Headache, nausea and vomiting, difficulty swallowing
Olga Zheludkova, pediatric oncologist of the highest category, Doctor of Medical Sciences, Professor of the Russian Scientific Center of X-ray Radiology:
“Headache - especially increasing pain - is a common symptom of a brain tumor. Usually it looks like this: I had a headache, my mother gave me a pill, a week later it happened again, a day later it happened again. Another common symptom is vomiting in the morning, which brings relief. The child gets out of bed, vomits, and feels better. Parents should be alarmed when this occurs not for the first time, but repeatedly, within a week or month. It is important to understand that ordinary gastroenterological problems, as a rule, recur every day, and vomiting with brain tumors may not be daily, but once every three days or once a week. And vomiting due to brain tumors does not fade over time, but, on the contrary, increases. Parents who notice this should urgently go to an ophthalmologist and ask him to look at the fundus and evaluate the child’s visual acuity, even if there are no obvious vision problems. And with this data, go to a neurologist. You should also be wary when there is a swallowing disorder. Usually it manifests itself as follows: while eating liquid food, the child develops coughing and choking.”
Symptoms
When brain cancer appears, symptoms in the early stages are local and depend on the location of the tumor. The disease manifests itself:
- impaired sensitivity in certain parts of the body, deterioration of orientation in space;
- memory impairment;
- decreased muscle activity up to complete paralysis;
- convulsive seizures of an epileptic nature;
- hearing damage and decreased speech recognition function;
- partial or complete visual dysfunction;
- partial or complete loss of the ability to write and speak;
- weakness, fatigue;
- pathological changes in the production of hormones from the pituitary gland or hypothalamus;
- changes in character, emotional imbalance;
- decrease in intellectual level;
- the appearance of hallucinations.
The first signs of brain cancer appear as minor changes in one or more of these areas, but the deterioration progresses over time. With a significant increase in pressure inside the skull, general cerebral symptoms appear:
- persistent headaches of high intensity that cannot be relieved with analgesics;
- dizziness caused by compression of the cerebellum or decreased blood supply to brain structures;
- vomiting independent of food intake.
Anorexia, behavior changes, depression
Irina Tatarova, child psychiatrist, candidate of medical sciences, consultant physician at the Russian Children's Clinical Hospital:
“Parents definitely need to pay attention to sudden changes in the child’s behavior. If he becomes irritable, excitable, if he loses control over his actions, if a previously active child suddenly becomes drowsy and lethargic, you need to take him to the doctor. These symptoms should alert you if the child has not behaved this way before and if there were no apparent reasons for the change in behavior - illness, stress or severe fatigue.
Sudden mood swings can also be a cause for anxiety: causeless uncontrollable laughter or crying, euphoria turning into aggression, or sudden attacks of fear. Sometimes children with brain tumors also experience hallucinations. Young children cannot tell their parents about this, so you need to monitor their behavior. If a child suddenly freezes, his eyes widen, if he looks for a long time and points to an empty space, this is a reason to contact a specialist. Many symptoms also accompany depression. But this is not a specific symptom, which in case of brain tumors is usually combined with other manifestations of the disease.
With all these symptoms, parents often take their child to a psychologist, but first of all they need to consult with a neurologist and a psychiatrist - and it is advisable for these two doctors to work in pairs. Unfortunately, sometimes symptoms are associated with autism spectrum disorders, so it is important to contact competent specialists who will conduct a comprehensive examination of the child.
Anorexia can also be a symptom of a brain tumor. If it is caused by psychological reasons, the child consciously begins to limit himself in food, avoids dinners with his family, and looks at himself in the mirror. But if a child eats normally and suddenly begins to lose weight sharply, parents should take him to an endocrinologist.”
Convulsions, weakness, loss of consciousness
Vladimir Solovyov, neurologist-epileptologist, head of the laboratory for pre-surgical diagnosis of epilepsy at the Morozov Children's City Clinical Hospital, doctor at the video-EEG laboratory of the Epilepsy Center:
“The main neurological symptoms of a brain tumor, in addition to headaches, are seizures and loss of consciousness. Of course, anyone can faint: for example, this happens with children of asthenic physique, or with overwork and hormonal changes in the body. But if a disturbance of consciousness occurs unexpectedly, without physical activity, then this is a reason to go to the doctor. In any case, seizures should also be seen by specialists. Very young children may experience febrile seizures - seizures during fever and infectious diseases. Most likely, such seizures will not be a symptom of a brain tumor, but it is still necessary to exclude this. Well, if attacks bother children older than one year, then this is definitely a reason to consult a doctor.
Another symptom is general weakness. He should be alert if this happens systematically, if it is clear that the child is not pretending. It’s one thing when he doesn’t want to go to school in the morning, and it’s a completely different thing when you and your whole family go to the zoo, and the child doesn’t have the strength, although he always really wanted to go there.
Unfortunately, specialists do not always immediately prescribe the necessary examinations for children. In my practice, I often encounter the fact that instead of an MRI, children are referred for an ultrasound of the brain vessels. Doctors suspect vasoconstriction, which allegedly causes chronic oxygen deprivation and headaches. Some people even try to blame it on a migraine, but how can a six-year-old child get a migraine? Then the parents themselves do an MRI, and there the tumor is in an advanced stage. This also happens.
At my appointments, I always advise parents to get a second opinion, especially when it comes to a serious illness. If parents suspect something, it is better to hear from a second specialist. Moreover, if the doctor at the appointment without hesitation says that there is no need to do an MRI, that everything is fine - it’s just a headache and will go away soon. It is important to remember that even one of the above symptoms is enough to consult a specialist.”
Leukemia
Among all malignant tumors of childhood, the proportion of leukemia is high - up to 35-50%. Peak incidence is between 2 and 4 years of age. Boys get sick 1.5 times more often than girls. Lethargy, weakness, irritability, increased fatigue, unclear fever, pallor, decreased appetite, hemorrhages on the skin, bleeding (usually nasal), pain in the bones and joints, enlarged peripheral lymph nodes, enlarged abdomen due to an enlarged spleen and liver, stomatitis, gingivitis is often the reason for the initial visit to a medical professional. In a clinical blood test, a combination of a sharp decrease in red blood cells, hemoglobin with a normal color indicator (normochromic anemia), an increase or decrease in leukocytes, a decrease in platelets, an increase in ESR, an increase in lymphocytes due to undifferentiated lymphoid cells (blasts). At the slightest suspicion of acute leukemia, a bone marrow puncture is indicated to identify changes in the bone marrow inherent in this disease.
There are acute and chronic leukemia (leukemia or leukemia); in children, acute leukemia predominates. There are 3 main options:
Acute lymphoblastic leukemia;
Acute myeloblastic leukemia and its variants:
a) acute promyelocytic leukemia;
b) acute myelomonoblastic leukemia;
c) acute erythromyeloid leukemia;
3) acute monoblastic leukemia.
When a diagnosis is made, the child is subject to urgent hospitalization for special and accompanying therapy. General principles of treatment: early onset, radicality by prescribing several cytostatic drugs at once in full therapeutic doses on strictly defined days. Strictly regulated days of treatment constitute one cycle, several cycles constitute a polychemotherapy course of treatment. Each cytological (cytochemical) variant of leukemia has its own optimal program. There are several phases in the treatment process:
- induction of remission (weakening);
— consolidation (strengthening) of remission;
— reinduction of remission (anti-relapse treatment);
- maintenance therapy.
Growth problems, delayed puberty or early puberty, diabetes insipidus
Nadezhda Mazerkina, endocrinologist of the highest category, Doctor of Medical Sciences, doctor of the children's department of the National Medical Research Center for Neurosurgery named after. ak. N. N. Burdenko:
“Parents should first of all be alert to the following symptoms: growth retardation, premature or late puberty, as well as symptoms of diabetes insipidus: thirst and polyuria - that is, a frequent urge to go to the toilet, especially at night. If a child has at least one of these symptoms, parents need to take him to a good endocrinologist: he should figure it out.
It is very important to pay attention to the child's growth rate. To do this, it is necessary to regularly measure growth and record it, and observe it over time. A growth rate of less than four centimeters per year is suspicious - there is a high probability that the reasons are related to hormonal disorders. You also need to monitor the appearance of signs of puberty in the child: if they appear in a girl before the age of eight, and in a boy before the age of nine, then this is a reason to consult a doctor. The same can be said about delayed puberty. You should be concerned if a girl shows no signs of puberty after 13 years, and a boy does not show signs of puberty after 14 years.
It is worth mentioning separately about obesity: in itself it usually does not become a symptom of a brain tumor, but if excess weight is combined with any of the above symptoms, this is a cause for alarm. You should also be concerned if the change in weight is accompanied by deterioration of vision or severe headaches in the child. Quite rarely, cachexia can be a symptom: sudden weight loss for no apparent reason. The child becomes very thin, even to the point of exhaustion. You need to see a doctor if your weight change is really pronounced. Many children, for various reasons, get better and lose several kilograms - in these cases, of course, it’s not worth sending them for an MRI.”
Chapter 8.
Tumors of the central nervous system occupy the first place in frequency among solid malignant tumors in children, accounting for 20% of all cancer incidence in childhood. These tumors occur with a frequency of 2-2.8 per 100,000 children, ranking second among the causes of death in children with cancer. Children of preschool age get sick more often: the peak incidence occurs at 2-7 years. Although the mortality rate from these tumors still exceeds the mortality rate for many malignant processes in children, modern therapeutic approaches and the latest advances in diagnostic capabilities, allowing early diagnosis of the tumor and accurate treatment planning, make it possible to cure more children.
The etiology of this group of tumors is currently unknown, although there is evidence of the predisposition of patients, for example, with Recklinghausen's disease (neurofibromatosis), to the development of brain gliomas. There is a known connection between the occurrence of medulloblastomas in children and basal cell nevus syndrome (skin lesions, abnormalities of the skeleton, skin, hands, feet, and abnormalities of the central nervous system). An increased incidence of brain tumors is observed in children with congenital immunodeficiency and in children with ataxia-telangiectasia.
Often a brain tumor occurs as a second tumor in children suffering from acute leukemia, hepatocellular cancer, and adrenocortical tumors. All these data indicate the presence of a number of predisposing factors for the development of malignant brain tumors, which will need to be deciphered and their impact on prognosis determined in the future.
Classification of brain tumors in children.
According to the WHO international classification (1990, second edition), the biological behavior of CNS tumors is determined (in addition to the presence of histological differentiation features) by the so-called degree of malignancy, or anaplasia: from I (benign) to IV (malignant). Tumors of a low degree of malignancy include tumors of I-II degrees (Low grade), and those of a high degree of malignancy - III-IV degrees (High grade).
The histological structure of brain tumors in children differs significantly from that in adults (Table 10-1). Meningiomas, schwannomas, pituitary tumors and metastases from other organs, which relatively often affect the brain of adult patients, are very rare in childhood. In children, 70% of tumors are gliomas. In adults, tumors are more often localized supratentorially, affecting mainly the cerebral hemispheres,
In children under 1 year of age, supratentorial tumors also dominate, and these are mainly low-grade gliomas, PNETs (primitive neuroectoderm tumors), choroid plexus tumors, teratomas and meningiomas.
The first classification of brain tumors was proposed in the 20s of our century by Bailey and Cushing. This classification is based on the histogenesis of brain tissue and all subsequent classifications are based on this principle.
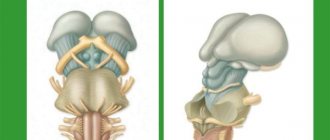
Brain tumors diagnosed in children in the first years of life have a central location, i.e. most often affect the third ventricle, hypothalamus, optic chiasm, midbrain, pons, cerebellum and fourth ventricle. Despite the fact that the volume of brain matter in the posterior cranial fossa is only a tenth of the total volume of the brain, more than half of all malignant brain tumors in children over 1 year of age are tumors of the posterior cranial fossa. These are mainly medulloblastomas, cerebellar astrocytomas, brainstem gliomas and fourth ventricle ependymomas.
Supratentorial tumors in children are represented by astrocytomas that arise in the frontal, temporal and parietal regions of the brain, ependymomas of the lateral ventricles and craniopharyngiomas. (Table 8-2)
Clinical picture.
Generally speaking, any brain tumor has malignant behavior regardless of its histological nature, since its growth occurs in a limited volume, and regardless of the histological nature of the tumor, the clinical picture of all brain tumors is determined mainly by the localization of tumor growth, age and premorbid level of development of the patient child.
Tumors of the central nervous system can cause neurological disorders by directly infiltrating or compressing normal structures, or indirectly by causing obstruction of the CSF pathways.
The factor that determines the dominant symptoms in children with brain tumors is increased intracranial pressure, resulting in the classic triad of morning headache, vomiting and drowsiness. Severe, recurrent headaches rarely occur in children, but it is all the more important to pay attention to this complaint. Seizures are the second most common symptom after headache, especially in children with supratentorial tumors. In approximately a quarter of these patients, seizures are the first manifestation of the tumor. Sometimes these children tend to tilt their heads to one side. Involvement of the cerebellum can cause ataxia, nystagmus and other cerebellar disorders. When the brain stem is damaged, bulbar disorders (dysarthria, paresis and cranial nerve palsies) are observed. Hemiparesis of the opposite side, resulting from compression of the corticospinal pathways, is one of the common symptoms. Visual impairment - decreased visual acuity, double vision and a number of other eye symptoms are a reason for a thorough examination of the child. In children under one year of age, rapid or slow development of macrocephaly with bulging of a large fontanel is possible. If the tumor disseminates along the spinal canal, back pain and dysfunction of the pelvic organs may appear.
Currently, with the introduction of modern diagnostic methods into practice, it is possible to detect a tumor quite early, provided that a child with neurological symptoms is referred to CT and MRI in a timely manner.
Diagnostics.
In addition to routine clinical examinations, including an examination by an ophthalmologist, such children must undergo CT and MRI with contrast material of the brain and spinal cord. Especially when the tumor is localized in the posterior fossa, MRI is extremely informative, since this method has a high resolution. These studies have successfully replaced invasive procedures such as arterial angiography or air ventriculography.
Histological verification of the tumor is necessary, but sometimes difficult due to technical difficulties associated with the localization of the tumor, which involves vital structures in the process. Currently, with the gradual introduction into the practice of neurosurgeons of a new high-tech method of surgical intervention - stereotactic surgery, it is becoming possible to perform tumor biopsies of almost any location. Sometimes, due to a significant increase in intracranial pressure, the first step is bypass surgery, which significantly improves the neurological status of the patient.
Examination of the cerebrospinal fluid will provide information about the possible extracranial spread of the malignant process. In rare cases of tumor spread beyond the central nervous system (for example, in the presence of medulloblastoma), additional diagnostic measures are necessary, such as OSG, chest X-ray, abdominal ultrasound, myelogram.
Treatment.
The prognosis of the disease depends to a very large extent on the completeness of tumor removal, which is especially true for high-grade tumors such as malignant astrocytomas, medulloblastomas and PNETs. However, very often radical surgery is associated with significant damage to the normal structure of the brain, which subsequently has an extremely negative impact on the neurological and mental status of surviving patients. Foreign studies in recent years have convincingly shown that the neurological status of patients treated for tumors of the posterior cranial fossa depends to a very large extent on the amount of destruction of brain tissue that arose not only as a result of the growth of the tumor itself but also as a result of surgical intervention. Therefore, ideally, such children should be operated on by a pediatric neurosurgeon who has sufficient experience in treating these patients.
In recent years, radiation therapy has become firmly established in the standard treatment of central nervous system tumors and plays a leading role among conservative methods of treating this pathology. The volume of radiation (craniospinal or local) and dose depend on the nature of the tumor and its location. (see section LT). Due to the unsatisfactory results of treatment of high-grade gliomas and inoperable medulloblastomas, attempts to use polychemotherapy for various brain tumors, sometimes with significant success, have recently been of great interest.
Astrocytomas
Astrocytomas are divided into two large groups: low grade and high grade.
Low-grade gliomas. (Low grade). More than half of gliomas in children are histologically benign. Low grade (i.e., pilocytic and fibrillar) astrocytomas have a pleomorphic structure, sometimes containing stellate structures, giant cells and microcysts. They exhibit epithelial proliferation with low mitotic activity.
The prognosis for these children depends on the location of the tumor and its resectability. Most of these tumors can be radically removed. In these cases, treatment is limited to surgery. If radical surgery is not possible or there is a residual tumor after surgery, then the issue of further treatment should be decided taking into account factors such as the child’s age, morphological structure and volume of the residual tumor. Since these tumors have a low growth rate, most researchers adhere to the “wait and see” practice, i.e. dynamic monitoring with regular CT and MRI, and begin re-treatment of such children only in case of tumor progression. If surgical removal of the tumor is not possible, radiation therapy to the tumor area is indicated at a dose of 45-50 Gy. There is no consensus regarding chemotherapy for low-grade astrocytomas. Currently, a number of foreign clinics are conducting randomized studies on the use of chemotherapy in such patients.
The choice of treatment tactics in a number of patients is quite difficult, especially with tumors arising from the diencephalic region in children under 3 years of age, since the main method of treatment, radiation therapy, is not applicable at this age due to the severe neurological and endocrinological consequences of treatment in this age group .
Thalamic/hypothalamic/(diencephalic) gliomas. Most often these are benign tumors (the most common are pilocytic astrocytomas). By the time of diagnosis, these tumors typically involve the diencephalon, optic nerves, and optic tract throughout, causing progressive visual impairment and proptosis along with symptoms of increased intracranial pressure. Localization of the tumor in the hypothalamus causes behavioral problems in the child. Spread to the pituitary region may cause precocious puberty or secondary hypopituitarism. Obstruction of the foramen of Monroe leads to hydrocephalus. These tumors are most often found in children under 3 years of age.
Optic tract gliomas are most often low-grade pilocytic and sometimes fibrillary astrocytomas. They make up approximately 5% of all CNS neoplasms in children. More than 75% of tumors affecting the optic nerves occur during the first decade of life, while chiasmal lesions are more common in older children (Figure 8-3).
Page 186
Approximately 20% of children with optic chiasma gliomas suffer from neurofibromatosis, and a number of researchers argue that the prognosis for such children is better than for patients without neurofibromatosis. The course of intracranial tumors is more aggressive than gliomas located intraorbitally. Surgical removal of intraorbital tumors can often be total and in these cases it is recommended to resect the optic nerve at the maximum possible distance (up to the chiasm) in order to reduce the risk of recurrence. It is almost impossible to radically remove chiasmal tumors, but surgery—a biopsy—is necessary in such patients for the purpose of differential diagnosis, and sometimes partial resection improves the neurological status of these patients.
With tumor progression in children over 5 years of age, local radiation therapy at a dose of 55 Gy is indicated. Radiation therapy helps to at least stabilize the process within 5 years, although late relapses of the disease often occur.
If relapse occurs, chemotherapy is an alternative to radiation therapy. In young children, the combination of vincristine and dactinomycin has worked well, achieving 90% survival of patients within 6 years after relapse (Packer, 1988). This is especially important since the use of chemotherapy makes it possible to postpone radiation in young children. A number of studies indicate the high effectiveness of carboplatin in this type of tumor, as well as in most low-grade gliomas.
Older children have a slightly better prognosis than younger children and overall survival is about 70%. Patient survival rates range from 40% for intracranial tumors to 100% for patients with intraorbital tumors.
High-grade astrocytomas, or anaplastic gliomas, account for 5-10% of brain tumors, and in children these tumors have a more favorable course compared with similar processes in adults. The most common malignant gliomas are anaplastic astrocytoma and glioblastoma multiforme. They are characterized by the presence of characteristic “malignant” features, such as high cellularity, cellular and nuclear atypia, high mitotic activity, the presence of necrosis, endothelial proliferation and other features of anaplasia. Clinically, these tumors are very aggressive and are capable not only of invasive intracranial growth and seeding of the spinal canal, but also of spreading beyond the central nervous system, metastasizing to the lungs, lymph nodes, liver, and bones, which, however, is much more common in adult patients. The prognosis in such patients depends on the completeness of tumor resection, although total removal is hardly possible due to infiltrating growth.
Radical removal is possible if the tumor is localized in the frontal or occipital lobes of the brain. Postoperative local irradiation of these tumors with a dose of 50 - 60 Gy is the standard approach in most clinics around the world. The use of radiation improves the survival rate of such patients by up to 30%.
The role of chemotherapy in the treatment of these tumors remains controversial. Encouraging results were obtained in the USA using adjuvant polychemotherapy using lomustine and vincristine (Packer, 1992). In older patients, good results were obtained using a combination of CCNU, procarbazine and vincristine in the treatment of grade III gliomas (Kyritsis, 1993). The overall 5-year survival rate for low grade astrocytomas is about 60%, for high grade astrocytomas it is only 25%.
Cerebellar astrocytomas are indolent tumors that occur in two histological subtypes: juvenile piloid tumor with elongated unipolar cells and fibrillar structures and diffuse low-grade tumor. The tumors may contain cysts and are usually resectable. Rarely, these tumors can spread beyond the skull with dissemination along the spinal canal. The possibility of late malignant transformation of these tumors has been described. If radical surgery is not possible after partial tumor resection, local radiation therapy at a dose of 55 Gy is justified.
Anaplastic gliomas of the posterior fossa are treated similarly to gliomas of cortical localization, however, due to their ability to seed the spinal canal, these children in the postoperative period should receive craniospinal irradiation with a local increase in dose, as is used in the treatment of medulloblastomas. Adjuvant chemotherapy similar to that used in the treatment of supratentorial gliomas is also used in the treatment of these patients. The overall 10-year survival rate after total tumor removal is about 90%; in the case of complete tumor removal, survival rates range from 67 to 80%.
Medulloblastoma or PNET.
Medulloblastoma is the most common infratentorial tumor, with a typical location in the midline of the cerebellum. Located supratentorially, this tumor is called PNET. The peak diagnosis of these tumors is observed at the age of 5 years.
These tumors belong to the family of small round cell tumors and have an identical morphological structure. Tumors contain neural structures of varying degrees of differentiation with the formation of rosettes and stellate structures. The desmoplastic subgroup contains areas of connective tissue with nests of malignant cells. This type is the most favorable prognostically, since these tumors are localized superficially and are most often easily removed. They are highly malignant and tend to seed the spinal canal early and quickly. Therefore, the range of mandatory initial examination of these patients should include NMR scanning of the entire central nervous system with a contrast agent (gadolinium) and examination of the cerebrospinal fluid. Among all malignant neoplasms of the central nervous system, medulloblastoma has the highest capacity, although rarely, to metastasize beyond the central nervous system, for example, to the bone marrow, skeletal bones, lungs, liver and lymph nodes. Even in the case of seemingly radical removal of the primary tumor, morphological examination often indicates a microscopically non-radical intervention. Therefore, in any case, the treatment of such patients is not limited to surgery. The treatment complex for such patients necessarily includes radiation and chemotherapy.
Medulloblastoma is the most sensitive tumor of the central nervous system to chemoradiotherapy. In the treatment of this tumor, it is standard to carry out craniospinal irradiation at a dose of 34-35 Gy and additionally to the posterior cranial fossa - 20 Gy up to a total focal dose of 55 Gy. (see chapter “Radiation therapy”). For young children, RT doses can be reduced (since high doses of radiation cause adverse long-term consequences), which, accordingly, significantly increases the risk of relapse. When performing craniospinal irradiation, the radiologist should avoid overlapping the irradiation fields of the skull and spine due to the risk of radiation myelitis. Radiation therapy is not indicated for children under 3 years of age due to the sharply negative consequences of cranial irradiation at this age. Therefore, in early childhood, only polychemotherapy is performed either in the postoperative period or if surgery is impossible - as the only method of antitumor therapy. Reports in recent years indicate the successful use of combinations of vincristine, CCNU and steroids in young patients. Medulloblastoma is the most sensitive tumor of the central nervous system to chemotherapy. Treatment protocols adopted in different countries include different combinations of chemotherapy drugs. The CCSG protocol (USA) involves the use of a combination of vincristine, lomustine and cis-platinum. The International Society of Pediatric Oncology (SIOP) protocol uses a combination of vincristine, carboplatin, etoposide, and cyclophosphamide.
As has been shown in recent years, the effective use of chemotherapy may reduce radiation exposure in children with medulloblastoma.
For medulloblastoma, negative prognosis factors are the child's age under 5 years, male gender, non-radical tumor removal, involvement of the trunk in the process, extracranial spread, non-desmoplastic type of histology. 5-year survival rate is 36 - 60% (Evans, 1990)
Ependymoma.
This tumor arises from the inner lining of the ventricles of the brain or the lining of the central canal and accounts for approximately 5-10% of tumors of the central nervous system. In children, 2/3 of these tumors are localized in the posterior cranial fossa. More than half of the patients are children under 5 years of age. About 10% of all ependymomas arise in the spinal cord, but in these cases the tumor rarely affects children under 12 years of age.
Like medulloblastoma, ependymoma can infiltrate the brain stem and seed the spinal canal, which significantly worsens the prognosis, but more often these tumors tend to differentiate and are more benign. Its radical removal is always very difficult, although this is the cornerstone in the treatment of these patients. Therapeutic approaches are similar to those for medulloblastoma, although if the tumor is supratentorial, if it is completely removed and the histology is favorable, spinal irradiation can be excluded. Among the chemotherapeutic agents used in the treatment of ependymomas, platinum drugs are the most active. The 5-year survival rate of these patients is 40%. The best prognosis is for children with spinal tumor localization, especially in the cauda equina.
Brain stem gliomas.
These tumors account for 10-20% of all central nervous system tumors in children. These tumors infiltrate and compress the brain stem, causing multiple cranial nerve palsies, i.e. Due to their anatomical location, these tumors manifest relatively early. Most often they are localized in the bridge. According to their histological structure, they can belong to both low and high degrees of malignancy. The type of growth (exophytic or infiltrative) significantly affects the prognosis. The prognosis for an exophytically growing tumor with a low degree of malignancy can be 20%, while infiltrative high-grade gliomas are practically incurable. These tumors are diagnosed using CT and MRI with a high degree of confidence, so the extremely dangerous procedure of biopsy of a tumor in this location may not be performed. The exception is exophytically growing tumors, when it is possible to remove them, which significantly improves the prognosis in such patients.
Treatment of such patients includes local irradiation at a dose of 55 Gy with a noticeable improvement in the neurological status of these patients, but in more than 30% of cases there is a relapse of the disease on average 6 months from the start of therapy. Currently, studies are being conducted in the USA and Great Britain on the effectiveness of hyperfractionated irradiation and the use of aggressive chemotherapy regimens due to extremely unsatisfactory long-term treatment results. Attempts to improve the situation using additional chemotherapy have not yet led to significant success, but encouraging results have been obtained in the United States using platinum drugs.
Pineal tumors.
Tumors of the pineal region combine tumors of different histogenesis, but are usually described together due to their location. The incidence of damage to this area is 0.4 - 2% of all central nervous system tumors in children. Three main groups of tumors are found in this area: pineal tumors proper (pinealoblastoma and pineocytoma), accounting for 17%, germ cell tumors, diagnosed in 40-65% of cases, and glial tumors, found in 15% of tumors of this localization. Parenchymal pineal tumors are more common in children in the first decade of life, germ cell tumors are more often diagnosed in adolescents, predominantly boys. Astrocytomas of this localization have two age peaks: 2–6 years and the period from 12 to 18 years.
Pinealoblastoma is an embryonal tumor of the epiphysis tissue. This is a highly malignant tumor. Its histological characteristics are similar to PNET and medulloblastoma. Its biological behavior is similar to medulloblastoma, i.e. it tends to seed the spinal canal early and spread beyond the central nervous system. Bone, lungs, and lymph nodes are the most common sites of metastasis.
Germ cell tumors arise in the brain due to pathological migration of germ cells during embryonic development. Histologically, this heterogeneous group, including germinomas, endodermal sinus tumors, embryonal carcinomas, choriocarcinomas, mixed cell germ cell tumors, and teratocarcinomas, is virtually indistinguishable from “classical” germ cell tumors. If a germ cell tumor is suspected, it is necessary to determine the level of alpha-fetoprotein (AFP) and beta-human chorionic gonadotropin (HCG) in the cerebrospinal fluid and blood serum. Elevated levels of AFP and HGT are detected in embryonal cell carcinomas or mixed cell germ cell tumors. An increased content of only hCG is characteristic of choriocarcinomas. Although germinomas are more often negative in relation to these markers, a number of studies emphasize that 1/3 of patients with germinomas have an increased level of hCG, although its level is significantly lower than in patients with choriocarcinoma. In all patients with non-germ tumors of the pineal region, these tumor markers are not detected. These tumors (especially choriocarcinomas and yolk sac tumors) have the appearance of large infiltrating formations that early disseminate along the spinal canal and in 10% of cases metastasize beyond the central nervous system (to bones, lungs, lymph nodes).
Since the histological type of pineal tumor has prognostic significance, verification of the diagnosis is necessary, if possible. Germinomas and astrocytomas (usually low grade) have a better response to therapy and a better prognosis. Teratomas and true pineal tumors have a less favorable outcome. The worst prognosis is for patients with non-germ cell tumors, which are characterized by rapid progression, leading to death within a year from the date of diagnosis.
Radiation therapy is the main treatment for pineal tumors. The standard approach for germ cell tumors and pineablastomas is craniospinal irradiation with local dose escalation, as used for medulloblastomas. This group of tumors has a high sensitivity to RT.
If it is impossible to histologically verify the tumor in this area and there are negative markers of germ cell tumors, ex juvantibus radiation therapy is used as the treatment of choice: local irradiation at a dose of 20 Gy and, if the dynamics are positive (which will indicate the malignant nature of the tumor), expanding the irradiation field to craniospinal irradiation. If there is no response to radiation therapy, only local radiation followed by an attempt at exploratory surgery is recommended.
The absence of a blood-brain barrier in the pineal region and the success achieved in the treatment of germ cell tumors outside the central nervous system have led to the fact that the use of classical chemotherapy regimens, including platinum drugs, vinblastine, VP-16 and bleomycin, makes it possible to achieve complete or partial remission. Pineal parenchymal tumors are sensitive to platinum and nitrosourea. Pineacytoma and gliomas of this localization are treated according to the regimens used for similar tumors of other localizations.
Craniopharyngiomas account for 6-9% of all central nervous system tumors in children, the average age at diagnosis is 8 years. They are most often localized in the suprasellar region, often involving the hypothalamus, but can also occur within the sella turcica.
These are rather slow-growing tumors, histologically of low malignancy, often containing cysts. Malignant behavior of craniopharyngiomas with infiltration of surrounding normal structures is rarely described. Examination often reveals calcifications in the tumor. In the clinical picture in 90% of patients, along with the typical symptoms of increased ICP, neuroendocrine deficiency dominates: most often there is a deficiency of growth hormone and antidiuretic hormone. 50-90% of patients experience visual field impairment.
The prognosis of such patients largely depends on the completeness of tumor resection. If radical removal is not possible, the method of choice may be aspiration of the contents of the cysts, but one must keep in mind that patients with a non-radically removed tumor in 75% of cases have a relapse of the disease within the first 2-5 years. RT may reduce the incidence of relapse in patients with incomplete tumor removal or after cyst drainage. Local irradiation is usually used at a dose of 50-55 Gy, which, according to Japanese scientists, can provide a cure rate of up to 80%. The role of chemotherapy in patients with craniopharyngiomas is unclear due to very limited published data.
Meningiomas.
These tumors are rare in young children and are more common in teenage boys. They are usually localized supratentorially, affecting the cerebral hemispheres and lateral ventricles. Multiple meningiomas can occur in patients with Recklinghausen disease. Due to their location, these tumors are usually resectable and therefore do not require further treatment.
Choroid plexus tumors account for 2-3% of all brain tumors in children. In children under 1 year of age, these tumors occur in 10–20% of cases. Up to 85% of these tumors are localized in the lateral ventricles, from 10 to 50% in the fourth ventricle, and only 5 to 10% in the third ventricle. Most often, these tumors arise as functioning intraventricular papillomas that secrete cerebrospinal fluid. These tumors grow rather slowly and, due to their intraventricular location, often reach a large size (weighing up to 70 grams) by the time they are detected. In 5% of cases, tumors can be bilateral.
Choroid plexus carcinoma is a more aggressive tumor, accounting for 10–20% of all choroid plexus tumors. This tumor exhibits features characteristic of anaplastic tumors and has a propensity for diffuse, aggressive extracranial spread. Although papillomas of the choroid plexus can spread beyond the skull, their deposits are benign and, as a rule, are asymptomatic.
The main treatment method for these tumors is surgery. Complete tumor removal is possible in 75-100% of patients with papillomas, which ensures their cure. Other treatment methods are not indicated for patients with choroid plexus papillomas. In case of tumor recurrence, repeated surgery is possible.
Patients with choroid plexus carcinoma after surgical resection of the tumor should receive RT, although the main prognostic factor in such patients is the completeness of tumor resection.
In small series of patients, a positive effect was shown from the use of preoperative chemotherapy, consisting of ifosfamide, carboplatin and VP-16, in order to reduce the size of tumor vascularization.
SPINAL CORD TUMORS
These tumors are much less common than brain tumors. Clinical manifestations of the disease depend on the level of damage and the rate of tumor growth. Movement disorders, lameness, other gait abnormalities, and back pain are symptoms characteristic of these tumors. Localization of the tumor in the sacral segments causes dysfunction of the bladder and intestines.
Lymphomas and neuroblastomas, sometimes arising in the spinal canal, are treated according to appropriate programs. Approximately 80-90% of primary spinal cord tumors are gliomas. Less common are ependymomas and PNETs. Approximately half of gliomas are low-grade and the best treatment for them is currently unknown. Two approaches are being studied: wide resection or less aggressive surgical tactics followed by local irradiation. Local irradiation is indicated for children with rapid tumor progression and worsening neurological symptoms. Anaplastic gliomas of the spinal cord have a worse prognosis due to rapid dissemination along the spinal canal already at the onset of the disease. In the treatment of these patients, craniospinal irradiation and adjuvant polychemotherapy (vincristine, lomustine, platinum drugs) are used.
The prognosis for children with central nervous system tumors is determined primarily by the degree of radicality of tumor removal, its histological structure and the adequacy of postoperative treatment (volume and dose of radiation therapy, chemotherapy). Recently, megadose chemotherapy regimens followed by autologous transplantation of peripheral stem cells have been introduced into the treatment program for highly malignant brain tumors, such as medulloblastoma and PNET, high-grade gliomas, and pineoblastoma.
Careful monitoring of patients with tumors of the central nervous system should include, in addition to regular neurological examinations, a number of instrumental examinations. The frequency of necessary examinations (CT, nuclear MRI, cerebrospinal fluid examination, etc.) depends on the type of tumor and the degree of initial spread. Early detection of disease relapse by CT or nuclear MRI (before the development of clinical symptoms) makes it possible to timely resume specific therapy. Unfortunately, many children cured of brain tumors subsequently have intellectual, endocrine and neurological problems, both as a result of the tumor itself and the therapeutic effects that were used on the child. Therefore, in addition to the oncologist, these children should be observed by an endocrinologist, a neurologist and a psychologist or psychiatrist.
Page 187
Deterioration and various visual impairments
Andrey Levashov, pediatric oncologist, candidate of medical sciences, researcher at the department of chemotherapy of hemablastosis with the neuro-oncology group of the National Medical Research Center of Oncology named after. N.N. Blokhina:
“A symptom of a brain tumor is often rapid deterioration of vision. A child may complain of various disturbances: the flickering of midges or the appearance of multi-colored highlights and stripes in front of the eyes, loss of visual fields from different sides - that is, when he ceases to see with peripheral vision, loss of central visual fields - when the child’s gaze is constantly directed to the side. It is also possible to develop photophobia (photophobia) - painful sensitivity of the eye to light.
There are a number of other symptoms of a brain tumor that should be cause for concern. These are increasing nystagmus, that is, rapid movement of the eyeballs from side to side or up and down, diplopia (double vision), exophthalmos (protrusion of the eyeball outward), ptosis (drooping of the upper eyelid so that the eye is constantly in a half-closed state). Also, with brain tumors, strabismus may develop, and sometimes the pupils begin to differ in size. The child may be bothered by pain in the projection of the eye: in this case, he will say that the eye hurts somewhere deep, something is pressing on it.
It can be difficult for parents of young children to notice visual impairment in their child. Young children cannot complain, so parents need to closely monitor their behavior. For example, if a son or daughter used to assemble a construction set, but now cannot, or if they suddenly have difficulty picking up an object that was not there before, this may indicate vision problems.
If you experience any of these symptoms, you should immediately contact your pediatrician and ophthalmologist. Next, a comprehensive examination should be carried out, including an MRI of the brain with intravenous contrast. The most important thing is timely diagnosis; it is better not to delay treatment.”
Bone tumors
They account for 6% of all malignant tumors in children. 1 child per 100,000 people gets sick. It mainly affects children 12-17 years old.
The most common are osteogenic sarcoma, Ewing's sarcoma, and synovial sarcoma.
Main symptoms: swelling, pain, impaired movement.
Osteosarcoma is most often localized in the knee joint, affecting the femur, tibia, and humerus. X-ray picture: “visor” symptom (detachment of the periosteum) and needle periostitis. Ewing's sarcoma most often affects the fibula, femur, pelvic bones, and vertebrae. X-ray picture: bulbous periostitis.
For early diagnosis of the disease it is necessary to:
- CT, MRI of the affected limb;
— RCT of the chest organs;
— Scintigraphy of bones and soft tissues.
— Puncture, open biopsy of the tumor.
— Bone marrow puncture.
After the diagnosis is established, complex treatment is carried out: preoperative chemotherapy, surgery (the most important is the radicality of the operation), radiation therapy for Ewing's sarcoma, postoperative polychemotherapy. Predominantly, safe operations are performed - endoprosthetics. In some cases, mutilation is amputation.
Ringing in the ears, hearing loss, noticeable tilting of the head or curvature of the neck, dizziness
Andrey Levashov, pediatric oncologist, candidate of medical sciences, researcher at the department of chemotherapy of hemablastosis with the neuro-oncology group of the National Medical Research Center of Oncology named after. N.N. Blokhina:
“Symptoms of a brain tumor can also include hearing impairment. The child begins to hear worse, or he develops hypersensitivity to sound: you talk to him quietly, but it seems to him that it is very loud. Ringing in the ears can also be bothersome, often only on one side. With all these symptoms, the pediatrician, of course, can refer you to an ENT doctor, but if he rules out pathology of the ENT organs, then this is a direct route to a neurologist.
Another symptom from the ENT organs is a constant cough. It's not wet or long-lasting: I'd say it's more of a cough. In this case, they usually first contact an ENT doctor. If it excludes colds, then the child begins to suspect allergies. But allergic cough usually depends on seasonality and worries in the spring and summer, when there are a lot of allergens around. It may also depend on the presence of food, drug allergies, or allergies to pet hair. If the child’s living environment and diet have not changed, and if he has not taken medications, then a cough should cause concern.
When the tumor is located in the cervical region or the transition of the brain stem to the spinal cord, the child sometimes experiences a tilt of the head to the side or a curvature of the neck. But usually this is not the key symptom; it is combined with something else.
It is necessary to mention dizziness. If they bother your child regularly, if he complains about them, even when he’s just sitting or lying down, you need to go to the pediatrician. First, he will prescribe a general blood test, and if no signs of anemia are detected, he will refer you to a neurologist. Sometimes this symptom can also indicate dysfunction of the heart muscle or thyroid gland: in this case, a cardiologist and endocrinologist will be involved.”
What are the most common brain tumors in children?
- glioma;
- glioblastoma multiforme;
- tumor of the posterior cranial fossa;
- medulloblastoma;
- pilocytic astrocytoma;
- ependymoma;
- brainstem glioma;
- metastatic lesions.
Each has its own characteristics and is diagnosed by a specialist depending on the symptoms, examination results and tests.
More information about neurosurgery at the Odrex Medical House can be found on the website. You can make an appointment with Konstantin Anatolyevich Kardash by calling +38 or using the “Make an appointment” form on our website.
Developmental delay, developmental regression, increased head circumference
Olga Zheludkova, pediatric oncologist, Doctor of Medical Sciences, Professor of the Russian Scientific Center of Radiology:
“In young children, up to two years old, a brain tumor, as a rule, does not manifest itself in any way. And the only symptom is an increase in head size. Therefore, parents should pay attention to this, and if they notice that the head circumference continues to increase rapidly, they need to go to the pediatrician and tell them about it. Also, a manifestation of the tumor process can be a reverse development: when the child developed and gained weight up to six months, everything was normal, but after six months of age he ceases to be interested in the world around him and objects, stops sitting and walking, and holding his head up. Although he eats well, for example. This could also be a symptom of a brain tumor."
Recorded by: Liza Kofanova, Victoria Vyakhoreva
What are the main causes of tumors in children?
Some tumors are hereditary. For example, one of the common genetic diseases treated by neurosurgeon Konstantin Kardash is neurofibromatosis (Recklinghausen disease).
The mechanisms of development of brain tumors in children are not fully understood; presumably, these are radiation, hormonal imbalances, viral infections and environmental factors that are considered carcinogenic. We only know for certain that the cause of tumor development is radiation - this has been confirmed by scientific research.
Unfortunately, many carcinogens are found in everyday life. Of course, this is not a reason to abandon the basic benefits of civilization, but they must be used consciously:
- high voltage power lines,
- electromagnetic radiation from mobile communications,
- sweetener (aspartame),
- gas used in the production of plastics (vinyl chloride).