Intercostal neuralgia is a disease in which irritation or compression of the intercostal nerves occurs. This can happen for various reasons. The disease is relatively rare, its main manifestation is pain along the affected nerve.
Our expert in this field:
Lashch Natalia Yurievna
Neurologist of the highest category, candidate of medical sciences, associate professor. Laureate of the Moscow City Prize in the field of medicine.
Call the doctor Reviews about the doctor
How are intercostal nerves arranged? What functions do they perform?
Two nerve roots emerge from the spinal cord: the anterior one is formed by the processes of motor nerve cells, the posterior one - by sensory ones. Then, while still inside the spinal canal of the spine, these roots are connected to form the spinal ganglion. Two spinal nerves depart from it: anterior and posterior.
In the thoracic spinal cord, the anterior branches of the spinal nerves pass into the intercostal nerves. They pass in the spaces between the ribs - each of them is located along the lower edge of the corresponding rib - and, unlike the anterior spinal roots, are mixed, that is, they are responsible for both movement and sensitivity:
- provide movement of the chest muscles involved in the breathing process;
- provide sensitivity to the skin of the chest and upper abdomen.
How does intervertebral neuralgia develop?
The human musculoskeletal system includes not only bone formations, but also surrounding structures - discs, blood vessels and nerve fibers.
The discs are made of fibrocartilaginous tissue and act as a durable shock absorber.
However, when exposed to negative factors, the disc fibrous ring is deformed and enters the intervertebral space, disrupting innervation and blood supply.
The result is intervertebral neuralgia, which significantly worsens the quality of life.
Treatment of intercostal neuralgia
How to treat intercostal neuralgia? Therapy is carried out in two directions:
- It is necessary to alleviate the main symptom of the disease - chest pain.
- At the same time, it is necessary to identify the cause - the disease that led to compression or irritation of the nerve - and treat it.
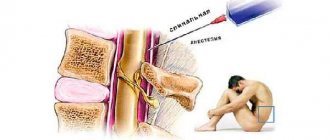
In the acute stage of the disease, the doctor prescribes bed rest and recommends sleeping on a flat and firm bed. To combat pain, non-steroidal anti-inflammatory drugs are used, and various ointments help. In case of severe pain, a novocaine blockade is performed: the place where the affected nerve is located is injected with an anesthetic solution. There are also special patches with anesthetics.
Vitamins are prescribed to improve the condition of nervous tissue, muscle relaxants to relieve muscle spasms. Prolonged pain leads to a person becoming overly excitable and nervous, in which case sedatives are prescribed. Physiotherapy procedures help: Sollux, electrophoresis, UHF. A neurologist can prescribe massage and acupuncture sessions.
Is it possible to cope with the disease on your own? Over-the-counter pain medications and folk remedies can help relieve pain for a while. But in order to prescribe truly effective treatment for intercostal neuralgia on the right or left, you need to understand what causes it. Improper self-medication can be harmful.
We will call you back
Message sent!
expect a call, we will contact you shortly
The main symptom of intercostal neuralgia is pain. It spreads along the rib, as if encircling the right or left half of the chest, and can be sharp, stabbing, burning, or dull, aching. The pain intensifies during inhalation, because of this the person cannot breathe deeply. Movements, changes in body position, coughing, and sneezing also lead to aggravation.
Painful sensations occur if you press on certain points between two adjacent ribs along their course. This symptom is checked by a neurologist during an examination.
Other possible symptoms of intercostal neuralgia on the right and left (as well as pain, occur in the area of the affected nerve):
- twitching of the chest muscles;
- increased sweating;
- redness or paleness of the skin;
- numbness.
With intercostal neuralgia on the left, a person may complain that his heart and stomach hurt. Pain may radiate under the shoulder blade, to the collarbone area.
Similar chest pains can occur with diseases of the heart, lungs, pleura, and spine. An incorrect diagnosis and lost time can lead to serious consequences.
Forms of the disease
Chest neuralgia can be primary (an independent pathology) and secondary (a symptom of another disease). There are also radicular and reflex forms of the disease. In the first case, symptoms of intercostal neuralgia on the left and right arise due to irritation of the spinal roots. The second type of pathology occurs due to a negative effect on peripheral receptors.
In addition, clinicians distinguish the following types of thoracic neuralgia:
- musculoskeletal;
- vertebrogenic;
- spicy;
- chronic;
- right-sided;
- left-handed;
- psychogenic;
- during pregnancy.
Intercostal neuralgia of a certain type has its own characteristic symptoms and treatment features.
How to distinguish the signs of intercostal neuralgia from the symptoms of other diseases?
It is especially important to distinguish in time between irritation of the intercostal nerves and angina pectoris, a condition in which the heart muscle does not receive enough oxygen-rich blood. Main differences:
- With intercostal neuralgia, pain persists for a long time. With angina pectoris, they last about 5 minutes and go away if you take nitroglycerin.
- With neuralgia, pain intensifies during deep inspiration, movements, sneezing and coughing, but with angina pectoris this does not happen.
Other dangerous conditions that need to be distinguished from intercostal neuralgia are myocardial infarction and PE ( pulmonary embolism) . Typically, a heart attack occurs after physical exertion or after a person becomes very nervous. The pain is accompanied by signs of dysfunction of the cardiovascular system:
- The man turns pale. Fingertips, nose, lips may become bluish.
- Sticky cold sweat appears.
- Shortness of breath that persists even when the person is resting - lying or sitting.
- Blood pressure drops.
- The fear of death arises.
You should not engage in self-diagnosis - erroneous conclusions are fraught with serious consequences. See your doctor. Get examined at the clinic. In any case where there is a suspicion of a heart attack, it is better to play it safe and immediately call an ambulance.
Symptoms
With neuritis, the nerve fiber is damaged, and therefore the functions suffer, the main ones being sensitive, motor and trophic, therefore the following symptoms are clinically noted:
- In the phase of irritation of the nerve fiber: pain, burning, feeling of “crawling goosebumps”, feeling “as if many needles are being pricked”.
- In the phase of loss of functions: decreased muscle strength, muscle atrophy, decreased reflexes, decreased sensitivity, tissue atrophy including skin, subcutaneous fat, muscles, bone tissue.
Treatment of symptoms of intercostal neuralgia on the right and left
The leading symptom of the disease – pain – is helped by painkillers (non-steroidal anti-inflammatory drugs), anesthetic patches, novocaine blockades, and physiotherapy.
But coping with the symptoms does not mean curing the disease. Therefore, treatment should also be aimed at the cause. A thorough diagnosis must first be carried out - this is only possible in a clinical setting.
Take care of yourself, book a consultation now
Message sent!
expect a call, we will contact you shortly
“Intercostal neuralgia” is not one specific diagnosis, but a collective term. It refers to different conditions that lead to damage to the intercostal nerves and, as a result, to chest pain.
Why is it important to understand the cause of this condition in each specific case? This will allow you to prescribe effective treatment that will help you recover or keep your chronic disease under control.
Possible complications and consequences
Any neuralgia, in particular intercostal neuralgia, that does not respond to treatment, may be a sign of a serious illness. Most of the complications that arise with thoracalgia are precisely a manifestation of the underlying pathology, which worsens against the background of constant pain.
Chest neuralgia itself, with a long-term severe course, can provoke the development of a hypertensive crisis or an attack of angina (less often, myocardial infarction). Severe, constant pain affects a person’s physical and mental state in different ways. Often severe symptoms of intercostal neuralgia on the left or right significantly complicate the patient’s life. He sleeps poorly, is nervous, cannot move normally and do his usual work.
Pain in the intercostal spaces does not allow the patient to perform full breathing movements, which leads to a decrease in oxygen supply to the body and the development of hypoxia. Sometimes neuralgia is accompanied by such debilitating pain that it contributes to emotional exhaustion, and this is a serious complication, since this condition causes depression.
The main causes of intercostal neuralgia
Most often, the following reasons lead to compression and irritation of the intercostal nerves:
- Osteochondrosis. A degenerative disease that primarily affects the intervertebral discs. Their height decreases - the distance between adjacent vertebrae decreases, this leads to compression of the nerve roots.
- Hypothermia, exposure to drafts.
- Intense physical activity, sudden awkward movements.
- Working in an awkward position when your back is constantly under tension.
- Injuries to the chest and thoracic spine, previous surgeries.
- Frequent and severe stress.
- Viral infections. The most common cause is a cold, shingles.
- Chronic spasm of the back muscles. It promotes irritation of nerve receptors.
Most often, intercostal neuralgia occurs in older people, when the causes of the disease are layered with age-related changes in the spine and blood vessels.
Causes of pathology
The reasons for the development of neuralgia can be different: inflammatory processes, injuries, bacteria and viruses, poisoning with drugs and various substances, autoimmune diseases, circulatory disorders in the vessels supplying the nerve.
- infections such as shingles, Lyme disease, or HIV
- pressure on bone nerves, blood vessels or tumors
- kidney disease or diabetes
- age
What other diseases lead to girdle pain in the chest?
Often people tend to dub “neuralgia” any girdle pain along the ribs. But this symptom may have other causes, including:
- Spondylosis is an inflammatory disease that causes damage to the vertebral bodies and deformation of the spinal column.
- Hormonal spondylopathy is a pathology that develops in older people, for example, in women after menopause. The spine is deformed, and disorders occur in the vessels that supply it.
- Malignant tumors - those that arise in the spine itself or metastases from other parts of the body.
- Ankylosing spondylitis is a chronic inflammatory process that leads to decreased mobility in the spinal column.
- Gastritis and other diseases of internal organs.
How does the treatment of intercostal neuralgia depend on the cause?
With intercostal neuralgia, it is not enough to eliminate the main symptom of the disease - pain. You should always look for and treat the underlying cause. The doctor prescribes therapy individually, depending on the pathological changes detected during examination and examination, and the final diagnosis.
Make an appointment at the Medica24 International Clinic - get a consultation with an experienced neurologist and undergo an examination using our modern equipment. This will help to quickly and accurately establish a diagnosis and prescribe the correct treatment in a timely manner.
Get a consultation with a doctor
Message sent!
expect a call, we will contact you shortly
The main manifestation of intercostal neuralgia – chest pain – can also occur with many other diseases. And figuring out the correct diagnosis is not always easy.
The diagnostic process begins with a visit to a neurologist. The doctor will ask you some questions:
- When did you first experience pain? How did this happen? What preceded this?
- What is the nature of the pain, when does it usually occur, how often, how long does it last?
- Do you have chronic lung or heart diseases? Are you monitoring your blood pressure?
- What infections have you had? Have you had any chest injuries or surgery?
- What other symptoms bother you?
You may be asked to complete a special “pain questionnaire”. The doctor will perform a complete neurological examination to rule out other neurological diseases. You will then be given an examination.
To understand the causes of irritation or compression of the intercostal nerve, the doctor may prescribe x-rays, CT, MRI, and, if necessary, other studies.
BACK PAIN: painful muscle spasms and its treatment with muscle relaxants
Back pain is one of the most common complaints that patients present in general medical practice. They are often caused by spinal osteochondrosis - a degenerative lesion of the intervertebral disc cartilage and reactive changes in the adjacent vertebral bodies. Damage to the intervertebral disc develops as a result of repeated injuries (heavy lifting, excessive static and dynamic load, falls, etc.) and age-related degenerative changes. The nucleus pulposus, the central part of the disc, dries out and partially loses its shock-absorbing function. The fibrous ring, located along the periphery of the disc, becomes thinner, cracks form in it, towards which the nucleus pulposus moves, forming a protrusion (prolapse), and if the fibrous ring ruptures, a hernia. Currently, drugs have been created that have a structure-modifying effect on cartilage tissue (the old name is chondroprotectors). A typical representative of the group is the drug chondro, prescribed in a course of 4 months (the effect lasts 2 months after discontinuation). In the affected spinal segment, relative instability of the spine occurs, osteophytes of the vertebral bodies develop (spondylosis), and ligaments and intervertebral joints are damaged (spondyloarthrosis). Herniated intervertebral discs are most often observed in the lower lumbar discs, less often in the lower cervical and upper lumbar discs, and extremely rarely in the thoracic discs. Disc herniations into the vertebral body (Schmorl's hernias) are not clinically significant; disc herniations in the posterior and posterolateral direction can cause compression of the spinal root (radiculopathy), spinal cord (myelopathy at the cervical level) or their vessels.
In addition to compression syndromes, reflex (muscular-tonic) syndromes are possible, which are caused by impulses from receptors in response to changes in the discs, ligaments and joints of the spine - painful muscle spasm. Reflex muscle tension initially has a protective nature, since it leads to immobilization of the affected segment, but later this factor becomes the cause of pain. Unlike compression syndromes of spinal osteochondrosis, which are relatively rare, painful muscle spasms occur during the life of almost every second person.
A classic example of a painful muscle spasm is lumbago (lumbago), which is characterized by a sharp, shooting pain in the lower back, usually developing during physical activity (lifting heavy objects, etc.) or awkward movement. The patient often freezes in an uncomfortable position, and an attempt to move leads to increased pain. The examination reveals tension in the back muscles, usually scoliosis, flattening of the lumbar lordosis or kyphosis.
Lumbodynia - back pain - and lumboischialgia - pain in the back and along the back of the leg - develop more often after physical activity, awkward movement or hypothermia, less often - without any reason. The pain is aching in nature and intensifies with movements in the spine, certain postures, and walking. Lumboischialgia is characterized by pain in the buttock, in the posterior parts of the leg, not reaching the toes. The examination reveals pain, tension in the muscles of the back and posterior group of leg muscles, limited mobility of the spine, often scoliosis, and symptoms of tension (Lasegue, Wasserman, etc.).
At the cervical level, reflex muscular-tonic syndromes may occur: cervicalgia and cervicobrachialgia, which often develop after physical activity or awkward neck movement. Cervicalgia is pain in the cervical region, which often spreads to the back of the head (cervicocranialgia). Cervicobrachialgia is pain in the cervical region spreading to the arm. Characteristically, the pain intensifies with movements in the neck or, conversely, with a prolonged static position (at the movies, after sleeping on a thick, high pillow, etc.). During the examination, tension in the cervical muscles is revealed, restriction of movements in the cervical spine, and pain on palpation of the spinous processes and intervertebral joints on the side of pain are often observed.
When a nerve root is compressed (radiculopathy), in addition to painful muscle spasms and limitations in mobility in the spine and limbs, sensory, reflex and (or) motor disturbances are detected in the area of the affected root. At the lumbar level, the fifth lumbar (L5) and first sacral (S1) roots are most often affected, less often - the fourth lumbar root and very rarely - the upper lumbar roots. Radiculopathies of the lower cervical roots are much less common.
Painful muscle spasm also occurs with another fairly common cause of pain in the back and limbs - myofascial pain caused by the formation of so-called trigger zones in the muscles and (or) associated fascia. Myofascial pain is manifested by muscle tension and the presence of trigger points in them, which are identified through manual examination of the muscles. An active trigger point is a constant source of pain that increases with palpation in the muscle; a latent trigger point causes pain only when palpated. For each muscle there is an independent myofascial syndrome with a characteristic localization of pain when the trigger zone is irritated, spreading beyond the projection of the muscle to the skin surface. There are no focal neurological disorders, except in cases where tense muscles compress the nerve trunk.
It is important to remember that back pain may be the only symptom of a spinal cord tumor, syringomyelia and other spinal cord diseases. Pain occurs with destruction of the vertebrae and damage to the nerve roots due to infectious processes (tuberculous spondylitis, spinal epidural abscess), neoplasms (primary and metastatic tumors of the spine, myeloma), dysmetabolic disorders (osteoporosis, hyperparathyroidism, Paget's disease). Back pain can be a consequence of a spinal fracture, congenital or acquired deformities (scoliosis, etc.), spinal stenosis, spondylolisthesis, ankylosing spondylitis.
It is possible for various somatic diseases (heart, stomach, pancreas, kidneys, pelvic organs, etc.) through the mechanism of referred pain.
The examination of a patient with back pain requires careful consideration. Any back pain cannot be attributed to “osteochondrosis” - a condition that is detected by X-ray examination in most middle-aged and elderly people. Neurological manifestations of spinal osteochondrosis and myofascial pain are characterized by painful muscle spasms and limited mobility of the spine.
The diagnosis of reflex and compression complications of osteochondrosis is based on clinical data and requires the exclusion of other possible causes of back pain. X-rays of the spine are used mainly to exclude congenital anomalies and deformities, inflammatory diseases (spondylitis), primary and metastatic tumors. X-ray CT or MRI can identify a disc herniation, determine its size and location, and also detect spinal stenosis and a spinal cord tumor.
The diagnosis of myofascial pain is based on clinical findings (identification of painful muscle tension in one or more muscles) and requires the exclusion of other possible causes of pain; differential diagnosis with reflex syndromes (muscular-tonic syndromes) due to spinal osteochondrosis often causes difficulties; a combination of these diseases is possible.
Treatment of reflex syndromes and radiculopathy due to osteochondrosis is based in the acute period on ensuring rest - the patient is advised to avoid sharp bends and painful positions. Prescribed bed rest for several days until the sharp pain subsides, a hard bed (a shield under the mattress), taking centrally acting muscle relaxants, and, if necessary, additional analgesics and non-steroidal anti-inflammatory drugs. To facilitate movement during this period, you should wear a neck or lumbar corset (fixing belt). You can use physiotherapeutic analgesic procedures, rubbing in pain-relieving ointments, compresses with a 30-50% solution of dimexide and novocaine, novocaine and hydrocortisone blockades. As pain subsides, a gradual increase in physical activity and muscle strengthening exercises are recommended.
In the chronic course of reflex syndromes and radiculopathies, manual therapy, reflexology, physiotherapeutic treatment, and sanatorium-resort treatment can be effective. Surgical treatment (removal of a herniated disc) is necessary in those rare cases when compression of the spinal cord or cauda equina roots occurs. Surgical treatment is also indicated for discogenic radiculopathy, accompanied by severe paresis, and in case of long-term (more than three to four months) lack of effect from conservative treatment and the presence of a large disc herniation. To prevent exacerbations of osteochondrosis, it is recommended to avoid provoking factors (lifting large loads, carrying a heavy bag in one hand, hypothermia, etc.), and regularly engage in therapeutic exercises.
For myofascial pain, it is necessary to keep the muscle at rest for several days. As treatment, you can prescribe muscle stretching exercises (post-isometric relaxation), physiotherapy, reflexology or local injection of anesthetics into trigger zones, compresses with dimexide and anesthetics.
As already noted, for both acute pain and chronic pain syndromes, the treatment of painful muscle spasms is of great importance. Tonic muscle tension can not only cause pain in itself, but can also cause deformation and limit the mobility of the spine, as well as cause compression of the nerve trunks and vessels passing nearby. For its treatment, in addition to non-steroidal anti-inflammatory drugs, analgesics (for example, nimulide in the form of a transdermal gel for local therapy or in the form of lingual tablets for acute pain syndrome), physiotherapy and therapeutic exercises, muscle relaxants are used as first-line drugs - drugs that can break the “vicious circle" of pain syndrome [2].
To treat painful muscle spasms, muscle relaxants are used orally or parenterally. By reducing reflex muscle tension, muscle relaxants reduce pain, improve motor functions and facilitate physical therapy. Treatment with muscle relaxants begins with the usual therapeutic dose and continues as long as the pain syndrome persists; As a rule, the course of treatment lasts several weeks. A number of studies have proven that in the case of painful muscle spasms, adding muscle relaxants to standard therapy (non-steroidal anti-inflammatory drugs, analgesics, physiotherapy, therapeutic exercises) leads to a more rapid regression of pain, muscle tension and improved spinal mobility.
Mydocalm, baclofen and sirdalud are used as muscle relaxants. Muscle relaxants are usually not combined with each other. To relieve painful muscle spasms, you can also use diazepam (Seduxen, Relanium) in an individually selected dose.
Baclofen has a muscle relaxant effect mainly at the spinal level. The drug is close in structure to γ-aminobutyric acid (GABA); it binds to presynaptic GABA receptors, leading to a decrease in the release of excitatory amino acids (glutamate, aspratate) and suppression of mono- and polysynaptic activity at the spinal level, which causes a decrease in muscle tone; baclofen also has a moderate central analgesic effect. It is well absorbed from the gastrointestinal tract, the maximum concentration in the blood is reached 2-3 hours after administration. The initial dose is 15 mg per day (in three doses), then the dose is increased by 5 mg every day until the desired effect is obtained, the drug is taken with meals. Usual doses for the treatment of painful muscle spasms are 20-30 mg. The maximum dose of baclofen for adults is 60-75 mg per day. Side effects often include drowsiness and dizziness. Sometimes nausea, constipation, diarrhea, and arterial hypotension occur; Caution is required when treating elderly patients.
Sirdalud (tizanidine) is an α-2 adrenergic receptor agonist. The drug reduces muscle tone due to suppression of polysynaptic reflexes at the level of the spinal cord, which can be caused by inhibition of the release of excitatory amino acids and activation of glycine, which reduces the excitability of spinal cord interneurons; Sirdalud also has a moderate central analgesic effect. When taken orally, the maximum concentration of sirdalud in the blood is reached within an hour; food intake does not affect its pharmacokinetics. The initial dose of the drug is 6 mg per day in three doses, the average therapeutic dose is 12-24 mg per day, the maximum dose is 36 mg per day. Side effects include drowsiness, dizziness, and a slight decrease in blood pressure; Caution is required when taking the drug in elderly patients.
Mydocalm (tolperisone) has been widely used for a long time in the treatment of reflex and compression complications of degenerative changes in the spine (osteochondrosis, spondylosis, spondyloarthrosis) and myofascial pain [3]. Mydocalm has a predominantly central muscle relaxant effect. A decrease in muscle tone when taking the drug is associated with a depressive effect on the caudal part of the reticular pharmacy and suppression of spinal reflex activity. The drug has a moderate central analgesic effect and a slight vasodilator effect. Mydocalm intake begins with 150 mg per day three times a day, gradually increasing the dose until the effect is obtained, in adults usually up to 300-450 mg per day. For a quick effect, the drug is administered intramuscularly at 1 ml (100 mg) twice a day or intravenously at 1 ml once a day.
The effectiveness and safety of the use of mydocalm for painful muscle spasms was proven in a double-blind, placebo-controlled study [4]. In eight study centers, 110 patients aged 20 to 75 years were randomized to receive mydocalm 300 mg per day or placebo in combination with physical therapy and rehabilitation for 21 days. The pain threshold of pressure, measured using a special device (Pressure Tolerance Meter) at 16 symmetrical points of the torso and limbs, is considered as an objective criterion for the effectiveness of treatment. In addition, patients subjectively assessed their condition based on the intensity of pain, the feeling of muscle tension and spinal mobility; the doctor also assessed muscle tension and spinal mobility. Before the start of treatment and after its completion, a detailed clinical and laboratory examination was carried out, including an ECG, blood pressure measurement, and a biochemical blood test for 16 indicators.
According to research results, the use of mydocalm significantly reduces painful muscle spasms, measured objectively by instrumental methods. The difference between the treatment and placebo groups, which was observed as early as the fourth day, gradually increased and became statistically significant on the 10th and 21st days of treatment, which were chosen as endpoints for evidence-based comparison. An analysis of the subjective assessment of treatment results given by doctors and patients after its completion (21 days) showed that in the group of patients receiving Mydocalm, the treatment results were significantly more often assessed as very good, while in the placebo group there was no effect significantly more often. According to the subjective assessment of the results of treatment given by patients after its completion (after 21 days), no significant differences were identified regarding the tolerability of mydocalm and placebo. The vast majority of patients had good tolerability of mydocalm. ECG results, biochemical and hematological parameters in the group of patients taking both mydocalm and placebo also did not differ.
It is important to note that more than half (62%) of the patients included in the study were receiving other types of therapy before the study began, and most of them (68%) did not experience improvement. This demonstrates the effectiveness of Mydocalm in the treatment of painful muscle spasms that are resistant to other types of therapy.
Parenteral administration of mydocalm can quickly relieve pain and reduce muscle tension. In vertebrogenic muscular-tonic syndrome, intramuscular administration of 100 mg mydocalm relieves pain after 1.5 hours, and treatment with mydocalm for a week at 200 mg/day intramuscularly, and then for two weeks at 450 mg/day orally has a significant advantage over standard therapy; At the same time, therapy with mydocalm not only reduces pain, but also relieves anxiety and increases mental performance [1].
For painful muscle spasms, the advantages of mydocalm, in addition to its effective muscle relaxant and analgesic effect, are the absence of side effects and good interaction with non-steroidal anti-inflammatory drugs, which in many cases makes it possible to reduce the dose of the latter and, as a result, weaken or even completely eliminate their side effects without reducing the effectiveness of treatment.
An important advantage of mydocalm over other muscle relaxants is the absence of sedation and muscle weakness when taking it. This benefit was proven in a double-blind, placebo-controlled study [5]. The study included 72 healthy volunteers aged 19 to 27 years (mean age 21.7 years). The study was carried out over eight days, during which time volunteers randomized to receive 150 or 450 mg of mydocalm per day in three divided doses or placebo, also in three divided doses. Neuropsychological studies are carried out in the morning on the first and last (eighth) days of the study before and after taking mydocalm after 1.5, 4 and 6 hours or placebo. The results of the study did not show any significant differences in the speed of sensorimotor reactions and the speed of performing various psychological tests 1.5, 4 and 6 hours after taking mydocalm at a dose of 50 or 150 mg or placebo. Similar studies conducted on the eighth day from the start of taking mydocalm also did not show significant differences compared to the placebo group. This indicates the good tolerability of mydocalm and the possibility of prescribing it in cases where the patient’s occupation requires maintaining quick reactions and the ability to concentrate, including when driving a car.
Thus, painful muscle spasm is one of the most common causes of back pain (due to reflex syndromes of osteochondrosis or myofascial pain). In such cases, it is recommended to use muscle relaxants in combination with various medications, physiotherapy and therapeutic exercises. In recent years, the effectiveness and safety of the muscle relaxant mydocalm has been proven, which does not cause a sedative effect and is available in a form for parenteral administration to quickly relieve pain.
Literature.
- Avakyan G.N., Chukanova E.I., Nikonov A.A. The use of mydocalm in the relief of vertebrogenic pain syndromes // Journal. neurol. and psychiatrist. 2000. No. 5. P. 26-31.
- Parfenov V. A., Yakhno N. N. Neurology in general medical practice. - M., 2001.
- Parfenov V. A. Mydocalm in neurological practice // Treatment of nervous diseases. 2002. No. 2. P. 10-12.
- Pratzel HG, Alken RG, Ramm S. Efficacy and tolerance of repeated doses of tolperisone hydrochloride in the treatment of painful reflex muscle spasm: results of a prospective placebo-controlled double-blind trial // Pain. 1996. Vol. 67.- P. 417-425.
- Dulin J., Kovacs L., Ramm S. et al. Evaluation of sedative effects of single and repeated doses of 50 mg and 150 mg tolperisone hydrochloride. Results of a prospective, randomized, double-blind, placebo-controlled trial // Pharmacopsychiat. 1998. Vol. 31. P. 137-142.
V. A. Parfenov, Doctor of Medical Sciences, Professor of MMA named after. I. M. Sechenova T. T. Batysheva, Candidate of Medical Sciences Polyclinic for Rehabilitation No. 7 of Moscow
Instrumental methods for diagnosing intercostal neuralgia
At the Medica24 International Clinic, you can undergo examination using our own diagnostic equipment, which meets the most modern standards. It will help diagnose the disease at an early stage and take timely measures.
First of all, it is important to carry out a differential diagnosis of intercostal neuralgia with certain diseases of the spine, cardiovascular system, and lungs. To do this, if necessary, the neurologist will refer you for a consultation with a cardiologist or pulmonologist.
You may be prescribed an ECG, Holter monitoring, cardiac ultrasound, X-ray, CT and MRI of the chest, biochemical blood test, and bacteriological studies.
Neuralgia during pregnancy
If intercostal neuralgia appears in a pregnant woman, how to diagnose it and how to treat it is decided by a neurologist together with a gynecologist. Therapy is selected taking into account possible negative effects on the fetus. Self-medication in this situation is considered unacceptable, as this can have a negative impact on the health of the expectant mother and child.
To prevent chest neuralgia from appearing during pregnancy, it is advisable to follow preventive measures. If a woman has previously had attacks of thoracalgia, then at the stage of preconception preparation she should visit a neurologist and osteopath. The doctor will conduct a diagnosis, and then the neurologist will give a number of recommendations on how to treat intercostal neuralgia. An osteopath will identify possible causes of neuralgia and conduct a treatment session aimed at eliminating them.