Premenstrual syndrome (PMS) is a wide range of symptoms and discomfort associated with the menstrual cycle that often occurs in young and middle-aged women. These symptoms appear 1-2 weeks before menstruation and disappear immediately or 1-2 days after its onset. Three out of four women experience PMS at some point in their lives.
Symptoms of PMS can range from mild to very severe. These changes in physical and emotional well-being can affect a woman's lifestyle and relationships. To help control the impact of premenstrual syndrome on your life, consult a gynecologist who can advise you on various treatment options and lifestyle changes that can help you.
Causes of premenstrual syndrome
Premenstrual syndrome Modern medicine does not yet have complete information about the mechanism of premenstrual syndrome.
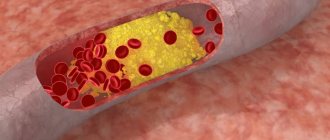
There are many theories describing the causes of PMS. First of all, hormonal changes and chemical processes in the brain are distinguished. The course of the menstrual cycle is regulated by hormonal fluctuations. Researchers believe that PMS symptoms may be associated with high levels of estrogen, prolactin and aldosterone, as well as progesterone deficiency.
Certain chemicals in the brain may also play a role in PMS. First of all, we are talking about serotonin, one of the main neurotransmitters. The concentration of this substance fluctuates during the menstrual cycle. Serotonin regulates mood, and when it is deficient, mood disorders and depression associated with PMS can occur. Low serotonin levels also cause fatigue, food cravings, and sleep problems.
Food preferences can also influence the course of PMS. Excessively salty and fatty foods, caffeine and alcohol consumption contribute to the aggravation of symptoms. Low levels of certain vitamins (such as vitamin B6) and minerals are also thought to contribute to PMS.
Women who are obese or who do little or no exercise are at higher risk for PMS. Those who smoke, suffer from thyroid disease, and have low blood sugar are also at risk.
Pathology of peri- and postmenopause
The share of postmenopausal osteoporosis among all forms of osteoporosis is 85%. The incidence of postmenopausal osteoporosis in developed countries among white women is 25-40%. Densitometric examination in accordance with WHO criteria revealed osteoporosis in 30.5-33.1% of women aged 50 years and older. The social significance of osteoporosis is determined by its consequences - fractures of the vertebrae and bones of the peripheral skeleton, which leads to an increase in morbidity, disability and mortality among older women. Among the urban population of Russia, 24% of women aged 50 years and older have at least one clinically significant fracture. In Russia, the annual incidence of fractures of the distal forearm in women over 50 years of age is 563.8 per 100,000 population of the same age, and of the proximal femur - 122.5 per 100,000. It is assumed that an increase in the life expectancy of women up to 80 years will lead to an increase the incidence of femoral neck fractures to 6.25/million in 2050 and will exceed the 1990 indicators (1.66/million) by more than 3 times.PREVENTION
The goal of preventing osteoporosis is to maintain bone density and prevent fractures. Primary prevention is aimed at creating and maintaining skeletal strength during various periods of a woman’s life (during the period of intensive growth and formation of peak bone mass, during pregnancy and lactation, and in the postmenopausal period).
Primary prevention includes:
- Healthy diet (foods high in calcium, avoiding excess protein intake).
- Active lifestyle and regular exercise.
- Maintaining optimal body weight.
- Adequate intake of calcium (up to 1000 mg/day) and vitamin D (400 IU/day) starting in early childhood.
- Providing the body with calcium during pregnancy and lactation (1200 mg/day).
- Providing the body with calcium (1000 mg/day) and vitamin D (800 IU/day) in peri and postmenopause.
- A healthy lifestyle (excluding smoking, alcohol consumption, coffee abuse, fasting and unbalanced diet).
- Adequate sun exposure.
Secondary prevention is aimed at preventing fractures in cases of already developed osteoporosis:
- Use of adequate doses of calcium and vitamin D supplements.
- Correction of estrogen deficiency conditions (amenorrhea, surgical and natural menopause, chemotherapy, radiation therapy to the pelvic area) using HRT as the first line of prevention of postmenopausal osteoporosis.
- The use of non-hormonal drug therapy for osteoporosis.
- Prevention of falls.
- Use of hip protectors and corsets.
- Correction of conditions and diseases that increase the risk of falls.
- Treatment of conditions that negatively affect bone metabolism.
- A healthy lifestyle, including moderate physical activity, a balanced diet, and the elimination of bad habits.
SCREENING
Key indicators for screening:
- age,
- presence of risk factors for fractures,
- history of fractures.
Dual-energy X-ray absorptiometry, or densitometry, evaluates bone health in the most important areas of the skeleton: the lumbar spine, proximal femur, and distal radius. It is used for screening and can detect a decrease in bone mineral density of 1-2%.
Indications for dual-energy X-ray absorptiometry:
- Women aged 65 years and older.
- Postmenopausal women under 65 years of age with risk factors.
- Fractures with minimal history of trauma.
- Diseases or conditions that lead to decreased bone mass.
- Taking medications that reduce bone mass.
CLASSIFICATION
There are primary (85%) and secondary (15%) osteoporosis.
Postmenopausal osteoporosis refers to primary osteoporosis (type I).
Primary osteoporosis:
- postmenopausal (type I);
- senile (type II);
- juvenile;
- idiopathic.
Secondary osteoporosis occurs against the background of the following conditions:
- endocrine diseases (hyperthyroidism, hyperparathyroidism, hypercortisolism, hypogonadism);
- gastrointestinal diseases, in which calcium absorption in the intestines decreases;
- long-term immobilization;
- chronic renal failure;
- diseases of the hematopoietic system;
- iatrogenic causes (long-term use of glucocorticoids, heparin, anticonvulsants, GnRH agonists);
- bad habits (alcohol abuse, coffee, smoking).
ETIOLOGY
Postmenopausal osteoporosis is a multifactorial disease. It is based on progressive bone loss that begins after menopause.
Risk factors for osteoporosis:
Unmodifiable:
- low bone mineral density;
- female;
- age over 65 years;
- Caucasian race;
- family history of osteoporosis and fractures with minimal trauma in relatives (mother, father, sisters) over the age of 50 years;
- hypogonadism;
- systemic use of glucocorticoids for more than three months;
- previous fractures;
- immobilization.
Modifiable risk factors:
- smoking;
- low physical activity;
- tendency to fall;
- insufficient calcium intake;
- vitamin D deficiency;
- alcohol abuse.
PATHOGENESIS
The mechanisms of the influence of sex hormones on bone tissue are not fully understood. However, it is known that these hormones, along with physical activity and good nutrition, are among the main factors determining the mass and quality of bone tissue. The role of sex hormones and their deficiency is especially important during puberty, reproductive and menopausal periods. During puberty, the production of sex hormones increases and the skeleton becomes the target of their action. Features of skeletal formation largely depend on the predominance of female or male sex hormones. Activation of bone metabolism manifests itself in a progressive increase in bone mass. Peak bone mass is reached between 20 and 30 years of age. Preservation of three main protective factors - physical activity, good nutrition and sufficient production of sex hormones - is a necessary condition for healthy aging of bone tissue, which begins after 40-45 years. In the first 5-10 years of natural menopause, there is a gradual decrease in the secretion of sex hormones. A decrease in estrogen levels leads to an acceleration of bone turnover and loss of bone matter (up to 3-5%/g). Peak bone mineral density and the rate of bone loss determine the risk of developing osteoporosis.
A drop in estrogen levels leads to an acceleration of bone metabolism due to increased resorption processes, which leads to a decrease in bone mineral density. Estrogens play a key role in the regulation of bone turnover, but the determining factors in this process are genetic.
CLINICAL PICTURE
The clinical picture of osteoporosis is quite poor, and in 1/2 of women it can be asymptomatic and clinically manifest as a fracture that occurs after a minor injury. The main complaints (regardless of the duration of menopause): pain in the sacrum and lumbar region that increases with physical activity and walking, general weakness, increased fatigue. Patients often indicate a feeling of heaviness between the shoulder blades and the need to rest during the day in a lying position. The pain syndrome intensifies as the disease progresses. Intense pain that does not stop with rest appears in the spine, pelvic area, and tibia. Often the cause of a sharp increase in pain is trabecular microfractures that occur after heavy lifting or awkward movement. The most common fractures are the thoracic and lumbar vertebrae, the distal radius, the ankles, and the proximal femur. As the disease progresses, deformation of the vertebral bodies occurs, muscle weakness increases, and posture is disrupted (kyphosis of the thoracic spine is formed). Vertebral fractures are accompanied by a decrease in height, decreased ability to work and the ability to self-care. Osteoporosis should be suspected if height decreases by more than 2 cm/year or 4 cm over a lifetime.
Studying the anamnesis is based on identifying risk factors for osteoporosis. Facts that may indicate osteoporosis:
- Decrease in height by more than 4 cm during life.
- Fractures with minimal history of trauma. (A minimal trauma fracture is defined as one that occurs spontaneously or from a fall from a height no higher than the person's own height, including fractures caused by coughing, sneezing, sudden movement, or lifting.)
- Chronic pain in the lumbar and thoracic spine, intensifying after physical activity or heavy lifting; bone pain.
- Kyphosis of the thoracic spine.
- Body mass index less than 19 (or body weight less than 57.7 kg).
- Estrogen deficiency conditions (amenorrhea, surgical and natural menopause).
The presence of causes leading to the development of secondary osteoporosis (taking drugs that affect bone metabolism; prolonged immobilization; diseases of the gastrointestinal tract).
Symptoms of premenstrual syndrome
The symptoms of premenstrual syndrome vary widely from person to person; Each woman may experience this condition differently. There are about 150 possible symptoms of PMS. They are divided into two groups: physical, emotional, the latter group also includes behavioral symptoms.
Premenstrual dysphoric disorder (PMDD) is particularly recognized as the most severe form of PMS. PMDD is characterized by more severe symptoms, primarily from the group of emotional and behavioral ones.
Physical symptoms
The most common physical symptoms are:
- feeling of fullness and bloating. You may feel a buildup of gas. Fluid retention is also possible;
- soreness of the mammary glands;
- intestinal disorder manifested by constipation or diarrhea;
- fatigue and increased fatigue;
- dizziness, nausea or vomiting;
- headache and back pain. There may also be muscle and joint pain. PMS can make migraines or asthma worse;
- increased sensitivity to noise and bright light;
- rapid heartbeat and increased sweating;
- skin symptoms such as acne or oily skin;
- discomfort in the pelvis and even pain.
Emotional and behavioral symptoms
First of all, the following emotional and behavioral symptoms are distinguished:
- atypical cravings for sweets;
- feelings of hopelessness and sadness;
- excessive tension, anxiety and nervousness;
- mood swings: bouts of tearfulness and outbursts of anger;
- loss or, conversely, increased sexual desire;
- self-esteem problems and feelings of guilt; some women may suffer from irrational and reinforced fears;
- sleep disturbances, which may manifest as difficulty falling asleep, interrupted sleep, or excessive sleepiness;
- slowness and lethargy of movements.
Treatment methods for premenstrual syndrome
You can do a lot on your own. You can achieve relief from the symptoms of premenstrual syndrome with simple measures such as:
- to drink a lot of water;
- Eat a balanced diet, choosing foods rich in fiber, vegetables and fruits, and low in salt, sugar and caffeine;
- exercise regularly;
- avoid lack of sleep and stress;
- do not drink alcohol.
It is not recommended to actively use painkillers without consulting a doctor.
Be sure to see your doctor if you are having a hard time with PMS and it is interfering with your daily life. In order for the doctor to receive the necessary amount of information, if possible, write down the symptoms of PMS, their frequency, severity and how you tolerate them. Three months' worth of entries will be sufficient.
In order to rule out conditions that may cause these symptoms, you may be prescribed laboratory and instrumental tests.
What your doctor can prescribe for you
Depending on your situation, you may be prescribed:
- vitamins and minerals (including B6, E, gamma-linolenic acid (GLA), calcium, magnesium), if there is reason to believe that the symptoms are associated with their deficiency;
- pain relievers such as aspirin, ibuprofen, and other nonsteroidal anti-inflammatory drugs (NSAIDs). They will help reduce headaches, back and muscle pain, breast tenderness and pelvic pain;
- diuretics (if there are problems with fluid removal). The use of these drugs reduces bloating, breast tenderness, and prevents weight gain (due to fluid during PMS, weight gain of up to 1 kg is possible);
- cognitive behavioral therapy. It will help you organize yourself and cope with your symptoms;
- antidepressants and anti-anxiety medications – to relieve the emotional symptoms of PMS;
- hormonal medications – to balance hormone levels.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
What to do when your period is late and the test is negative
If you feel nauseous in the morning, feel dizzy, experience fatigue, or have an uncharacteristically pronounced appetite, then it is best to buy a couple more tests and try again. If pregnancy is desired, then you should calm down, observe your body for several days and repeat the test. In cases where pregnancy is undesirable, it is best to make an appointment with a doctor; an ultrasound will accurately show the presence of pregnancy, because in such a situation you cannot hesitate. And a blood test, in comparison with a urine test, is more accurate and reliable, because it allows you to detect a minimal amount of the pregnancy hormone gonadotropin.