Common factors that provoke the development of this pathology also include:
- High body weight. It leads to an increase in mechanical and shock-absorbing loads on the joints of the bones.
- Pregnancy. In the later stages, if you do not follow the recommendations of your doctor, divergence of the pelvic bones may appear.
- Pathologies of cartilage and bone tissue. This may be the occurrence of bone growths, stretching of the joint capsule and a number of similar problems.
- Bad habits. Inflammation often manifests itself against the background of heavy smoking, drinking alcohol, or ingesting heavy metal salts.
- Problems with blood supply. They can arise due to varicose veins, atherosclerosis and a number of other factors.
- Traumatic impact. In addition to the injuries listed above, the pathology can be caused by bruises with the formation of internal hematomas, microscopic ruptures of tendons and fascia, and other injuries that may be invisible to the naked eye.
Therapeutic procedures will be aimed at achieving the following goals:
- preventing the inflammatory process;
- eliminating pain syndrome;
- normalization of blood circulation in the joint;
- preventing further destruction of cartilage tissue.
Treatment of the hip joint in the “Health Workshop” relieves muscle spasm, pain and inflammation in the joints, normalizes the nutrition of the cartilage and accelerates its recovery. Therapeutic procedures activate blood circulation and improve overall well-being.
After completing the course, our doctor will give the patient a manual with joint gymnastics exercises to perform independently at home. The doctor will advise what else to do to prevent the disease.
Drug treatment
Drug therapy for this pathology varies greatly depending on what was the root cause of the disease. to treat hip joint pain :
- Glucocorticoids. Prescribed for severe intoxication.
- Antibacterial agents. They are used if it has been established that the cause of the disease is an infectious effect. Fluoroquinolones, macrolides or tetracyclines are commonly used.
- Muscle relaxants. Used if you need to reduce muscle spasm.
- Immunosuppressants. They are used if the cause is reactive arthritis or psoriasis. Often, the doctor prescribes their use in conjunction with folic acid.
- Non-steroidal anti-inflammatory drugs. Help reduce the inflammatory response.
- Chondroprotectors. They stimulate the restoration of cartilage tissue and stop the development of degenerative processes.
- Vitamins and immunostimulants. Used as maintenance treatment.
All of these medications (and a number of others) can be used exclusively as prescribed by the attending physician. Independent choice of drugs can lead to aggravation of the situation and the emergence of health problems.
Causes of pinched nerve of the leg in the hip joint
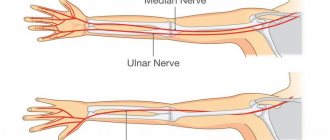
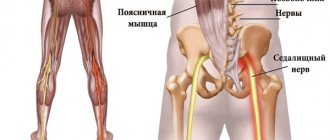
First, let's look at pinching of the sciatic nerve in the hip joint, since this condition is often accompanied by loss of ability to work and provokes severe pain. This pathology is not always associated with damage to the hip joint. It is not correct to think that compression occurs in the cavity of the bone articulation. In fact, the pinching of the sciatic nerve occurs in the piriformis muscle tunnel. It starts at the sacrum and ends at the hip joint. Inside it passes the sciatic nerve and blood vessels that provide its nutrition.
Leg entrapment in the hip joint in relation to the sciatic nerve is in most cases associated with piriformis tunnel syndrome.
The causes of pinching of the femoral nerve in the hip joint may be as follows:
- deforming osteoarthritis of the hip joint;
- unstable position of the femoral head and its periodic displacement;
- sprain of the ligaments and their subsequent scar deformation, which provokes pressure on the nerve fiber;
- ruptures of the ligament and tendon fibers, the formation of hematomas in the areas where the femoral nerve passes;
- calcification of muscle fiber and its scar deformation;
- proliferation of osteophytes in the area of the acetabulum of the ischium;
- fractures, including those of the femoral neck;
- bone tissue cracks;
- all types of dislocations and subluxations;
- dysplasia of the cartilage tissue of the hip joint;
- pelvic bone distortion, short limb syndrome and spinal column deformity;
- osteochondrosis of the lumbar spine, aggravated by muscle fiber tension in the sacral, femoral and gluteal regions.
In addition, a pinched nerve in the hip joint can be caused by rheumatic pathologies of its tissues. More often than others, the articular form of ankylosing spondylitis and systemic lupus erythematosus are diagnosed. Rheumatoid polyarthritis and scleroderma are less common. One should also not exclude the possibility of developing tumors, including cancer, and infectious processes that cause infiltrative swelling of soft tissues and compression of nerve fibers.
Rehabilitation after surgery
Most often, non-surgical methods help cure inflammation of the hip joint. However, if there is severe pain or stiffness in the joint, surgery is necessary. We do not perform hip surgery.
If you have had surgery on a joint, you need to begin a rehabilitation course within a few days. This course can be taken at the Health Workshop network of clinics in St. Petersburg. Our doctors will create a set of procedures for the patient that will strengthen the body, restore mobility to the operated joint and consolidate the positive effect of the operation.
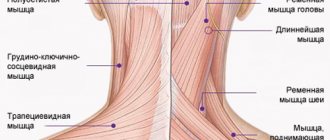
Pudendal neuralgia
Neuralgia (neuropathy) of the pudendal nerve (syn. pudendal neuralgia, pudendal neuropathy, pudendal neuralgia) is one of the causes of chronic pelvic pain. Develops when the pudendal nerve is damaged, compressed or irritated. The main symptom is pain in the anus, perineum, external genitalia, aggravated by sitting.
The pudendal nerve (syn. pudendal nerve) is one of the main pelvic nerves. It innervates the following areas:
- anorectal (anus area);
- crotch;
- external genitalia.
The pudendal nerve can be affected in several places as it passes through the pelvis:
- when exiting the greater sciatic foramen under the piriformis muscle (rarely);
- in the area of the ischial spine in the space between the sacrospinous and sacrotuberous ligaments (most often - 70% of cases);
- in the area of the Alcock canal (syn. Genital canal) - between the layers of the fascia of the obturator internus muscle (20% of cases).
Genital neuralgia (neuropathy) occurs in both women and men.
Pudendal nerve
Genital neuralgia develops when the pudendal nerve is damaged, compressed, or irritated.
Possible reasons:
- prolonged sitting;
- with some types of sports activity: cycling, horse riding. When performing certain exercises, such as deadlifts, squats with heavy weights;
- for chronic constipation;
- after surgical operations on the pelvic organs;
- for fractures of the pelvic bones;
- nerve injury during childbirth;
- genital herpes (postherpetic neuralgia);
- for benign and malignant neoplasms (tumors) in the immediate vicinity of the pudendal nerve.
In many cases, the cause cannot be identified.
Currently, when making a diagnosis, doctors use the so-called Nantes criteria (adopted by a multidisciplinary working group in the French city of Nantes in 2006). There are 5 main (mandatory) symptoms:
- Pain in the area of innervation of the pudendal nerve (from the anus to the external genitalia, including the perineum).
- The pain predominantly occurs in a sitting position. At the same time, sitting on the toilet does not cause pain.
- The pain does not bother me at night. If the patient complains of pain during the night, then an examination is necessary to exclude compression of the pudendal nerve by the tumor.
- Absence of objective sensitivity disorders. This is explained by the fact that the innervation zone of the pudendal nerve overlaps with other nerves (for example, the posterior cutaneous femoral nerve, etc.). If sensory disorders are detected, it is necessary to exclude damage to the sacral nerve roots (for example, a herniated lumbar intervertebral disc) or the sacral nerve plexus.
- The pain goes away with a diagnostic block of the pudendal nerve.
Additional criteria:
- Burning, shooting, stabbing pain; feeling of numbness (characteristics of neuropathic pain).
- Intolerance to tight (tight-fitting) clothing and underwear.
- Sensation of a foreign body in the rectum or vagina.
- Pain worsens during the day (in the evening).
- Predominantly unilateral pain. Bilateral pain does not exclude the diagnosis.
- The pain is provoked by defecation (most often not immediately, but after a few minutes).
- Increased sensitivity to palpation in the ischial spine during digital rectal or vaginal examination.
- Neurophysiological data.
Additional symptoms that are not directly related to damage to the pudendal nerve, but do not exclude the diagnosis of pudendal neuralgia:
- Pain in the gluteal region when sitting (possibly associated with spasm of the piriformis muscle, under which the pudendal nerve passes; or spasm of the obturator internus muscle).
- Referred pain along the sciatic nerve.
- Pain along the inner surface of the thigh (along the obturator nerve).
- Pain in the suprapubic region (associated with spasm of the levator ani muscle).
- Frequent urination.
- Pain after ejaculation.
- Pain after intercourse.
- Erectile disfunction.
The diagnosis is established by exclusion: it is necessary first of all to exclude diseases of the pelvic organs and abdominal cavity, which may require consultation with a gynecologist, urologist, proctologist, and additional studies (MRI, ultrasound, MSCT).
- Modification of motor activity. Avoid activities that cause pain: cycling, horse riding, squats, etc. Limit sitting and take breaks more often. Sit on ring-shaped or semicircular pillows. Sit while maintaining lumbar lordosis (use bolsters under the lower back).
- Treatment of constipation.
- Physical therapy (physical rehabilitation): exercises for the pelvic floor muscles and other pelvic muscles (Kegel exercises, for example), stretching, myofascial release, yoga, etc.
- Drug treatment. The following drugs can help: non-steroidal anti-inflammatory drugs, centrally acting muscle relaxants (drugs that relax muscles), gabapentinoids (pregabalin, gabapentin). For severe pain, use opioids. The dosage and duration of use is determined by the doctor individually.
- Pudendal nerve blocks. The nerve block is performed under the guidance of ultrasound, x-ray or computed tomography. In our clinic, it is possible to use all three types of control, but preference is given to the computed tomography method, as the most accurate and safe. To carry out the blockade, local anesthetic drugs (lidocaine, bupivacaine, etc.) and glucocorticoids in the form of a suspension (drugs with pronounced anti-inflammatory and decongestant effects) are used. During the blockade, hydrodissection is also performed - creating additional space around the nerve by injecting fluid (anesthetic or saline). Typically three blocks are performed at intervals of four weeks.
The moment of performing a nerve block under MSCT control.
Such complex treatment (physical therapy, medications, blockades) is effective in most patients. If it is ineffective or the pain syndrome recurs, pulsed radiofrequency therapy of the nerve is indicated.
Currently, the possibilities of using hyaluronic acid and botulinum toxin preparations for the treatment of sexual neuropathy are also being studied.
Prevention
Doctors at the Health Workshop give the following recommendations for preventing joint inflammation:
- swim, walk more, get stronger;
- do not overload or overcool the joints;
- treat infections in a timely manner, do not endure them “on your feet”;
- drink at least 1.5 liters of water per day;
- watch your weight and posture, don’t slouch;
- do not drink alcoholic beverages or smoke;
- limit the consumption of sugar and salt, carbonated drinks;
- monitor the level of uric acid in the body;
- eat more dairy products, fruits, vegetables;
- include fatty fish, jellied meat, jelly and other products with gelatin in your diet.
How to treat a pinched nerve in the hip joint
Before treating a pinched hip nerve, it is necessary to conduct a differential diagnosis. To do this, you need to visit a neurologist. Before treating a pinched nerve in the hip joint, he will perform a manual examination and a series of diagnostic tests. With this, he will be able to make a preliminary diagnosis. Next laboratory tests are prescribed:
- an x-ray of the hip joint and the lumbosacral spine will eliminate the possibility of injury, proliferation of osteophytes, development of deforming osteoarthritis, etc.;
- electromyography to exclude muscle fiber pathology;
- electroneurography to clarify the condition of the nerve fiber;
- MRI – shows the condition of ligaments, tendons, muscles, cartilage and nerve tissue in real time;
- Ultrasound of the internal organs of the abdominal cavity to eliminate the risk of developing tumor processes that put pressure on the nerves.
The first thing to do if a nerve is pinched in the hip joint is to avoid physical activity and ensure rest until you see a doctor. Second, make an appointment with a neurologist. Third, lie on your back and try to relax overly tense muscles. Often this allows you to relieve the spasm for a while and ensure safety for the pinched nerve.
Hip impingement can be treated using different methods. We will consider the most effective of them later in the article.