Find out more about nervous diseases starting with the letter “N”: Sleep disturbance; Narcolepsy; Hereditary cerebellar ataxia of Pierre-Marie; Spinal circulatory disorders; Trigeminal neuralgia; Neuralgia of the submandibular and sublingual nodes; Neuralgia of the glossopharyngeal node; Neuralgia of the ear ganglion; Neurasthenia; Neural amyotrophy of Charcot-Marie-Tooth; Acoustic neuroma; Neuroma; Optic neuritis; Pharyngeal neuritis; Neuritis of the facial nerve; Neuritis; Obsessive-compulsive neurosis; Pharyngeal neurosis; Neuroses; Neurosis-like stuttering; Femoral nerve neuropathy.
Femoral nerve neuropathy is an injury to the most powerful nerve in the lumbar region, has various origins, causing pathologies in the penetration of nerve signals. Symptoms depend on the type of injury, appearing in the form of pain, sensory disturbances in the lower extremity, mainly in the anteromedial areas of the thigh and lower leg. Gait disorders occur due to difficulties in knee extension.
The diagnosis is made based on ultrasound of the femoral nerve and EMG. The therapy is complex and is aimed at eliminating nerve compression and inflammation, relieving pain and swelling, restoring innervation and metabolism. A course of electrical stimulation therapy and physical therapy is required.
general information
In 1822, the disease was described for the first time as anterior crural neuritis. Inflammation of the femoral nerve has been studied for almost 200 years, but remains poorly understood. Among mononeurotic pathologies, femoral neuritis is more common than others. The lack of complete information on this type of neurological disorders leads to the fact that the disease cannot be differentiated from radicular syndrome or myelopathy. Difficulties arise due to the variability of clinical symptoms from sensory distortions to movement disorders, depending on etiological factors.
Features of the anatomical structure of the femoral nerve
The lumbar processes of the spinal nerves arise at the level of L2, L3, L4 and merge into a single nerve trunk - the femoral nerve. N. femoralis passes between the iliacus and psoas major muscles, descends to the inguinal ligament and extends to the anterior thigh. Here there is a division into cutaneous, muscle branches and subdermal nerve. The femoral nerve innervates the muscle tissues through which it passes. Muscle functions include flexion and rotation of the hip, and with a stable hip, lumbar flexion and forward bending.
The processes coming from the femoral nerve under the inguinal ligament provide innervation to the hip flexor and knee extensor muscles. Dermal processes guarantee sensitivity of the frontal and part of the inner thigh. The subdermal nerve is the longest, exits in the area of the inguinal ligament, then along the anterior surface of the thigh enters the muscular canal and follows along the medial edge of the knee with the origin of the infrapatellar branch, with innervation of the anterior part of the patella.
Then the subcutaneous branch goes along the median surface area of the leg, foot - to the beginning of the big toe. It provides sensory sensation to the anterior and middle surfaces of the lower leg and the medial part of the foot.
Etiology
Neuritis is an imbalance of the nervous system and physical body. Therefore, the causes of the disease can be both physiological and emotional :
- injuries (bruise, dislocation, fracture) in the hip area;
- hypothermia;
- excessive physical activity;
- inflammation of the pelvic organs (bladder, prostate, rectum, ovaries, uterus);
- diabetes mellitus – causes blood flow disturbances and impairs nerve nutrition;
- infectious and viral diseases (influenza, herpes, measles, diphtheria, malaria, etc.);
- dysproteinemia – a violation of the protein ratio in the blood serum;
- lack of certain vitamins (especially group B);
- vasculitis - an inflammatory process in blood vessels;
- numbness of the thigh;
- physiological features of body structure;
- compression of the femoral nerve trunk. The reasons may be: staying in an uncomfortable position for a long time, pinched nerve due to a vertebral hernia, surgery;
- nervous tension, stress;
- pregnancy - as venous congestion occurs in the pelvic organs.
In general terms, neuritis is caused by: pinched nerve, compression, damage, disruption of the supply of nutrients, damage by various viral and infectious pathogens.
Factors in the formation of the disease
Muscle spasms, injuries and hemorrhages in the psoas muscle lead to compression of the femoral nerve at the iliopsoas border. The cause of compression may be abdominal tumors or hematomas. Hematomas are the result of thrombocytopenia, hemophilia, complications during treatment with anticoagulants in patients with thrombosis, and abdominal aortic aneurysm. Femoral nerve neuropathy can result from damage to the nerve during operations for appendicitis, on the ureters and kidneys, with abscesses of the iliopsoas muscles, and bursitis.
Compression of the femoral nerve in the groin area is caused by femoral hernias, lymphogranulomatosis inguinal, or prolonged forced positioning of the hip. The condition of neuritis occurs as a complication after operations on the hip joint, surgical treatment of inguinal hernias.
In the area of Gunther's canal, femoral neuropathy occurs when the adductor muscles are tense during sports or professional work. Pathologies and instability of the knee joint can also cause muscle tension. The result of knee surgery is iatrogenic femoral neuropathy. Neuropathy of the infrapatellar part of the femoral nerve is associated with the development of thrombophlebitis, varicose veins, and knee injuries.
Clinical manifestations
Symptoms of the disease depend on the cause of the condition. If the process taking place in the iliopsoas region, motor, sensory and vegetative-dystrophic disorders develop throughout the entire innervation zone. Impairments may occur alone or as a combined combination of motor and sensory impairments.
Absolute neuropathy is accompanied by disruptions in the activity of the iliopsoas muscles due to the possibility of alternative innervation. The ability to rotate and flex the hip is maintained. The decrease in the potential of the quadriceps extensor muscle of the knee joint is significantly pronounced. The patient strives to keep his leg straight even while walking.
It is difficult to walk, especially up the stairs, as well as running. There is a change in gait. The lower limb on the corresponding side is stable in the hyperextension position. There is no knee reflex. Tactile and pain sensations are impaired in the anterior inner area of the thigh and lower leg, and the medial area of the foot.
The process is expressed in the form of trophic and vegetative disorders, pain of an irrigation nature. The Wasserman symptom is pronounced - lying on the stomach, the patient experiences pain in the anterior part of the thigh when trying to raise the straightened leg to the maximum height, as well as the Mickiewicz symptom - the inability to bend the leg at the knee joint.
If the process takes place in the inguinal ligament area, the symptoms are similar to those described above. The most common motor disorders are those accompanied by pain when pressing on the inguinal ligament. Compression of the femoral nerve shaft in Gunther's canal is accompanied by pain and numbness of the skin of the central part of the knee joint, the anterior inner surface of the leg and the inner part of the foot.
Spontaneously occurring pain and paresthesia intensify with extension of the leg. The patient keeps his legs bent in a standing position and when walking. The knee reflex is preserved. Tinel's symptom is clearly expressed - when tapped with a hammer, paresthesia passes along the saphenous nerve, significant pain is detected at the site where the nerve exits the conductive canal.
Diagnostics
For an accurate diagnosis, it is important to determine the cause of neuropathy. The conclusion is made by a neurologist after carefully collecting anamnesis and studying the results of instrumental research methods. X-ray of the spinal column is not a reliable diagnostic method, since identified spinal defects do not exclude the manifestation of neuropathy. EMG allows you to resolve controversial issues in making a diagnosis.
Neuropathy corresponds to the slow passage of impulses along the femoral nerve column, a decrease in the amplitude of the M-response, symptoms of impaired innervation in the corresponding muscles, as well as the muscles of the L2-L4 segments. Using ultrasound diagnostics, the integrity of the femoral nerve is traced, pathological neoplasms, swelling, adhesive-scar changes and degenerative phenomena are determined. The level of nerve mobility in the adductor canal is confirmed by ultrasound with dynamic tests.
Differential diagnosis is aimed at excluding radiculopathies of the lumbar vertebrae of vertebrogenic origin, lumbosacral plexopathy caused by diabetes mellitus, injuries and gonarthrosis of the knee joint. To differentiate diseases of the abdominal cavity, ultrasound, MRI or CT are performed.
Prevention
The patient must take preventive measures that will help avoid relapse or the occurrence of a dangerous disease. They include enriching the diet with vitamins, regular monitoring of blood sugar levels, and complete cessation of smoking, drugs and alcoholic beverages.
To prevent the disease, it is recommended:
- wear comfortable shoes that do not pinch the foot, impairing blood flow;
- regularly inspect your shoes to avoid the formation of fungus;
- avoid walking long distances;
- do not stand in one place for a long time;
- wash your feet with cool water or do contrast baths, which helps improve blood circulation in the body.
Victims in remission are strictly prohibited from taking medications without the consent of the attending physician. It is important to promptly treat inflammatory diseases, take precautions when working with toxic substances that have a detrimental effect on the body, and regularly perform therapeutic physical exercises.
Treatment
If the femoral column is compressed by abdominal tumors, surgical intervention is performed urgently. If a traumatic violation of the integrity of the nerve with interruption of its fibers is confirmed, surgical treatment is also performed. For other established causes of the pathology, conservative treatment is carried out aimed at eliminating swelling, restoring blood supply, metabolism of the femoral nerve, and eliminating pain.
Glucocorticoid drugs are prescribed for decongestant and anti-inflammatory purposes when the nerve fiber is compressed under the inguinal ligament or in the muscle canals. Blockades are performed in the compression zone with solutions of glucocorticoid drugs (hydrocortisone, diprospan) in a cocktail with local anesthetics (solutions of lidocaine, novocaine).
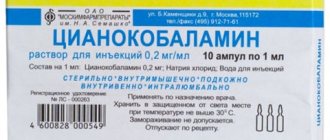
If nonsteroidal anti-inflammatory drugs in combination with analgesics do not relieve intense pain, treatment is supplemented with antidepressants (amitriptyline) and anticonvulsants (pregabalin, topiramate, gabapentin). To restore the normal functioning of the femoral nerve, it is advisable to prescribe medications to improve blood supply to nerve cells (nicotinic acid, pentoxifylline) and drugs that improve tissue metabolism (combined forms of vitamins B6, B1).
To prevent muscle contractures and atrophies in cases of detected paresis of the quadriceps muscle and lumbosacral muscles, it is advisable to prescribe a complex of exercise therapy, electrical stimulation physiotherapy, and prescribe medications that restore the transmission of neuromuscular impulses (ipidacrine, neostigmine).
Causes
The most common causes of axonal polyneuropathy of the lower extremities:
- exhaustion of the body;
- long-term deficiency of B vitamins;
- ailments leading to dystrophy;
- acute infections;
- toxic damage from mercury, lead, cadmium, carbon monoxide, alcoholic beverages, methyl alcohol, organophosphorus compounds, medications taken without the consent of a doctor;
- diseases of the cardiovascular, hematopoietic, circulatory and lymphatic systems;
- endocrinological pathologies, including insulin dependence.
The main factors that provoke the development of motor or sensorimotor axonal polyneuropathy are:
- endogenous intoxication in renal failure;
- autoimmune processes occurring in the body;
- amyloidosis;
- inhalation of toxic substances or vapors.
The disease can also be caused by heredity.
A lack of B vitamins in the body, and especially pyridoxine and cyanocobalamin, has an extremely negative effect on the conductivity of nerve and motor fibers and can cause sensory axonal polyneuropathy of the lower extremities. The same happens with chronic alcohol intoxication, helminthic infestation, and diseases of the gastrointestinal tract, which impair the rate of absorption.
Toxic poisoning with drugs, aminoglycosides, gold salts and bismuth occupy a large percentage in the structure of factors of axonal neuropathy.
In patients with diabetes, peripheral nerve function is impaired due to the neurotoxicity of ketone bodies, i.e. metabolites of fatty acids. This happens due to the body’s inability to use glucose as the main source of energy. Therefore, fats are oxidized instead.
With autoimmune diseases occurring in the body, the human immune system attacks its own nerve fibers, perceiving them as a source of danger. This occurs due to a provocation of the immune system that occurs when taking immunostimulating medications and unconventional treatment methods carelessly. Therefore, in people who are prone to autoimmune diseases, the triggering factors for axonal polyneuropathy are:
- immunostimulants;
- vaccines;
- autohemotherapy.
With amyloidosis, a protein called amyloid accumulates in the body. It is this that disrupts the basic functions of nerve fibers.