reading and counting. Seizures with convulsions are common.
Temporal lobe - impaired sense of smell and hearing, problems with taste, there are hallucinations, emotionally unstable mood, partial or complete misunderstanding of speech.
Occipital lobe – visual impairment up to blindness, problems with coordination of movements and balance, hallucinations, convulsions during seizures.
Naturally, therapy and correction of APM should be prescribed based on the cause of its occurrence and development. For example, doctors recommend eliminating lesions caused by infection with the help of antibiotics, antiviral drugs and immunostimulants. If APM has developed as a result of a tumor, then, first of all, care must be taken to remove it. You can't argue with that.
Official medicine suggests treating ischemic diseases of the brain with nootropic drugs , as well as using decongestant and vascular therapy.
It is imperative to remember that drug therapy cannot but have side, sometimes harmful, consequences .
Eliminating the consequences is often more difficult and longer than the main violation.
But even in the case of successful drug therapy, you CANNOT do without psychological and correctional therapy.
If your child:
- very picky and capricious in choosing food
- reacts sharply to weather changes
- he gets carsick
- he's inattentive
- speaks poorly
- restless
- cries often
- clumsy
- lazy
Do you think that all these are character traits? In fact, these are neurological problems that may be associated with organic brain damage. If these violations are ignored now, then in the future they can cause serious behavioral disorders, speech delays and general development, and subsequently difficulties in learning at school.
The fact is that at an early age the consequences of many neurological disorders can be easily corrected and forgotten about them forever. But in adolescence, small problems often turn into big ones and are already very difficult to cope with.
Therefore, it is better not to postpone a visit to a neurologist and neuropsychologist.
It is especially important to conduct neuropsychological diagnostics in children before entering grade 1, to identify and correct neuropsychological disorders in a timely manner so that children do not develop “school failure”, which will affect not only the learning process, but also the psychological state of the child.
For example, in the temporal lobe of the left hemisphere there are areas “responsible” for the sound analysis of speech. If neuropsychological tests that check the state of this area of the brain are performed incorrectly, it is possible not only to diagnose its immaturity, but also to predict the occurrence of certain types of errors in speaking, writing, reading and remembering information.
Treatment methods
The treatment tactics for intracerebral formations are selected by a neurosurgeon or neurologist after a comprehensive examination. It includes the appointment of the following studies:
- EEG, Echo-EG;
- determination of visual acuity;
- ophthalmoscopy;
- perimetry;
- MRI and CT of the brain.
The main diagnostic method is magnetic resonance imaging. With its help, you can identify the exact location of the tumor and differentiate the tumor from an intracerebral hematoma, abscess or cyst.
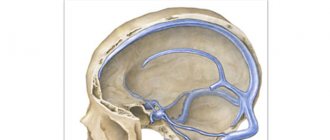
Removal of the brain mass is the main treatment method. When a pathological lesion grows into the brain tissue, shunt operations are used, which ensure the outflow of cerebrospinal fluid and the installation of modern drainage systems. Additionally, specialists use radiation therapy. With its help, you can influence the pathological formation from different positions, while preserving healthy cells. This slows down further growth of the tumor and reduces the main clinical manifestations.
Surgical treatment can be combined with radiation therapy, as well as chemotherapy. But the main method of combating the disease is surgery. Precision neurosurgical operations make it possible to completely or partially remove brain tumors, relieve the patient from severe clinical manifestations of pathology and improve the future prognosis.