Fetal hydrocephalus is an increase in the volume of fluid in the child's brain and spinal cord, accompanied by an increase in head size. Such children often have problems with mental and physical development. Hydrocephalus, like other fetal pathologies, is detected by screening ultrasound during pregnancy, but there are still many children born with this diagnosis.
Appointment with a gynecologist - 1000 rubles. Comprehensive pelvic ultrasound - 1000 rubles. Admission based on test results - 500 rubles. (optional)
CLICK TO MAKE AN APPOINTMENT or ultrasound tests
Why does hydrocephalus form in the fetus?
The content of the article
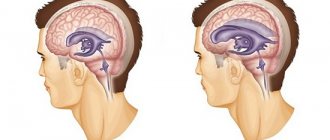
Inside the medulla, there are chambers called ventricles. They contain cerebrospinal fluid (CSF), which flows down and circulates around the brain and spinal cord. The purpose of the fluid is to act as a cushion for the brain, protecting it from damage. But sometimes cerebrospinal fluid is formed in excess or does not flow well from the brain structures. Such a child develops hydrocephalus (water on the brain).
The disease can occur due to mutations that appear during the process of fertilization, or unfavorable heredity. But often it is caused by infection of a woman during pregnancy with TORCH infections - rubella, toxoplasmosis, herpes, cytomegalovirus infection. Sometimes a developmental abnormality can be caused by a common flu suffered at the beginning of pregnancy, when the organs of the unborn baby are just forming.
Sometimes hydrocephalus is caused by intrauterine oxygen deprivation of the fetus. This condition is observed in women with a constant threat of miscarriage, whose uterus is in good shape throughout the pregnancy.
These conditions affect the baby's entire body, and 50-80% of babies with hydrocephalus have other developmental defects.
Therefore, pregnant women who have had a viral infection or suffer from constant increased uterine tone need to undergo an interscreening ultrasound in addition to the mandatory screenings to see how the child is developing.
These children are found to have:
- Chiari malformation
, in which brain structures protrude beyond its boundaries, “falling out” through the foramen magnum. Pathology, in addition to hydrocephalus, is accompanied by paralysis of the legs and other movement disorders; - Spinal defects
(spina bifida, spinal hernia), in which a hernial sac containing cerebrospinal fluid and sections of the spinal cord with membranes and nerves protrudes from the child’s back. 85% of these children develop hydrocephalus; - Brain cysts
are tumor-like formations in the brain, filled with fluid and compressing the brain matter; - Incorrect development of cerebral veins
, accompanied by protrusion of their walls - aneurysms. Such children also suffer from severe headaches and often die from extensive cerebral hemorrhage caused by ruptured aneurysms. - Blindness and strabismus
caused by compression of the optic nerve by excess fluid, leading to disturbances in its function and even atrophy.
Treatment of hydrocephalus
In most cases, hydrocephalus requires surgical treatment. Conservative therapy is used to reduce the symptoms of compensated hydrocele of the brain only with a minimal increase in the amount of cerebrospinal fluid and a moderate course of the disease. For this purpose, diuretics or glucocorticosteroids are prescribed.
Closed hydrocephalus requires urgent surgical intervention, since cerebrospinal fluid quickly accumulates and there is a risk of displacement of the brain stem, pressing it into the foramen magnum. In this case, vital parts responsible for breathing and blood circulation are damaged. Respiratory and cardiac activity stops.
Emergency surgery is performed to decompress the cranial cavity. The simplest method is resection trepanation. In a child of the first year of life, a puncture of the lateral ventricles of the brain through the fontanelles can be performed, which helps to quickly reduce intracranial hypertension. For closed hydrocephalus, drainage is used, which is much more effective than ventriculopuncture, especially in children with developmental anomalies. A silicone catheter is inserted into the brain ventricle, which communicates at the other end with a sterile container. In some cases, it is necessary to carry out bilateral drainage. In neurosurgical practice, unloading lumbar punctures are also used. The above methods have a temporary effect and are preparatory steps for a more complex operation.
Surgery for occlusive hydrocephalus is aimed at removing the obstruction to the outflow of brain fluid. Once the barrier is removed, circulation is resumed and the child recovers. But sometimes this procedure cannot be completed fully, so the surgeon looks for workarounds to discharge excess cerebrospinal fluid by shunting.
Open dropsy of the brain was incurable for a long time. With the introduction of new materials, neurosurgery has successfully solved this problem. The cavity of the ventricles of the brain through drainage valve systems is connected to other organs, where cerebrospinal fluid is absorbed and does not accumulate. There are mainly two types of shunting used: ventriculoperitoneostomy and ventriculoatriostomy. In the first case, the catheter is inserted into the abdominal cavity. This is the most effective and common method. But if there are obstacles to its implementation, then a second one is used, during which the shunt is connected to the atrium.
Ultrasound diagnosis of hydrocephalus
The main symptom of the disease is an increase in the size of the head, caused by increased fluid pressure on the soft bones of the baby. The first and subsequent screenings show that the fetal head is too large.
When making a diagnosis, the doctor compares the size of the fetal head with normal ones. To do this, measure the dimensions of the head:
- Biparietal (BPR) - the distance between the temples along the line of the superciliary arches;
- Fronto-occipital (FOR) - the distance between the forehead and the back of the head.
An increase in both indicators indicates possible hydrocephalus. The more they deviate from the norm, the more severe the pathology. The data in the tables is considered approximate as it depends on the size of the fetus
| Duration in weeks | BPR, mm | LZR, mm |
| 10-11 | 13-17 | – |
| 12-13 | 21-24 | – |
| 14-15 | 27-31 | – |
| 16-17 | 34-38 | 45-50 |
| 18-19 | 42-45 | 54-58 |
| 20-21 | 48-51 | 62-66 |
| 22-23 | 54-58 | 70-74 |
| 24-25 | 61-64 | 78-81 |
| 26-27 | 67-70 | 85-88 |
| 28-29 | 73-76 | 91-94 |
| 30-31 | 78-80 | 97-101 |
| 32-33 | 82-84 | 104-107 |
| 34-35 | 86-88 | 110-112 |
| 36-37 | 90-92 | 114-116 |
| 38-40 | 94-96 | 118-120 |
Therefore, to identify hydrocephalus, the gynecologist simultaneously measures all other dimensions of the child. If they are also larger than normal, then the baby is simply large. With hydrocele of the brain, the development of the fetus often suffers, so its body and limbs are even smaller than necessary.
Measurements make it possible to differentiate hydrocephalus from a congenital increase in the size of the cerebral ventricles. Since these children do not have increased cerebral pressure, the head size may be normal. Sometimes it is even less than normal.
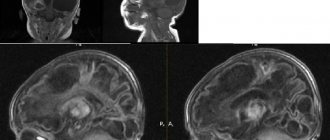
With hydrocephalus, the ventricles are filled with cerebrospinal fluid and are therefore deformed and enlarged. The size of their lateral walls, which is normally 7.5 mm, increases to 1 cm. The height of the ventricles increases by 0.2-0.3 mm. Incorrect development of other parts of the spinal cord and brain - the cisterna magna and the interhemispheric fissure - is often observed. At later stages, it is noticeable that the baby’s brain convolutions are flattened, the furrows are smoothed, and the vessels and membranes are incorrectly formed.
Classification of the disease
In children, there are four main types of hydrocephalus of the brain:
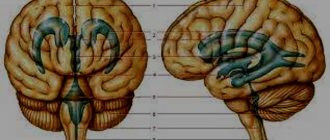
- External - fluid accumulates in the subarachnoid space - the cavity between the pia mater and the arachnoid mater.
- Internal - cerebrospinal fluid remains in the cerebral ventricles. The substance of the brain begins to thin out.
- Open (communicating) - all ventricular systems of the brain expand, but there are no obstacles to the movement of fluid through the cerebrospinal fluid system.
- Closed (occlusive) - disruption of the liquor flow is caused by pathologies of the ventricles: their adhesions, neoplasms.
The open form of childhood hydrocephalus can be either external or internal. But occlusal in 99% of cases is internal.
In addition, dropsy is also divided according to the form of its flow:
- Acute – a rapid increase in intracranial pressure, the baby’s condition worsens in the period from one to three days.
- Subacute - normal circulation of cerebrospinal fluid is disrupted for three to six months, after which severe brain damage occurs.
- Chronic – the development of the disease also lasts up to six months, but there is no such serious damage to the brain. Characteristic of open hydrocephalus.
Can hydrocephalus be cured?
Modern methods make it possible to normalize the outflow of cerebrospinal fluid from a congested brain or spinal cord by installing shunts - tubes that drain cerebrospinal fluid. Sometimes, with a mild form of the disease, this is enough to preserve the child’s intelligence. However, such a child will have to be home schooled, because... a minor head injury, which he easily receives at school, can be fatal. Such children also do not attend preschool institutions.
But in severe forms of the disease, manifested by a significant increase in head size, especially when combined with other developmental defects, the child’s physical and mental development inevitably suffers.
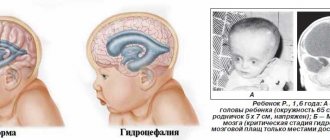
The growth of the head progresses after birth and it becomes very large with protruding external saphenous veins. Such children often have profound disabilities and cannot even care for themselves.
The most dangerous situation is when, already in utero, the child receives severe brain damage caused by increased intracerebral division. Children often suffer from visual impairment, hearing impairment, cerebral palsy, convulsive seizures, epilepsy, and attacks of uncontrollable headaches accompanied by vomiting. Most children, except those suffering from a mild form of hydrocephalus and receiving timely treatment, die before the age of 10 years.
Of course, the question of whether or not to leave a child with hydrocephalus depends on the degree of manifestation of the pathology, so the doctor, during an ultrasound of the fetus, will tell you what problems may arise and whether there is a chance for treatment and rehabilitation.
In the future, everything depends on the principles and financial capabilities of the family, because the treatment and recovery of such a child is expensive and not always promising. If the doctor insists on terminating the pregnancy, it is better to agree with him.
It is not uncommon for the birth of such a child to destroy a family. As a result, by the age of 6-10, the sick child still died, but at the same time other children suffered, deprived of the care and attention of parents who were fully occupied with caring for a child with a high degree of disability.
How does the disease develop and what are the consequences?
The activity of the endocrine glands, which produce cerebrospinal fluid, is disrupted. As a result, there is too much cerebrospinal fluid, and the small body is unable to ensure its normal outflow. On the left of the diagram is a normal brain, and on the right is one affected by hydrocephalus.
Hydrocephalic babies are easily recognized by their disproportionately large heads. Water cannot compress and increases the volume of the skull, and since in children under one year old rigid connections between the cranial bones have not yet formed, the increase in volume of the head occurs unhindered.
When hydrocephalus of the brain develops in an older child, excess fluid manifests itself exclusively as damage to the central nervous system.
The disease is quite dangerous: the cerebrospinal fluid does not leave the head and begins to put pressure on the nervous tissue, destroying neural connections. Without proper treatment, this usually leads to swelling of the brain and ultimately the death of the child.
What is fetal hydrocephalus
Hydrocephalus is a pathological accumulation of transudate.
The condition is characterized by increased intracranial pressure. WARNING! The information on the site is provided for informational purposes and cannot be used to make a diagnosis or make treatment decisions. The disease develops due to exposure to an infectious pathogen or a number of third-party causes.
The disease is formed as follows:
- Excessive amounts of fluid drain from the spinal cord area;
- it begins to gradually accumulate in the brain.
Dropsy in pregnant women can occur due to the abnormal structure of the embryo at the stage of conception.
Pathology has several forms:
- primary;
- secondary.
The first type is a disease caused by congenital defects or genetic mutations. The secondary form develops as a result of exposure to infection.
Fetal hydrocephalus can be closed or open. Closed - when there is an obstacle to the drainage of fluid from the head.
Open - cerebrospinal fluid is not absorbed into the bloodstream, and its circulation in the brain is not impaired.
In addition to the acute and chronic course, doctors distinguish external, internal and mixed types of the disease.
Types and forms of internal hydrocephalus
Depending on the cause of the disease, two forms of hydrocephalus are distinguished - open, communicating and closed (occlusive). Open hydrocephalus occurs as a result of increased secretion or impaired absorption of cerebrospinal fluid. Closed hydrocephalus develops when the patency of the cerebrospinal fluid outflow tract is obstructed by a tumor, inflammatory infiltrate, or adhesions.
Internal non-occlusive hydrocephalus can be congenital or acquired. Congenital hydrocephalus occurs during intrauterine development of the fetus. Acquired hydrocephalus develops under the influence of various diseases and injuries after the birth of a child.
The acute form of hydrocephalus is characterized by the rapid onset of symptoms of the disease within 3 days. In the subacute course of the disease, the increase in signs of hydrocephalus continues up to 1 month from the onset of the disease. Chronic hydrocephalus can take anywhere from several weeks to six months to develop.
Depending on the rate of progression of the symptoms of the disease, 3 forms of internal hydrocephalus are distinguished:
- progressive or active – occurs with rapid accumulation of cerebrospinal fluid and severity of symptoms;
- stabilized or passive – signs of the disease do not increase;
- regressive - symptoms of the disease disappear without treatment.
Neurologists distinguish compensated, subcompensated and decompensated stages of hydrocephalus. Depending on the level of intracranial pressure, there are hypertensive (with increased cerebrospinal fluid pressure) and normotensive (with normal intracranial pressure) internal hydrocephalus. Internal asymmetric non-occlusive hydrocephalus is characterized by dilation of one ventricle; in the presence of symmetric hydrocephalus, both ventricles of the brain are dilated.
At-risk groups
Taking into account the causes of fetal pathologies, scientists have identified risk groups. Women from these groups come under the close attention of doctors due to the high likelihood of developing anomalies.
These include:
- women over 35 years of age;
- patients who already have children with congenital pathology;
- women with a history of miscarriage, premature birth, stillbirth or antenatal fetal death;
- couples with a family history;
- patients exposed to radiation or exposed to toxins at work.
In such cases, ultrasound is performed repeatedly - the doctor needs to examine the fetus in detail, evaluate its development over time in order to exclude congenital anomalies.
Symptoms
Failures in development do not affect the mother’s well-being in any way.
Pathology can be suspected only by increased activity and sudden freezing of the child. Signs of the onset of illness in a baby are:
- maternal drowsiness;
- her emotional stress;
- hypertension;
- headaches turning into migraines.
Hydrocephalus of the fetus during gestation is determined only by ultrasound diagnostics.
The main manifestation of the pathology is an overly large head of the child with a tendency to increase. This is very clearly visible on the monitor screen and photographs.
A situation is considered dangerous when the baby in utero suffers serious damage to the brain. They are caused by strong intracranial pressure.
During intrauterine development, many babies begin to suffer from seizures, cerebral palsy, and epileptic seizures.
Clinical manifestations of the disease in newborns are:
- anxiety, irritability, tearfulness, increased drowsiness;
- lack of appetite;
- increased muscle tone;
- the pupil is located close to the lower eyelid;
- vomiting, constant regurgitation;
- rapid decrease in body weight;
- convulsions.
With hydrocephalus, symptoms appear gradually. The disease is characterized by the occurrence of acute phases, respiratory failure occurs - a condition that threatens the baby’s life.
If a child has a seizure, immediate medical attention is required.
How does hydrocephalus manifest?
Depending on the form of development of the pathology and the age of the child, the external signs of the disease change.
For children under two years of age, in which in 95% of cases hydrocephalus is a congenital pathology, the following symptoms are characteristic:
- Severe course of the disease. A rapidly deteriorating condition caused by damage to brain structures.
- The main symptom is a rapid increase in head volume. Growth of 1.5 cm or more every month is typical, for at least three months in a row. Starting from the ninth month of life, growth drops to 8-9 mm.
- A child is born with a head whose girth is larger than the girth of the chest. If by six months the ratio does not change, and the head is still larger than the chest, there is reason to suspect hydrocephalus.
- The veins on the occipital, temporal and frontal parts of the head are clearly visible.
- At three months the child does not yet hold his head up and begins to sit up late, crawl, and walk.
- The fontanel on the top of the head is convex.
- The accumulation of cerebrospinal fluid primarily occurs in the frontal lobes of the brain. Head enlargement starts from the forehead.
- While fixating the baby's gaze, the baby's pupil twitches chaotically.
- The scalp becomes thin and has a painful shine.
- Overhang of the brow ridges over the facial bone - the eyes appear to be very deep-set.
A number of less characteristic signs can confuse the initial diagnosis of hydrocephalus in children and complicate treatment. For example, tearfulness, poor appetite, slow weight gain, frequent regurgitation, drowsiness, legs constantly bent at the knees, head tilting - all these symptoms are characteristic of hydrocephalus. But at the same time, they can be observed in dozens of other childhood diagnoses.
In the acute form of dropsy, when the disease progresses rapidly, other signs can be observed:
- convulsions;
- long cry on one note;
- loss of acquired physical skills (sitting, following other people's movements, vocal functions);
- vomit.
For children aged two years and older, other manifestations of hydrocephalus of the brain are typical:
- Headaches that begin in the morning (after sleep) and gradually subside in the evening. Nausea and vomiting often begin at the same time.
- Migraines that appear after stress, mental or physical work. Often accompanied by nosebleeds.
- A feeling of a rush to the head when bending over and bursting headaches.
- Pain in the fundus of the eye.
- Visual impairment: loss of sharpness, double vision.
- Urinary incontinence.
- Decreased muscle strength, accompanied by rapid fatigue.
- Cramps and fainting.
- Loss of coordination and uncontrolled movements of the limbs.
Risk factors
There are accompanying conditions that contribute to the development of hydrocephalus of the brain in a child:
- Early birth (gestation period did not exceed 34 weeks).
- A narrow maternal pelvis and, as a result, a difficult birth process.
- The newborn's light weight is less than one and a half kilograms.
- During childbirth, hypoxia or asphyxia was observed in the fetus.
- Active methods of obstetrics: manual techniques, vacuum, forceps.
- The mother suffered viral infections during pregnancy: herpes, influenza, ARVI, toxoplasmosis.
- Bad habits of the mother that manifested themselves during pregnancy.
- Untreated sexually transmitted diseases in the mother during pregnancy.
Most risk factors for hydrops are related to maternal health.
Even indirect reasons, such as a premature baby with low weight, indicate an abnormal pregnancy. Every problem with a woman’s health during pregnancy weakens the embryo’s body.