Glioma is a brain tumor that originates from neuroglial cells. Neoplasms are the most common type of malignant pathogenesis of varying degrees of aggressiveness. Symptoms of glioma in adults and children will depend on where it forms. The main diagnostic methods are CT and MRI; the most accurate result is obtained by cytohistological analysis of the selected material (biopsy). The main treatment method for brain glioma is surgical removal of the pathological tumor. Treatment is always comprehensive; in addition to surgery, chemotherapy and radiotherapy are prescribed. Recovery and life expectancy after tumor removal depend on many factors: the adequacy of treatment, the degree of malignancy of the brain tumor, the stage of the disease, the general condition of the patient and many other factors. Benign gliomas have the best prognosis, while grade 3 and 4 gliomas have the worst prognosis. For example, with glioblastoma, life expectancy is usually no more than two years.
Origin of brain gliomas and characteristics
There is still no consensus on which cells give rise to glial tumors. The classical view is based on the fact that gliomas develop from mature glial cells (oligodendrocytes and astrocytes). Recently, they have become more inclined to believe that they are formed in the so-called “malignancy gaps.” This means that brain tumors of this type are formed from immature, slowly proliferating cells that gradually become malignant (degenerate into cancer). How exactly the neoplasm will develop depends on transformations in the genome, for example, astrocytomas (a type of glioma) are formed due to mutations in the TP53 gene,
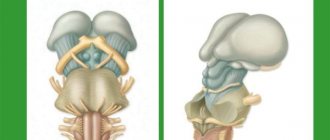
The share of gliomas in the general population of brain tumors is about 60%. Most often, neoplasms form in the brain and are primary in nature. Brain stem glioma is diagnosed relatively rarely. The color of neoplasia ranges from dark red to soft pink, the shape in most cases resembles a circle or spindle, but can also have irregular outlines. The size depends on the stage of the disease: from a few millimeters to 10-14 cm.
The most common location of the tumor is the area of the chiasmata or cerebral ventricles. Benign glioma, as a rule, does not spread to the bone structures of the skull and does not grow into the membranes of the brain, however, this cannot be excluded. Malignant glioma grows slowly at first, but as carcinogenesis progresses, its growth accelerates. Infiltrative growth is characteristic, i.e. the ability to grow into neighboring tissues, which during diagnosis does not allow defining clear boundaries of the pathogenic focus.
Note. Brain gliomas are not characterized by metastasis, however, they lead to degeneration of neighboring tissues.
Causes
Today, the mutation theory of carcinogenesis is relevant. It is based on the doctrine that brain tumors, like other neoplasms, develop as a result of mutations in the cell genome. The tumor is of monoclonal origin - the disease initially develops from a single cell.
Other theories:
- Viral. This theory suggests that the tumor develops due to exposure to oncogenic viruses: Epstein-Barr, herpes type six, papillomavirus, retrovirus and hepatitis viruses. Pathogenesis of an oncogenic virus: the infection penetrates the cell and changes its genetic apparatus, as a result of which the neuron begins to mature and work along a pathological path.
- Physico-chemical theory. There are artificial and natural sources of energy and radiation in the environment. For example, gamma radiation or x-rays. Irradiation with them in large doses leads to the transformation of a normal cell into a tumor-like one.
- Dishormonal theory. A hormonal imbalance can lead to mutation of the cell's genetic apparatus.
Causes and risk factors
Cancer and benign dysplasia can form in the brain at any age, but the likelihood of developing pathology increases as you get older. The overall peak incidence occurs in the seventh decade. The tumor process develops more often in men than in women.
The main causes of brain glioma are the following:
- exposure to ionizing radiation (radiation is the main risk factor);
- genetic prerequisites due to heredity;
- damage by oncogenic viruses;
- head and cervical brain injuries;
- bad habits.
Important. There is no specific prevention against brain cancer. Minimizing risk factors, a healthy lifestyle, quality nutrition, regular exercise and a calm emotional background reduces the likelihood of developing a tumor process.
Reasons for the ineffectiveness of chemotherapy and radiation treatment using outdated methods
Due to the special organization and functions of the central nervous system, the effectiveness of irradiation of a brain tumor using traditional radiotherapy installations was extremely low, as was the benefit from taking previous generation chemotherapy drugs. This happened because:
- radiotherapists could not use high enough doses of ionizing radiation, since it destroyed not only the tumor, but also healthy brain tissue located in the path of the radiation flow;
- Chemotherapists had practically no drugs at their disposal that had the ability to penetrate the blood-brain barrier, act selectively and not cause significant harm.
With the advent of new technologies, equipment and drugs in the arsenal of neuro-oncologists, the situation has changed dramatically.
Classification
Depending on the type of brain cells that degenerated and gave rise to pathogenesis, the following types of tumors are distinguished:
- astrocytomas are the most common type, their share in the general population is about 50%;
- oligodendrogliomas – the share in the general population of tumors of this type is up to 10%;
- Ependymomas are the rarest forms (occurrence less than 7%).
According to the WHO classification (which is generally accepted), neoplasia is ranked depending on the degree of malignancy.
Benign gliomas
These are tumors of the first degree of malignancy, for example, astrocytomas: giant cell, pilocytic, juvenile subependymal. They are benign because they grow slowly, have no signs of cancer, and are easy to treat. The prognosis for life with benign glioma is favorable. After tumor removal, patients live 10 years or longer.
Low grade glioma
Second degree of malignancy. It is also classified as a benign neoplasm, but with a borderline degree of malignancy. The growth of pathological tissue is slow (low-grade), they are well differentiated, as a rule, there is only one sign of cancer (cell atypia). Tumors of this type can degenerate into cancer and easily progress to the third and fourth degree of malignancy. These include diffuse and fibrillary astrocytomas. Treatment is complex: surgery to remove atypical tissues, additionally radio and chemotherapy.
Malignant gliomas
These include gliomas of grade 3 and 4:
- Third degree of malignancy . There are all signs of malignancy, except for tissue necrosis. Tissues lose clear differentiation, tumor growth accelerates (high-grade), the boundaries are unclear, and growth into nearby tissues is typical. The most striking example is anaplastic astrocytoma, which most often develops in middle-aged and older people. Treatment is hampered by the lack of clear boundaries of the tumor; life expectancy depends on how much atypical tissue is removed, as well as the stage of carcinogenesis at the beginning of treatment.
- The most dangerous is the fourth degree of malignancy (glioblastoma). It develops between the ages of 40 and 70 years. In this case, all the signs of malignancy are present, including necrosis. The tumor grows quickly, penetrates other tissues and has no clear boundaries. This significantly complicates therapy. The prognosis is unfavorable.
Neoplasia is divided into two types, depending on growth characteristics:
- Tumors of nodular growth . As a rule, these are benign neoplasms with clear contours. They are characterized by formation anywhere in the brain and the presence of cysts. Examples: pleomorphic xanthoastrocytoma and piloid astrocytoma.
- Diffuse type formations . There are no obvious boundaries, the size can reach significant sizes, neoplasia grows into adjacent brain tissue, which complicates the removal of dysplasia. These are often malignant tumors, such as glioblastoma or anaplastic astrocytoma, or those that can quickly degenerate.
Malignant and benign gliomas
Neoplasms can be benign or malignant. The exact type of tumor is determined by a neurologist or neurosurgeon based on the diagnostic data.
Experts distinguish three main types:
- astrocytomas;
- ependymocytes;
- oligodendrogliocytes.
Depending on the degree of malignancy, tumors come in several types. Juvenile and giant cell astrocytomas are considered benign. They are classified as the first degree and are considered the most harmless. Glioma of the second stage is borderline. It is growing slowly and has a favorable prognosis. But without timely treatment, it easily transforms into a tumor of the third and fourth degrees of malignancy.
Symptoms
Clinical manifestations are divided into general and focal. The latter manifest themselves depending on which part of the brain the pathological formation is formed.
General symptoms
General signs of brain cancer (or a benign tumor) arise due to increased pressure inside the skull, compression of neighboring tissues by the tumor body and the negative influence of its metabolites. Common symptoms include:
- dizziness, headache, discomfort in the head;
- dyspeptic manifestations not related to food intake or poisoning;
- loss of appetite, weight loss;
- blurred vision;
- changing the psycho-emotional behavior habitual for a person;
- memory problems, weakening of mental activity;
- signs of epilepsy.
It's important to understand. That general symptoms are not specific. If they bother you regularly, you need to urgently visit a doctor.
The pathological process in the early stages, as a rule, occurs latently or its signs are weak. Often neoplasms are found by chance, when examining a patient for another disease or for preventive purposes.
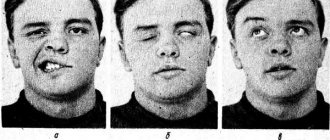
Focal symptoms
These are specific signs that arise as a result of damage to the cerebral structures of the central nervous system. The clinical picture depends on the location of the pathological focus:
- Glioma of the optic nerve is formed from cells of its trunk. Tissue growth is slow, accompanied by infiltration, but does not grow into the dura mater. The neoplasm is considered benign; it can form along the entire length of the nerve, but is more often located in the orbital part. Symptoms of optic nerve glioma: first, visual acuity decreases (as the nerve and elements of the eye are damaged), then bulging eyes develop.
- Diffuse glioma of the brainstem is highly malignant. Since diffuse dysplasia is formed in the area where the nerves responsible for the functioning of the limbs are located, when they are damaged, the coordination of the arms and legs is disrupted, up to paresis and paralysis. Clinical signs of diffuse pontine glioma are significant even with small sizes of dysplasia. There are many nerve cords passing through the bridge, so the clinic can be more diverse.
- Glioma of the frontal lobe of the brain is manifested by apathy, mental changes, the person becomes nervous, hot-tempered, and sudden mood changes are characteristic. The later stages of the disease are characterized by the onset of paralysis.
- Glioma of the temporal region causes impaired coordination of movements, memory deteriorates, and diction suffers. In addition, temporal lobe glioma negatively affects the sense of smell.
- Glioma of the cerebellum and cerebellar vermis leads to movement abnormalities. The gait is disturbed, it seems that the person is drunk. This is because it becomes difficult for the patient to maintain balance, his arms and legs do not obey, and maintaining the body in space becomes problematic.
- Glioma of the parietal lobe is accompanied by disturbances in fine motor skills, so a person’s handwriting changes, and over time it becomes difficult to write. Tactile sensations become dull.
- Glioma of the quadrigeminal plate or quadrigeminal plate causes visual disturbances, abnormalities in eye movement, and hearing impairment.
- Glioma of the corpus callosum is accompanied by visual hallucinations (the same ones occur in the presence of a tumor in the occipital lobe), violations of logic, as well as many other signs: changes in sensitivity, muscle weakness, and so on.
- Pontine glioma (diffuse or common) leads to disruption of conduction functions, since the nuclei of the cranial nerves are localized in this area. Therefore, the clinical picture will be quite broad. A violation of sensory perception, movements, and so on is recorded.
- Glioma of the cerebral ventricle leads to an increase in intracranial pressure due to disruption of the outflow of cerebrospinal fluid. Hydrocephalus may develop.
Tumor symptoms
Clinical manifestations are determined by the location of the tumor. The following groups can be distinguished: general cerebral and focal symptoms.
General cerebral symptoms are symptoms that occur when intracranial pressure increases.
- Headache is constant and has a high intensity headache. Poorly controlled by analgesics.
- Nausea and vomiting are associated with changes in intracranial pressure. Vomiting occurs due to the effect on the vomiting center and does not bring relief. Patients may become exhausted quickly due to loss of body fluids.
- Dizziness is caused by tumor growth, leading to deterioration of blood supply to the brain.
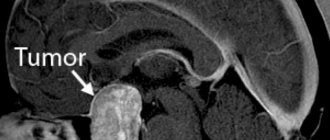
Diagnostics
After an oral conversation and a physical examination (coordination, mental state, work of analyzers and other external signs are studied), the patient is examined using:
- tomography (CT, MRI, PET);
- ultrasound diagnostic methods (echoencephalography);
- EEG (electroencephalogram);
- angiography of cerebral vessels;
- ophthalmological examination;
- scintigraphy and others.
The most reliable method is biopsy (tissue collection is performed when cancer is removed or stereotactic biopsy). Histological analysis of tissue samples gives a complete picture of the type of neoplasm and all its features.
Positron emission tomography (PET) for glioblastoma
Positron emission tomography is a useful adjunct in the detection of glioblastoma multiforme, especially after surgery to remove it. In this case, when performing CT and MRI, the distinction between residual or recurrent tumor and postoperative edema or scar is often difficult. The use of 18-fluorodeoxyglucose (FDG) PET is effective for tumors with high metabolic activity that actively take up glucose, whereas such FDG accumulation is not observed for postoperative edema or scar tissue. In cases where the tumor has been resected, the detection of increased FDG uptake in the surgical area is a reliable indicator of disease recurrence. However, after radiotherapy, increased activity can be observed in the surgical site without tumor recurrence. False-positive results are found after radiation therapy, when active granulation tissue can metabolize FDG, which can reduce the sensitivity of the method. An epileptogenic focus located adjacent to the surgical site may also show increased metabolism on PET, especially if epileptic activity is high. All of these options require assessment by an experienced neuroradiologist. If the initial evaluation of the images does not provide a clear answer, a second opinion on a PET scan may be helpful.
Treatment of brain glioma
Surgical removal of brain glioma is the main method of choice. Treatment is always complex. The results of the operation are supported by the administration of radiotherapy and chemotherapy (before and after the operation). As a rule, surgery to remove gliomas gives a good result only in the case of benign neoplasias that are at the first stage of pathogenesis. At this time, it is possible to completely remove the abnormal tissue.
In other cases this is difficult or impossible to do. Pathological tissues grow into neighboring ones, their boundaries are clearly indistinguishable, so the contour of the tumor cannot be identified, for example, in diffuse types of cancer. Regardless of the method of performing the operation: radical (trepanation or resection of the skull) or minimally invasive (stereotactic techniques and others), their meaning remains the same - it is important to try to remove all the pathological tissue (total removal) or most of it (subtotal).
More often, these tumors are detected at a progressive stage of development, which makes it impossible to perform total removal. In this case, radiotherapy becomes the main method of treatment, for example, this is how diffuse brainstem glioma is treated. Contraindications to surgery may be the presence of other types of cancer, the patient’s poor health or advanced age, the proximity of the cancer to vital structures, the growth of neoplasia in both hemispheres, or a location with difficult access.
Symptomatic treatment and rehabilitation
In addition to fighting a malignant tumor, it is important to relieve symptoms and ensure a satisfactory condition and quality of life for the patient. According to indications, glucocorticosteroids are prescribed to reduce cerebral edema and relieve headaches, dehydration therapy (aimed at reducing intracranial pressure and cerebral edema), anticonvulsant therapy, and anticoagulants.
Gliomas often disrupt the function of nerve centers responsible for speech and movement. In such cases, after completion of treatment, patients need rehabilitation measures: physical therapy, mechanotherapy, occupational therapy, classes with a speech therapist.
Recovery period and life prognosis
The recovery period after removal of a brain glioma will depend on many factors. The most important of them are: the quality of the tumor, its stages, the success of surgical treatment and the general condition of the patient. Generally speaking, the prognosis for life with glioma is unfavorable. With subtotal tumor removal, there is a high risk of relapse, so life expectancy after surgery for brain glioma with partial removal is low. Complete removal is possible at the first stage of a benign tumor. About 80% of patients live longer than five years, provided that the tumor of the first degree of malignancy is completely excised. With relapse of grade 3 or 4 glioma, the prognosis does not exceed two years.
Chemotherapy
Chemotherapy for gliomas is most often used in combination with radiation therapy. In most cases, treatment is carried out with the chemotherapy drug temozolomide (Temodar). It is available in tablet form. Sometimes other drugs are used. For example, a PCV regimen includes lomustine, vincristine, and procarbazine.
For high-grade gliomas, local chemotherapy is used. During the operation, the surgeon removes the tumor and implants in its place a special plate soaked in the drug carmustine (also known by the commercial name BCNU). It remains in the patient's body and continues to destroy remaining tumor cells. At the same time, it is possible to avoid side effects that occur with systemic administration of chemotherapy drugs. This treatment method has been used since 1995.
2.Symptoms of thalamic gliomas
At the beginning of the disease, the patient in most cases does not feel anything, and only in a later period, when the neoplasm becomes large enough, spreads beyond the thalamus and damages neighboring structures, certain symptoms arise:
- decreased skin sensitivity of half the body, impaired sensation of hot/cold;
- pain in half the body, aggravated in the cold - from mild to severe;
- movement disorder, deformation (twisting) of the hands and fingers;
- involuntary movements (hyperkinesia).
Visit our Neurosurgery page