Therapy of vegetative-vascular dystonia is a complex and lengthy process.
It is sometimes difficult for such patients to choose a truly effective remedy. Grandaxin for VSD helps eliminate the alarming symptoms of this complex, as well as other neurological disorders. The medicine is a relatively new product on the pharmaceutical market, but has already managed to prove itself on the positive side.
Description
Grandaxin is an anxiolytic drug or tranquilizer. Produced in 50 mg tablets. They have a round and flat shape, the color range varies from white to grayish. On one side there is a dividing line, on the other there is the Grandax logo.
The tablets are placed on a blister that holds 10 tablets. There are 2 or 6 pieces in a package.
The active substance of Grandaxin is represented by tofisopam. It is obtained by an atypical chemical modification of the diazepam molecule. Tofisopam belongs to the group of benzodiazepines and exhibits the properties of tranquilizers, but has some peculiarities.
How psychotherapy helps in treating panic attacks
Psychotherapy is a reliable way to get rid of panic attacks. The psychotherapist will not somehow calm you down, but on the contrary, in fairly energetic work with the patient, he will help you understand the reasons and teach you self-regulation techniques.
Treating panic attacks takes time and can take anywhere from a month to two. Considering the patient’s condition, he is offered various treatment methods. Recommendations for lifestyle changes may be given, mostly of a general nature. Mode of activity, nutrition and physical activity partially influence panic states, so the doctor may recommend getting enough sleep, eating regularly, spending more time outdoors and, of course, exercising and yoga. It is recommended to stop watching TV and news, and reduce the amount of caffeine-containing drinks to a minimum. Avoiding alcohol is also recommended.
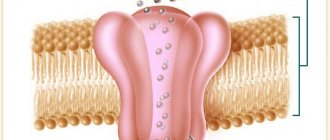
Tranquilizers and Grandaxin
Tranquilizers are identical to the concept of anxiolytics. Translated from Latin, anxietas means fear or anxiety, and litikoc from ancient Greek means weakening. Thus, tranquilizers are designed to relieve anxiety.
Anxiolytics are called minor tranquilizers, while antipsychotics are classified as major tranquilizers. Most of them exhibit 5 main effects:
- anxiolytic - elimination of emotional stress, obsessive thoughts and fears, reduction of anxiety;
- sedative - removal of psychomotor excitability, slowing down activity, speed of reactions, both mental and motor. Decreased concentration;
- sleeping pills - normalization of sleep, increasing its depth;
- muscle relaxant - muscle relaxation. May be accompanied by lethargy, weakness, slow reaction, excessive relaxation;
- anticonvulsant - reduction of excitation in epileptoid foci of the brain.
Grandaxin is also a representative of tranquilizers. However, it does not exhibit a pronounced sedative, muscle relaxant and anticonvulsant effect, but has mainly an anti-anxiety effect.
“Physiological” or “mental” depression: how to determine the cause of the disease
The first thing to remember is that panic attacks do not appear out of the blue; there is always a reason for their “awakening”. If a person does not have an innate predisposition to a depressive state, there have been no significant events in life that “knocked him out of the rut”, in 90% of cases we are talking about problems with the physical state of vital systems - cardiovascular and circulatory. The cause of uncontrollable panic and reluctance to enjoy life in the case of osteochondrosis is degeneration of vertebral cartilage in one form or another, which leads to disruption of the functioning of surrounding nerve roots and blood vessels. The resulting protrusions, hernias or other damage to the intervertebral disc lead to compression of the vessels providing blood supply to the brain. In 60% of cases, “advanced” osteochondrosis leads to oxygen starvation of the brain. Trying to normalize its condition, the “main organ” gives alarming signals, including those of a psychological nature.
How the drug works
When treated with Grandaxin, there is no drowsiness or lethargy. Moreover, it moderately increases mental and motor activity, stimulates mental activity, and provides a surge of strength and energy.
The drug does not cause muscle relaxation, eliminates the feeling of fatigue and increases performance. It returns sound and healthy sleep, but there is no lethargy or drowsiness during the day. In general, this drug does not have the side effects that are inherent in many tranquilizers.
Taking Grandaxin for VSD provides a vegetative stabilizing effect.
Our autonomic system regulates the activity of internal organs, as well as blood vessels. It consists of the sympathetic and parasympathetic divisions. If the balance in their work is disturbed, there is, accordingly, a failure in the regulation of the work of those systems for which they are responsible. Such violations can manifest themselves in different ways:
- tachycardia, pain and compression in the heart area;
- difficulty breathing, shortness of breath, feeling of lack of air;
- feeling of a lump in the throat;
- sweating, low-grade fever;
- redness of the skin, feeling of heat;
- headache, dizziness;
- asthenia, malaise;
- fear of death or concerns about one's health.
A similar symptom complex is a manifestation of vegetative-vascular dystonia.
Grandaxin helps to establish a synergistic effect of both parts of the autonomic nervous system, eliminates most symptoms of VSD, relieves apathy, anxiety, phobias and obsessive thoughts.
What are the symptoms of panic attacks?
The condition that occurs during fear is associated with the release of adrenaline into the blood. It is he who triggers the biological reaction to the threat, as we wrote - prepares for fight or flight. Changes occur in the functioning of the heart, lungs, kidneys, blood vessels, which are felt as symptoms of panic attacks, here are the most common:
- Feeling of fear, experiencing a threat to life
- Rapid heartbeat
- Difficulty breathing frequently, there may also be a “lump in the chest”
- Feeling hot or, conversely, becoming cold and shaking
- Blood vessels can spasm, causing headaches
The patient may breathe rapidly, complain of palpitations, “the heart is jumping.” Within an hour the symptoms subside. If panic attacks recur, they usually seek help from a psychotherapist or psychologist. Panic attacks can indicate an anxiety disorder or depression, or even physical illness. If a person experiences panic in a particular context repeatedly, phobias associated with those specific circumstances arise. The symptoms of a panic attack are themselves a source of stress and can come in waves. Despite the very unpleasant symptoms, panic attacks can be successfully treated.
Other indications
Grandaxin is effective not only for VSD, but also for neuroses, as well as other similar conditions. Indications include:
- alcohol withdrawal;
- premenstrual, menopausal period;
- mental maladjustment;
- mild depression;
- conditions accompanied by muscle asthenia and atrophy, when muscle relaxant anxiolytics are unacceptable for use.
The drug is a daytime tranquilizer. It does not cause addiction or withdrawal symptoms.
An important property of Grandaxin is the relief of panic attacks. This is a feeling that occurs suddenly or under the influence of a stressful situation. Accompanied by a strong feeling of fear and vegetative disorders.
The concepts of VSD and panic attack are closely related: the attack is a kind of exacerbation of neurocirculatory dystonia. Therefore, therapy for these conditions follows a similar plan.
Categories
There are two types of classifications of PA (panic attacks). For reasons of occurrence:
- situational. The feeling of horror, as well as other symptoms, appear only in a certain situation, which has a negative impact on the person and his body as a whole;
- spontaneous. Can occur at any time, regardless of place, time or emotional state at the current moment;
- conditional-situational. It only appears when exposed to chemicals. For example, alcohol or tobacco.
By VSD type:
- hypotonic type. It is characterized by sweating, decreased blood pressure, shortness of breath, nausea and body weakness;
- hypertensive. In this type, the most common symptoms are rapid heartbeat, rapid pulse and increased blood pressure;
- mixed. The patient experiences two types of panic attacks at once during VSD.
Features of use
Grandaxin is taken 1-2 tablets 1 to 3 times a day. The course of treatment is based on the severity of the manifestations and is prescribed exclusively by a doctor. A maximum of 300 mg of the drug per day is allowed.
Like any medicinal component, Grandaxin can lead to adverse reactions and intolerance by the body. They are manifested by the following violations:
- allergic rash and itching;
- pain and increased muscle tone;
- labored breathing;
- irritability and agitation, sleep disturbance, clouding of consciousness, headaches, exacerbation of epilepsy.
In case of an overdose of the drug, the development of a coma and breathing problems, depression of the central nervous system is possible.
Grandaxin should not be used for obsessive states and persistent psychoses. This will lead to a suicide attempt and increased aggression.
If you are allergic to lactose, the drug is also contraindicated, since each tablet contains about 90 mg of this substance.
The drug is not prescribed for respiratory disorders.
The drug should not be prescribed in the first 3 months of pregnancy and during breastfeeding.
The drug is prescribed with caution to patients with epilepsy, personality disorders and organic damage to the central nervous system, as well as elderly people, patients with mental retardation and decreased kidney function.
When the drug enters the intestines, it is quickly absorbed. Its highest concentration in the blood appears after a few hours. The active ingredient is not concentrated in the body. Most of it is excreted in urine, and a small amount is excreted in feces.
Grandaxin has some peculiarities of contact with other drugs. Its combination together with certain immunosuppressants (tacrolimus), as well as with cyclosporine, increases their accumulation in the blood.
Grandaxin enhances the intensity of the action of psychotropic drugs: sedatives, hypnotics and antidepressants.
In turn, its intensity of impact is increased by antihypertensive drugs, and accumulation in the blood is intensified by antimycotic drugs.
The combined use of Grandaxin and antacids reduces its absorption.
Anxiolytic mitigates the toxic effects of alcohol-containing drinks on the central nervous system. But its parallel use with these liquids, barbiturates, antiepileptic drugs, nicotine reduces its effectiveness.
How can a specialist help with depression?
Depression, especially spontaneous depression, is not a reason to make an appointment with a psychiatrist. Start with something simple - a visit to a therapist. A thorough visual inspection will tell a good specialist a lot. The doctor’s goal is to make a correct diagnosis, on which 90% of the effectiveness of treatment depends. If there is a suspicion of osteochondrosis and the symptoms are associated specifically with this pathology, a laboratory study of blood biochemistry and ultrasound of the vessels of the cervical spine are recommended. After studying the results, it will be possible to decide what caused the panic attack and depression. Treatment is prescribed in accordance with the physical and psychological condition of the patient and is carried out comprehensively. The goal is to simultaneously normalize blood flow in narrowed vessels and relieve a person from emotional exhaustion. Therapeutic measures can be different: taking medications to improve brain function, physiotherapy, prescribing sedatives or antidepressants.
Classification of attacks
Modern psychotherapy identifies three main categories of panic attacks:
- Spontaneous attacks. They are characterized by unexpected development and arise in a situation in which the patient feels comfortable. The spontaneous attack usually occurs first, then most patients attribute symptoms to specific places, situations or circumstances.
- Situational attacks. They arise in a certain situation or when waiting for a long time for this situation.
- Conditional-situational attacks. They are provoked by factors of a biological nature: drinking alcohol, coffee, hormonal changes. However, this connection is rather arbitrary and difficult to trace. Often a panic attack that occurs under the influence of a chemical stimulus later turns into a situational one.
- Chemically provoked attacks. Separately, panic attacks are distinguished that first occurred under the influence of psychoactive (narcotic) substances - ecstasy, LSD, “speed”, “spice”, cannabis (marijuana), psilobiscins (“narcotic mushrooms”). As a rule, such a panic attack is atypical (it contains vivid experiences of depersonalization with fear of losing control over oneself and a feeling of change and loss of one’s own personality), and concomitant autonomic disorders can be either very pronounced or not expressed at all. Often, after such a panic attack, even once suffered, a persistent fear for one’s health develops, so pronounced that daily functioning is markedly and persistently reduced - so much so that the person is practically unable to work.
It is important to understand the cause for treatment to be successful.
Symptoms
The symptoms of a panic attack can vary from person to person. This is due to the fact that symptoms are the results of the human body’s struggle with unexpected chemical processes, and exactly how this struggle will manifest itself depends on the individual characteristics of the person. During a panic attack, you may experience difficulty breathing (a feeling that your throat is swelling), rapid heartbeat, and pulsating blood in your temples. A person may feel sick, feel either hot or cold, or feel uncontrollable trembling. But in the end, the most difficult feeling is a feeling of sudden and overwhelming fear or panic.
How to treat panic attacks and when to see a specialist
It is necessary to contact a specialist if you have recurring panic attacks. Therapy is selected individually and, as a rule, includes psychotherapeutic work and drug therapy. Psychotherapy involves various techniques aimed at recognizing and understanding the causes of problems, teaching ways to deal with the symptoms of the disease, and relaxation methods. Psychotherapy can take place in the form of individual meetings with a psychotherapist or in the form of group sessions with other patients. Drug therapy for panic disorder is carried out with various drugs that help reduce the level of anxiety and fear. Prescription, dosage adjustment and discontinuation of treatment must be carried out under the supervision of a physician.
Modern neurotechnologies can also help in the treatment of panic attacks. Methods of neurofeedback training have been developed for patients with panic disorder. During the trainings, patients learn to manage their emotional state, they form new neural connections, and their anxiety level decreases. In addition to professional help, lifestyle plays a significant role in the treatment and prevention of panic attacks. Try not to abuse alcohol and caffeine, get more rest, go in for sports, preferably yoga.
Source: https://www.wmj.ru/krasota/telo/golovokruzhenie-zhar-i-dazhe-udushe-simptomy-panicheskikh-atak-i-kak-s-nimi-borotsya-razbiraem-s-vrachom.htm
Back to list
According to the Federal State Statistics Service, currently the average life expectancy of women in Russia is 76.3 years. The average age of menopause is 50-53 years, so a woman spends almost ⅓ of her life in a state of hypoestrogenism. At the same time, a significant proportion of women have vasomotor manifestations of menopause to varying degrees, affecting their quality of life [6].
Menopause is associated with the gradual decline of ovarian function, is a genetically programmed process and is characterized by special symptoms. The recommendations of the Russian Association for Menopause highlight several significant periods. Premenopause - begins with a disturbance in the rhythm of menstruation in women who have a monotonously high level of follicle-stimulating hormone, and ends with the last menstruation. A synonym for the term “premenopause” is the term “menopausal transition”. Perimenopause is the period immediately preceding menopause, when there are already certain endocrinological, biological and clinical signs of its approach, plus the first year after menopause. Menopause is the period that begins from the moment of the last, independent menstruation (set no earlier than after 12 months of amenorrhea). Postmenopause characterizes the period following menopause, regardless of whether it occurred spontaneously (naturally) or was induced. Early postmenopause lasts for 5 years after the last menstrual period.
The most clinically significant manifestations of estrogen deficiency, which have a significant impact on the quality of life of women of perimenopausal and postmenopausal age, include neurovegetative disorders, which are often called climacteric syndrome in our country, as well as urogenital disorders, dystrophic changes in the skin, a high risk of developing atherosclerosis and coronary heart disease , osteoporosis.
Neurovegetative disorders are manifested by hot flashes, headache, lability of blood pressure, increased sweating, palpitations, and sleep disturbances [7]. Neurovegetative symptoms, including hot flashes and night sweats, are experienced by the majority of women (60-80%) during menopause. Sleep disturbance is also a common complaint in postmenopausal women. Ten years after their last menstrual period, 10% of women are still negatively affected by neurovegetative symptoms. Up to 16% of women aged 85 years and older still report having hot flashes [8, 14].
Women with hot flashes more often seek medical help, especially from outpatient gynecologists, due to decreased performance and deteriorating quality of life. Society's focus on youth and beauty also has a destabilizing effect on the mental state of a woman during menopause and leads to disruption of her adaptation at this time. Anxiety and depressive disorders in postmenopause can occur in 95.8% of women [6].
Hormonal changes during perimenopause can lead to the formation of climacteric (menopausal) syndrome, which is a pathological symptom complex including neurovegetative, metabolic-endocrine, and psycho-emotional disorders [1, 2].
In the pathogenesis of menopausal syndrome, the leading role is played by a change in the functional balance in the hypothalamic-pituitary and autonomic nervous systems, which is manifested by a violation of the production of norepinephrine and dopamine, which are involved in the process of thermoregulation. Due to an increase in the activity of noradrenergic and dopaminergic structures of the central nervous system, skin vessels dilate and the phenomenon of hot flashes occurs. There is also an increase in the level of luteinizing and thyroid-stimulating hormones with stable levels of follicle-stimulating hormone, prolactin and thyroid hormones in the blood plasma. Patients with menopausal syndrome have preserved circadian rhythms of thyroid-stimulating hormone release with a significant increase in its level at night, which contributes to an increase in hot flashes at this time of day. There is a seasonality in the manifestations of menopausal syndrome with a deterioration in the condition of women in the spring and autumn periods.
There are groups at increased risk for the occurrence of vegetative symptoms in women with menopausal syndrome. Thus, a key risk factor is excess body weight. For many years, it was believed that the presence of significant subcutaneous fat reduces the risk of autonomic symptoms due to extragonadal estrogen synthesis through aromatization of androgens, the levels of which are elevated. However, studies have shown that the presence of excess body weight can act as a thermal insulator, provoking the occurrence and aggravating the course of vegetative symptoms. The influence of other endocrine functions of adipose tissue cannot be excluded either [13]. The predisposition to autonomic disorders is especially pronounced in women with abdominal obesity [17].
The potential role of bad habits in the occurrence of menopausal syndrome is of interest. It has been shown that smoking increases the risk of neurovegetative symptoms of menopausal syndrome by 60% [13]. Diet, coffee consumption and low levels of physical activity were found to be less associated with the occurrence of autonomic symptoms [13].
Decreased mood, high levels of anxiety, and feelings of stress are associated with an increased frequency of autonomic disorders in the first 6 years of postmenopause [13]. Moreover, the most pronounced connection is observed between such manifestations of autonomic disorders as hot flashes and decreased mood and increased anxiety [12]. It has been noted that women with a negative mood and an increased sense of anxiety assess their condition worse and their quality of life is lower than women with the same severity of menopausal syndrome, but without a negative mood [16]. The period of perimenopause is also characterized by sleep disturbances. The most common symptoms are difficulty falling asleep, interrupted sleep, and early awakening [15].
Many women during menopause find themselves in a state of subclinical and clinically pronounced depression [9], especially during premenopause and early postmenopause, when autonomic disorders are most pronounced. It is known that postmenopausal women with neurovegetative disorders are more prone to developing depressive conditions compared to women without neurovegetative disorders [10]. The development of depressive states is associated with sleep disturbances and decreased mood, which are an important factor in the development of depression. In addition, autonomic disorders may be the initial manifestation of disturbances in the functioning of the serotonergic and noradrenergic systems, as well as a manifestation of changes in the level of neurotransmitters associated with the development of depressive states [11].
The principles of therapy for neurovegetative disorders are based on reducing clinical manifestations, reducing the risk of complications, and improving the quality of life of patients. Regular calcium intake with vitamin D3 supplements is also recommended. Non-drug therapy for menopausal syndrome is based on the recommendation of a diet low in sugar and sodium, with increased consumption of fruits, vegetables and plant fiber. Lifestyle changes, including quitting smoking, reducing alcohol consumption, and increasing aerobic physical activity, can reduce the manifestations of neurovegetative symptoms of menopausal syndrome [14].
Drug therapy for menopausal syndrome includes the use of hormone replacement monotherapy with estrogen preparations or a combination of estrogens with gestagens. However, there are a number of limitations to the use of hormone replacement therapy. The increased risk of stroke, thromboembolic complications, cancer, and the patient's refusal of hormonal therapy significantly limit the use of hormone replacement therapy. Thus, there is a need for alternative, non-hormonal therapy for neurovegetative disorders in women with menopausal syndrome. As a non-hormonal therapy for the correction of neurovegetative symptoms, a drug is required that effectively normalizes the functions of the autonomic nervous system without causing dependence and withdrawal syndrome. Reducing the vegetative symptoms of menopausal syndrome is possible with treatment with benzodiazepines. However, muscle relaxation, dependence, drowsiness and decreased attention significantly limit the use of this group of drugs. The drug from the subgroup of atypical benzodiazepines, tofisopam (Grandaxin), is practically devoid of these side effects. In addition to the fact that the drug does not have a muscle relaxant or sedative effect, it also does not potentiate the effect of alcohol, does not cause addiction and does not impair memory and attention [5]. There is data on the safety and effectiveness of Grandaxin therapy for climacteric disorders [3], including surgical menopause [4]. The vegetative-corrective and anxiolytic effect of Grandaxin has been shown in women during perimenopause with severe vegetative symptoms and the presence of anxiety and depressive disorders [4]. The use of Grandaxin improves the quality of life of women with autonomic disorders [3].
The use of Grandaxin in patients with menopausal disorders is possible both in combination with hormonal drugs and as non-hormonal therapy. Grandaxin is available in 50 mg tablets and is prescribed 1-2 tablets 1-3 times a day. For occasional use, you can take 1-2 tablets. The maximum daily dose is 300 mg (up to 6 tablets per day). The duration of continuous course use of Grandaxin in the correction of psychoemotional and neurovegetative disorders during menopause and surgical menopause can last up to 3 months [4].
Thus, the use of Grandaxin in non-hormonal therapy of neurovegetative and psycho-emotional disorders in menopausal syndrome is pathogenetically justified and effective. The vegetative-corrective and anxiolytic effect of the drug in combination with the absence of muscle relaxation, sedation, and dependence allows us to recommend Grandaxin for use as part of the complex therapy of menopausal disorders.