Diencephalic cachexia (DC), or Russell's syndrome, is a rare disorder caused by a tumor lesion of the hypothalamic region. Its prevalence in the population is unknown. Since the first description of the syndrome by the English pediatrician A. Russell in 1951, it has been considered characteristic exclusively of early childhood [1-3].
A feature of the disease is the development of severe cachexia against the background of adequate nutrition and satisfactory health. Children often experience a lack of weight gain while maintaining linear growth rates. They often experience mental and behavioral changes that are noticeable to others. They become overly sociable, disinhibited and euphoric. Good health and physical activity are maintained in patients, despite severe exhaustion. As the tumor grows, various neurological symptoms often appear in the clinical picture, caused by compression of the surrounding brain structures by the tumor [1–6].
It should be noted that a progressive decrease in body weight with almost complete atrophy of subcutaneous fatty tissue may be the leading and, as a rule, the only manifestation of the disease in the early stages. This greatly complicates the timely diagnosis of the tumor before the onset of neurological symptoms. Regression of cachexia can be observed against the background of a decrease in tumor volume after surgical treatment, as well as during radiation and/or chemotherapy [7–10]. If left untreated, most patients die within 1–2 years [2]. Development of D.K. observed with suprasellar tumors of the anterior parts of the hypothalamus, as well as the chiasm and optic nerves, compressing the bottom of the third ventricle. Among those described in the literature [10–16], astrocytomas and other types of gliomas prevail. Much less frequently, the causes of DC were germinoma and craniopharyngioma (CP) [17, 18]. The age of children at the onset of the disease ranges from the neonatal period to 4 years with a peak in the first 2 years of life [2–6]. In adults, this syndrome is extremely rare: 4 cases of tumor lesions of the hypothalamus with the development of DC: 2 are caused by CF, 2 others by astrocytoma [19-22]. In foreign literature [1–6, 8–11, 14, 15, 18–23], this disorder is more often described as “diencephalic syndrome.” We present a rare case of DC development in a 24-year-old woman with papillary CF.
Description of a clinical case
Patient P
., 24 years old, (born in 1991) applied to the National Medical Research Center of Neurosurgery named after. N.N. Burdenko in August 2015 with complaints of progressive weight loss, thirst, absence of the menstrual cycle, decreased vision, and headache.
From the anamnesis it is known that she grew and developed normally. From previously suffered diseases: chronic pyelonephritis against the background of hereditary congenital duplication of the kidneys. There were no injuries or operations. The patient is married and has 2 children (two normal pregnancies ended in term births in 2009 and 2013, the children are healthy). After the second birth, amenorrhea persisted. However, the patient did not attach any importance to this and did not contact the doctors.
In January 2015, she began to notice a decrease in body weight due to adequate nutrition. Since March 2015, thirst, decreased vision, headache, and decreased memory appeared. Gradually lost body weight by 20 kg (from 48 to 28 kg). In May of the same year, magnetic resonance imaging (MRI) of the brain was performed, which revealed a tumor of the chiasmal-sellar region spreading into the third ventricle. To clarify the diagnosis and choose treatment tactics, the patient was sent to the National Medical Research Center of Neurosurgery named after. N.N. Burdenko.
On admission: condition is relatively satisfactory. Height 161 cm, body weight 28 kg, body mass index (BMI) - 10.9 kg/m2 (normal range 18-25 kg/m2). Outwardly he looks older than his age. Noteworthy is the complete absence of subcutaneous fat (Fig. 1, b, c).
Rice. 1. Appearance of patient P. with craniopharyngioma. a — before the onset of the disease (body weight 48 kg); b, c — upon admission to the National Medical Research Center for Neurosurgery (body weight 28 kg, practically no subcutaneous fat tissue).
The skin and visible mucous membranes are pale, with normal moisture. Teeth and fingers without signs of systemic “vomiting” behavior. Blood pressure 80/60 mm Hg. Heart rate 50 beats/min. Regular stool. There is no dysuria. The thyroid gland is not enlarged, soft, painless, nodules in it are not palpable.
ECG: sinus rhythm, heart rate 45 beats/min, normal position of the electrical axis of the heart, impaired AVL repolarization.
An examination by a neuro-ophthalmologist revealed visual disturbances in the form of chiasmal syndrome. VISOD = 0.6; VISOS = 0.9. Bitemporal hemianopsia. On the fundus: optic discs with blanching in the temporal half, clear boundaries. There are no focal otoneurological symptoms.
Psychiatrist examination data: the patient is quite active, approaches doctors independently, and is interested in her condition. Noteworthy is the obvious decrease in criticism: the patient does not take the situation into account, does not keep distance (goes into the doctor’s office to ask for tea, look out the window, etc.). At the same time, he actively talks about his life and illness, clarifying all the small details, getting stuck on trifles. Lists numerous complaints without highlighting the main ones. Only upon questioning does he complain of a noticeable decrease in memory that occurred simultaneously with weight loss. The emotional background is noticeably heightened, with a euphoric tint. Focused on the current time, place and personal situation. He is interested in the upcoming operation and his future, but at the same time does not show any particular concern or worry about either the operation or its possible consequences. According to relatives, such behavior and style of communication were not previously characteristic of the patient.
Laboratory data: clinical blood test
- decrease in hemoglobin level to 108 g/l (112-153), red blood cells to 3.56 (3.80-5.15 10·12/l), shift of the leukocyte blood count to the left: band neutrophils - 8% (1-6 ); segmented - 29% (47-72), lymphocytes - 57% (19-43), ESR 3 mm/h (2-15).
Clinical and biochemical analysis of morning urine
: reduction in specific gravity to 1004; sodium 148.3 (135-145) mmol/l, osmolality 649 mOsm/kg (>300 mOsm/kg).
Blood chemistry
without electrolyte disturbances, blood osmolality - 286 mOsm/kg H2O (275-295), increased ALT to 80 U/l (up to 60), hypoalbuminemia - 32 g/l (35-52), decreased serum iron level to 10.4 µmol/l (10.7-25), other indicators unchanged. The level of glycated hemoglobin (HbA1c) is 4.7% (<6.1%).
Hormonal blood test data
presented in the table indicate the presence of secondary hypothyroidism, hyperprolactinemia, and secondary hypogonadism. There is no convincing evidence for the presence of secondary adrenal insufficiency and diabetes insipidus. Noteworthy is the high level of somatotropic hormone (GH) against the background of reduced insulin-like growth factor-1 (IGF-1). The last change is characteristic of DC, but, like the above disorders, is not the cause of weight loss.
Results of a hormonal blood test of a patient before and after surgery to remove craniopharyngioma (explanations in the text) Note.
b-hCG - human chorionic gonadotropin. When performing MRI of the brain on a series of tomograms in three projections, in T1, T2, DWI and FLAIR modes before and after intravenous administration of a contrast agent, a cystic-solid formation of the chiasmal-sellar region with endosuprasellar growth is determined. The solid part of the tumor intensively accumulates contrast agent, corresponding in its location to the altered pituitary stalk, filling the space from the adenohypophysis to the hypothalamic infundibulum. There are cystic cavities around (above and around) the solid component of the tumor. The ventricular system is not dilated or displaced (Fig. 2).
Rice. 2. MRI with contrast enhancement in sagittal (a) and frontal (b) projections before the first operation (picture of stalk craniopharyngioma).
On September 2, 2015, an operation was performed (surgeon - Academician of the Russian Academy of Sciences A.N. Konovalov) - transcranial removal of the CF of the stem-infundibular localization using the basal frontotemporal approach. An “anterior” variant of the chiasma with short optic nerves was discovered. The tumor was removed through the opticocarotid triangle. Directly above the sella turcica, dense grayish-yellow tissue with a lumpy surface, with a thin capsule, extending into the cavity of the third ventricle, similar in appearance to papillomatous K.F., was found. Its removal was carried out mainly using ultrasonic suction. As the tumor was removed, large cysts were emptied, the capsule of which had arterial branches that were preserved. The walls of the capsule are mostly excised. In the posterior sections of the capsule, remains of the pituitary stalk were identified. The tumor was removed almost completely with the exception of fragments of the capsule that extended into the cavity of the third ventricle.
Immediately after the operation, a computed tomography (CT) scan of the brain was performed, which confirmed the high degree of radical removal of the tumor with the preservation of small remains in the infundibular region of the third ventricle (Fig. 3).
Rice. 3. SCT after the first operation (explanations in the text).
Histological diagnosis: papillary craniopharyngioma. In the postoperative period, therapy was carried out with hydrocortisone (100 mg/day intramuscularly for 7 days, then 25 mg per day orally), thyroid hormone preparations (L-thyroxine 25 mcg orally). On the 2nd day after surgery, signs of diabetes insipidus appeared in the form of thirst and polyuria up to 4000 ml per day, hypernatremia (sodium 147-149 mmol/l). The drug desmopressin (minirin 0.05 mg orally 3 times a day) was added to therapy.
In the early postoperative period, there was an increase in the severity of emotional and personal disorders (euphoricity, relief, non-criticality). Against this background, visual illusions of perception occurred occasionally, coinciding with water and electrolyte disturbances. There was also an inversion of the sleep-wake cycle. By the time of discharge, visual hallucinations had regressed and nighttime sleep had been restored. The patient was discharged with emotional, personal and cognitive disorders, which were detected to the same extent as before the operation.
With neuro-ophthalmological control, vision was maintained at the preoperative level. After the operation, the patient began to actively gain weight. By the time of discharge (12 days after surgery), the patient had gained 14 kg in body weight and was 42 kg (Fig. 4, a). Based on a hormonal examination, panhypopituitarism was diagnosed; moderate hyperprolactinemia persisted (prolactin 1005 mU/l) (see table). The patient was discharged in satisfactory condition with recommendations to continue replacement therapy for secondary adrenal insufficiency (Cortef 10 mg in the morning and 5 mg in the afternoon), secondary hypothyroidism (L-thyroxine 50 mcg), diabetes insipidus (minirin 0.1 mg 2 times a day) . Within 3 months, there was an increase in body weight by another 4 kg, followed by stabilization of body weight within 45-46 kg.
Rice. 4. The patient’s appearance after the first operation. a — 12 days after surgery (body weight increased from 28 kg to 42 kg); b — 6 months after surgery (body weight 46 kg).
A follow-up examination of the patient was carried out 6 months after the operation. Upon examination on January 18, 2016: the condition was satisfactory, consciousness was clear. Body weight - 46 kg, BMI - 16.89 kg/m2 (see Fig. 4, b).
The mental status retained a euphoric tone of mood, relief and disinhibition, and non-criticism. At the same time, the existing noticeable emotional and personal disorders did not affect the “quality of life” of the patient. During a hormonal examination (01/18/16), the patient still had panhypopituitarism, diabetes insipidus, and hyperprolactinemia (see table). Substitution therapy was adjusted: the dose of L-thyroxine was increased to 125 mcg in the morning, it was recommended to continue taking Cortef and Minirin in the previous doses, as well as the use of sex hormones after a gynecological examination. MRI dated January 18, 2016 (Fig. 5), as well as SCT after surgery (see Fig. 3), revealed tumor remains in the area of the pituitary stalk and the bottom of the third ventricle. In this regard, the patient was recommended to undergo stereotactic radiation, which was scheduled for September 2021.
Rice. 5. MRI of the brain with contrast enhancement in sagittal (a) and frontal (b) projections 6 months after surgery (tumor remains are visualized in the area of the pituitary stalk and the bottom of the third ventricle).
From January to May 2021, the patient's condition remained stable. However, in May 2021, she began to notice a headache, weakness, memory impairment, and periodic involuntary urination. Over the course of a month, further deterioration of the condition was observed in the form of increasing drowsiness, the appearance of weakness in the right limbs, loss of body weight, and weakening of control of pelvic functions. The level of wakefulness gradually decreased, the patient stopped moving independently, did not speak, and slept most of the day. It is known that she did not stop taking replacement therapy (Cortef 15 mg, L-thyroxine 125 mcg, Minirin 0.1 mg 2 times a day); She did not receive sex hormone replacement therapy.
On 08/01/16, due to progressive deterioration of her condition, she was hospitalized. On examination: the condition is serious, the level of consciousness corresponds to deep stupor. The skin and visible mucous membranes are pale, with normal moisture. Blood pressure 80/50 mm Hg. Heart rate - 60 beats/min. Muscle strength in the right limbs was reduced to 34 points. Does not control pelvic functions. No other significant deviations in the patient's condition were found.
Vision without obvious deterioration: VIS OD = 0.9; VIS OS = 0.9. Bitemporal hemoanopsia. On the fundus: optic discs with blanching in the temporal half, clear boundaries.
A clinical blood test revealed a decrease in hemoglobin level to 111 g/l (112-153), a biochemical blood test revealed a decrease in creatinine to 45 µmol/l (50-115), albumin to 34 g/l (35-50); sodium - 144 mmol/l (135-145), other indicators without deviations. According to the results of a hormonal blood test, panhypopituitarism persisted (secondary hypothyroidism and hypocortisolism were compensated for with medications), moderate hyperprolactinemia (prolactin 853 mU/l) (see table).
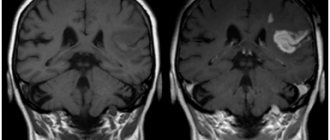
MRI of the brain revealed a relapse, mainly in the form of a gigantic multilocular cyst extending into the third ventricle (Fig. 6).
Rice. 6. MRI of the brain with contrast enhancement before the second operation in sagittal (a) and frontal (b) projections 8 months after the first operation (MRI picture of a giant multilocular, predominantly cystic craniopharyngioma of endosuprasellar localization, grossly compressing the brain stem).
On 08/04/16, the second operation was performed - transcranial removal of the CF of the third ventricle and sella turcica (surgeon - Academician of the Russian Academy of Sciences A.N. Konovalov) from a combined transcallosal and right-sided subfrontal approach with endoscopic assistance. First, removal was performed from the transcallosal approach on the right. In the area of the right foramen of Monroe, a tumor cyst wall was found that was perforated (according to urgent histology, there was no tumor tissue in it). A yellow-gray tumor was found in the area of the anterolateral wall of the third ventricle on the right. It is separated from its walls and removed. In the basal parts of the third ventricle there was a tumor capsule, which passed into its bottom without clear boundaries. Then, using the right-sided subfrontal approach through the optic carotid triangle, the remaining basal part of the tumor was removed, including the cyst wall that extended into the sella turcica. Then, using a repeated transcallosal approach, all fragments of the suprasellar capsule where there were visible tumor growths were excised.
Histological examination confirmed papillary CF.
A control CT scan performed on the day of surgery showed total removal of the tumor with the presence of small fragments of hemostatic materials in its bed (Fig. 7).
Rice. 7. SCT after the second operation. Radical tumor removal. Hemostatic material is visible in its bed.
On the 2nd day after surgery, against the background of the development of hypernatremia (sodium 147-163 mmol/l), episodes of psychomotor agitation with confusion were noted. At the same time, the patient was grossly disoriented in place and time, wanted to go somewhere, talked to herself, and did not give in to persuasion. She showed dysphoria, aggressiveness towards her caring relatives, and resisted medical procedures. At night I slept intermittently. Over time, against the background of correction of water and electrolyte disturbances, sedative and psychotropic therapy, these symptoms significantly regressed.
At discharge, visual functions remained at the preoperative level. The psychoneurological status showed clear positive dynamics with restoration of consciousness and orientation, complete regression of right-sided hemiparesis, and restoration of control of pelvic functions. The patient was discharged home on the 14th day after surgery.
2 months after the second operation, from 10/17 to 10/21/16, the patient underwent a course of stereotactic radiotherapy (Fig. in the hypofractionation mode of 5 fractions of 5.5 Gy. The total focal dose was 27.5 Gy. During the treatment, the patient’s condition remained stable.
in the hypofractionation mode of 5 fractions of 5.5 Gy. The total focal dose was 27.5 Gy. During the treatment, the patient’s condition remained stable.
Rice. 8. MRI of the brain with contrast enhancement before radiation therapy in sagittal (a) and frontal (b) projections.
2 months after the course of stereotactic radiotherapy, the patient’s condition was satisfactory. There is no evidence of relapse on MRI. Blood test for hormones without significant differences from those shown in the table. She is active on replacement therapy and has no complaints. Body weight 50 kg (Fig. 9, 10).
Rice. 9. MRI of the brain with contrast enhancement in sagittal (a) and frontal (b) projections 3 months after radiation therapy.
Rice. 10. Appearance of the patient 4 months after the second operation and 2 months after radiation therapy.
Throughout the entire treatment process, the patient's hormonal status was studied (see table).
Discussion
Weight loss is widespread in the pathogenesis of many diseases (chronic heart and kidney failure, diabetes mellitus, Addison's disease, rheumatoid arthritis, Alzheimer's disease, malignant neoplasms, etc.). Regardless of etiology, cachexia is a serious medical problem. Even a slight decrease in body weight in patients determines an unfavorable prognosis for the course of the disease and is a powerful predictor of high mortality [24–26]. The most life-threatening condition is a loss of more than 40% of ideal body weight [26, 27]. Since ancient times, the term “cachexia” (Greek kachexia, kakos
"bad" + hexis "condition) was synonymous with rapid death. “The flesh disappears... shoulders, collarbones, chest, fingers seem to melt. This state is the face of death,” wrote Hippocrates [28]. I.S. Turgenev in 1846, in his story “Living Relics,” describes cachexia in a young woman who was “the first beauty, tall, plump, white, ruddy...”. “Before me lay a living human being, but what was it? The head is completely dry, one-color, bronze - like an icon of an ancient letter; the nose is narrow, like a knife blade; You can barely see your lips—only your teeth and eyes are white, and from under your scarf, thin strands of yellow hair spill out onto your forehead. At the chin, on the fold of the blanket, two tiny hands, also bronze-colored, are moving, slowly moving their fingers, like sticks... the face is not only not ugly, even beautiful, but terrible, extraordinary” [29].
Despite the fact that the first description of cachexia was made more than 2000 years ago, questions of its pathogenesis in various diseases are still the subject of debate and scientific research. Body weight loss in CSR tumors remains unstudied. We describe a rare case of diencephalic cachexia in a young woman with CF.
CF are benign epithelial tumors (WHO I), which develop from the remains of embryonic cells of Rathke's pouch, located along the pharyngeal-pituitary tract. The incidence of CF in adults is about 2.1–4.6% of all intracranial neoplasms [30–32].
Histologically, there are two main types of CF: adamantine-like and papillomatous. The papillomatous variant occurs, as a rule, only in adults. CF are characterized by the presence of a solid and cystic component, which is detected in approximately 80% of cases [33, 34]. The occurrence of papillomatous CF, in contrast to adamantine-like ones, is associated with metaplasia of epithelial cells. Papillomatous K.F. predominantly localized in the region of the third ventricle; one of the names of these tumors is papillomas of the third ventricle.
Embryogenesis and topography of CF determine the high frequency of endocrine and metabolic disorders. The result of damage to the hypothalamic region can be an imbalance in energy homeostasis, leading to the development of obesity or cachexia. It is known that CF is often associated with the development of diencephalic (hypothalamic) obesity [35, 36]. DC is less common and is represented by descriptions of only isolated cases. Thus, in a large retrospective study among children with CF, out of 485 cases, the development of DC was observed in only 7 patients [37]. It is assumed that the development of obesity or cachexia in CF is associated with invasive tumor growth in contrast to its compression of the hypothalamic region, respectively [6, 37]. To date, the pathophysiology of DC remains unknown. Modern ideas about the central mechanisms of metabolic control suggest that weight loss in DC is caused by dysfunction of hypothalamic neurons involved in the regulation of energy homeostasis and body weight. The lack of clinical and laboratory data on secondary hypofunction of peripheral glands, primarily hypocortisolism, clearly demonstrates different mechanisms of weight loss in DC and Symonds and Sheehan syndromes.
Weight loss is a key symptom and the main reason for seeking medical help. When examining such patients, at the first stage of diagnosis, malnutrition, anorexia nervosa and conditions associated with malabsorption (impaired absorption of nutrients in the small intestine) are excluded. Further, the diagnostic search should be aimed at excluding organic pathology of the brain, even in the absence of general cerebral or focal neurological symptoms.
In our clinical observation, the manifestation of the disease coincided with the postpartum period; secondary amenorrhea was not regarded by the patient as a reason to seek medical help. Only a rapid decrease in body weight led her to be examined by doctors, and the appearance of neuro-ophthalmological symptoms in the form of chiasmal syndrome played a decisive role in conducting an MRI of the brain.
By the time the tumor was detected, the body weight deficit was about 20%, and by the time of hospitalization - more than 40% of the initial body weight, which is critical for the patient’s life.
Until the stage of surgical treatment or the impossibility of surgery, such patients require constant nutritional support. Currently, there is no generally accepted pharmacological therapy for the treatment of cachexia of any etiology.
From laboratory data, attention was drawn to the increase in basal GH levels characteristic of DCs against the background of a decrease in IGF-1. Similar changes can be observed with cachexia of any etiology, for example with anorexia nervosa [38].
The patient also showed a significant increase in prolactin levels, which was not previously described in D.K. This change is most likely due to blockade of the dopaminergic system when the tumor is located suprasellar. Laboratory tests confirmed secondary hypogonadism. No other clinically significant biochemical abnormalities were detected. All these changes are not the cause of weight loss, but develop secondary.
It should be noted that despite the pronounced lack of body weight, the patient remained in good health and physical activity, and was in an “elevated” mood, which created a contrast with her appearance. The presence of elevated mood and even euphoria has often been described in children with DC by authors of previously published cases.
This clinical observation is also of interest because the development of DC is typical for children in the first 2-3 years of life and is extremely rare in adults. Development of D.K. most often cause astrocytomas of the diencephalic region of varying degrees of malignancy. Other types of tumors, including CF, as in our case, are rather an exception. The development of cachexia is more likely a sign of irritation of intact hypothalamic structures, since regression of symptoms was noted after surgery.
The main treatment method for CF remains surgical. The anatomical proximity of the tumor to vital structures (the floor of the third ventricle, the optic nerves and chiasm, the great vessels of the base of the brain) determines the significant complexity of surgical treatment and creates difficulties for their radical removal [39–44]. As a rule, removal of CP leads to an increase in neuroendocrine disorders [44, 45]. In the observation we presented, the patient developed additional disorders after the first operation - diabetes insipidus, central hypocortisolism and hypothyroidism, and secondary hypogonadism persisted (see table). The patient required lifelong replacement therapy with L-thyroxine, hydrocortisone, desmopressin and sex steroids. However, it is important to emphasize that the patient began to quickly gain weight, despite the fact that there were tumor remnants in the area of the bottom of the third ventricle. Thus, we can assume a significant role of compression, and not destruction of diencephalic structures for the development of cachexia in the observation we described.
To date, the control of tumor growth after non-radical removal of CF remains an unsolved problem [46]. This tumor has a high recurrence rate, reaching 30% within 10 years with total resection [34, 39, 47].
Incomplete removal of CF is a prerequisite for tumor recurrence and determines the indications for stereotactic irradiation [39]. Our observation was also indicative in this regard. Continued tumor growth was detected in the patient 8 months after non-radical surgery. According to MRI of the brain, the size of the recurrent tumor exceeded the original ones, which characterizes CF as a tumor with an aggressive course. Considering the localization of the tumor, the goal of treating such patients is not only radical removal of the tumor, but also preventing the development of severe complications associated with damage to the hypothalamus. Such operations should be performed in institutions that have a multidisciplinary team of specialists, including a neurosurgeon, neurologist, radiologist, endocrinologist, psychiatrist and ophthalmologist.
Thus, in each case, the treatment strategy is determined individually based on the growth pattern and histology of the tumor, as well as the age and condition of the patient. Often, only partial removal or biopsy of the tumor is possible, followed by the use of non-surgical methods. In such cases, radiation and/or chemotherapy may be the only chance to save the patient [8, 9, 48, 49]. It is difficult to explain why, but even partial removal of the tumor can lead to regression of cachexia, which is what happened in our observation. Sometimes there is a restoration of body weight followed by the development of obesity [8, 23]. A detailed study of the mechanisms that control energy metabolism may shed light on the pathogenesis of these disorders and determine a targeted approach in the treatment of patients with metabolic disorders.
All photographic materials are posted with the voluntary written consent of the patient
.
The authors declare no conflict of interest.
Reasons for the development of diencephalic syndrome
The vessels involved in the blood supply to the hypothalamus are characterized by increased permeability. This makes them vulnerable to various damaging factors, the impact of which causes the development of diencephalic syndrome. The function of the hypothalamus may be affected for the following reasons:
- traumatic brain injury;
- previous neuroinfection;
- the presence of tumors that put pressure on the hypothalamus;
- severe diseases of internal organs;
- hormonal changes during pregnancy;
- birth trauma or postpartum hemorrhage;
- insufficient protein nutrition, starvation, anorexia nervosa;
- stress or mental trauma;
- the presence of foci of chronic infection of the ENT organs, genitourinary system, gastrointestinal tract;
- intoxication (drinking alcohol, smoking, drug use, occupational hazards, environmental pollution).
Considering the multifaceted function of the hypothalamus in the body’s activities, the clinical picture of its lesions is extremely diverse.
A comment
The subject of discussion in the presented work was a rather rare pathology - diencephalic cachexia (DC), the pathogenesis of which remains unexplored to date. The article presents a unique clinical observation of DC in a young woman with papillary craniopharyngioma. A detailed presentation of clinical manifestations, laboratory and MRI data clearly demonstrates the primary role of diencephalic lesions in weight loss and the development of cachexia. The long follow-up period gives particular value to this observation. It is important to emphasize that the regression of cachexia after surgery is probably associated only with compression of the diencephalic structures, and not with their destruction. Based on the analysis of the literature carried out by the authors, the issues of etiology, clinical picture, diagnosis of DC against the background of various tumors of the chiasmal-sellar region and modern approaches to their treatment are also considered. It is emphasized that weight loss may be the first manifestation of craniopharyngioma. The rapid course of the disease with the development of cachexia and the lack of effective therapeutic agents emphasize the importance of early diagnosis and timely surgical treatment, as well as the need for a multidisciplinary approach to the management of such complex patients. All this determines the exceptional relevance of this problem (article).
The article is written in good literary language and is read with great interest.
L.Ya. Rozhinskaya (Moscow)
Diencephalic syndrome and the hypothalamus
The hypothalamus (lat. hypothalamus) or hypothalamus is the part of the brain that suffers from diencephalic syndrome. This is the highest vegetative center that controls the work of all endocrine glands: the pituitary gland, adrenal glands, ovaries, thyroid and pancreas.
The hypothalamus controls the respiratory, cardiovascular, digestive and excretory systems. It is responsible for regulating body temperature, sleep and wakefulness rhythms, feelings of thirst and hunger, as well as human emotions and behavior.
Various clinical picture of diencephalic syndrome
Due to the many symptoms, doctors of various specialties often encounter diencephalic syndrome: endocrinologists, therapists, gynecologists, neurologists, surgeons, psychiatrists, dermatologists, etc.
With diencephalic syndrome, the following types of disorders are noted:
Autonomic-vascular disorders are manifested by crises, during which the following occur: suffocation, weakness, drowsiness, sweating, nausea, and also a rare pulse, a drop in blood pressure, pallor, and decreased motor activity. Autonomic-vascular crises are often replaced by sympatho-adrenal crises, which are characterized, on the contrary, by an increase in blood pressure.
Violation of thermoregulation is characterized by the appearance during a crisis of chills, increased sweating, an increase in body temperature to 38-39°C and often involuntary urination.
Neuromuscular disorders are expressed in asthenia, general weakness and adynamia, accompanied by low-grade fever, feelings of hunger and thirst, insomnia and unpleasant sensations in the heart area. The course of the disease is often paroxysmal.
Neurotrophic disorders are manifested by itching, dryness, the occurrence of neurodermatitis and bedsores, ulcers of the gastrointestinal tract, as well as softening of bones (osteomalacia). Against this background, the following are noted: drowsiness, general weakness, adynamia, tremor and a feeling of thirst. The course of the disease is critical.
Neuropsychic disorders are characterized by asthenia, sleep disturbances, and a decrease in the level of mental activity. In this case, hallucinations, a state of anxiety and fear, frequent mood swings, hypochondriacal disorders, and delusional states occur.
Hypothalamic epilepsy is a special form of epileptic seizures in which the primary focus is located in the hypothalamus. From it, excitation is transmitted to the cortical and subcortical motor centers. During attacks, the patient experiences palpitations with a rise in temperature and blood pressure (BP), tremors, respiratory distress, and fears. The electroencephalogram (EEG) records epileptic outbreaks in the form of single waves.
Neuroendocrine disorders are associated with dysfunction of not only the hypothalamus, but also other endocrine glands: thyroid, adrenal glands, pituitary gland. Isolated forms of endocrine dysfunction are often observed, such as diabetes insipidus, hypothyroidism, Itsenko-Cushing's disease, Sheehan's syndrome. The last two are often encountered in the practice of a gynecologist, so we will talk about them in more detail.