Today, the majority of patients of general practitioners are patients with vascular pathology, including neurological problems. But modern therapists do not know neurology well, and the therapist does not have enough time for a high-quality survey, examination and analysis of clinical data. Consequently, a clinic doctor must be able to identify situations when it is not necessary to deal with the patient on his own, but, without wasting time, refer him to a neurologist.
The outstanding neurologist of our time, academician Alexander Moiseevich Vein, said that it is necessary to engage in interdisciplinary medical practice, and not divide a person into parts that fall into the field of view of narrow specialists. Today there are no narrow-profile diseases, diseases of any particular organ or system. A person is one and is a complex organism, all parts of which are interconnected, therefore treatment requires a systemic, holistic approach.
These thoughts have come to life: general practitioners have appeared, they deal with comorbid patients, most of whom are represented by patients with vascular pathology, including neurological problems. However, as noted by the outstanding internist, Academician of the Russian Academy of Sciences V.S. Moiseev, today the situation is such that “modern therapists do not know neurology well for the reason that it has distanced itself, moved away from therapy, and set off on its own.”
Often in the clinic you can see patients visiting one office after another in the hope of getting the necessary help, and doctors who, experiencing diagnostic difficulties, do not know where to refer patients and where to start. Among the reasons for this situation, one can highlight the lack of sufficient time for a high-quality survey, examination and analysis of clinical data, and the impossibility, due to objective circumstances, of discussing problems with colleagues.
This leads to the prescription of numerous tests and often unnecessary medications, which ultimately lengthens the time for making a correct diagnosis. Consequently, a clinic doctor must be able to identify situations when it is not necessary to deal with the patient on his own, but, without wasting time, refer him to a neurologist.
There are 15 main neurological syndromes, upon identification of which the therapist should refer the patient to a neurologist:
- ✅ Back pain
- ✅ Temporary loss of consciousness
- ✅ Sudden dizziness
- ✅ Acute vestibular syndrome
- ✅ Sudden weakness in a limb or facial asymmetry
- ✅ Speech disorders
- ✅ Pain and numbness in the face
- ✅ Unsteadiness, swaying
- ✅ Memory impairment
- ✅ Numbness
- ✅ Sleep disorders
- ✅ Head or neck posture problems
- ✅ Difficulty writing
- ✅ Involuntary movements
- ✅ Tremor
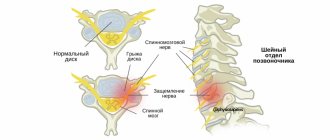
BACKACHE
Back pain is one of the most common situations when visiting a doctor. In Russia, patients traditionally turn to therapists, general practitioners and neurologists with this complaint. In foreign countries, there are different statistics, since back pain in the vast majority of cases is not a neurological problem. In Fig. Figure 1 presents an algorithm that reflects the necessary actions of a doctor in this syndrome. According to the algorithm, when a patient comes to an appointment with back pain, first of all it is necessary to exclude the so-called “red flags” that pose a threat to the health and life of the patient, which requires urgently referring the patient to a specialized specialist to provide specialized medical care.
"Red flags":
- ✅ connection of back pain with previous injury;
- ✅ irradiation of pain in the leg, feeling of numbness of the toes, weakness of the limb, the appearance of urinary and fecal incontinence;
- ✅ combination of pain with fever, leukocytosis, lymphadenopathy, acceleration of ESR, increased levels of C-reactive protein;
- ✅ unmotivated weight loss, anemia, fever;
- ✅ the appearance of pain at a young age, its duration and inflammatory nature: increased at rest, especially at night and in the morning, decreased during physical activity (warm-up);
- ✅ a history of diseases that may also be accompanied by acute back pain.
It is necessary to approach the diagnosis of the underlying disease very carefully, and it should begin not with an x-ray examination, not with a diagnosis of “osteochondrosis,” but with an assessment of the existing clinical symptoms.
For example, pain only at night, increased body temperature, anemia, accelerated ESR are manifestations of dangerous diseases, often leading to death. A thorough study of complaints, medical history, examination of the patient in combination with data from standard laboratory tests - a clinical blood test, including the mandatory determination of ESR, and a urine test - remain the basis for the initial diagnosis of a patient with back pain.
If “red flags” are excluded, a “multi-domain screening approach” is proposed, which involves assessing the patient’s pain and condition to create a personalized treatment program based on biopsychosocial analysis. In this case, to successfully diagnose the cause of chronic or recurrent pain, it is not enough to limit yourself to performing an X-ray examination, MRI or blood test, but it is necessary to conduct an in-depth analysis of the pain and characteristics of the social status of each individual patient.
The domains developed at the Department of Nervous Diseases of the First Moscow State Medical University are designed to help the clinic doctor quickly cope with the task in a short time for an outpatient appointment. I. M. Sechenov. This is a system of short questions and tests characterizing the pain pattern, which ultimately contributes to the selection of adequate therapy.
Currently, 10 domains have been proposed for a personalized therapy program: 5 for assessing the pain phenotype and 5 for assessing the patient’s social status.
To correctly select a drug or combination of drugs, the doctor’s task is to clarify the participation (“contribution”) of each domain in the formation of the sensation of pain.
For example, if we come to the conclusion that:
- Pain is associated with inflammation , then the drugs of choice are non-steroidal anti-inflammatory drugs (NSAIDs), because they act on the mechanisms of inflammation, especially acute ones.
- In chronic inflammation, chondroprotectors that act on cytokines activated during chronic pain come to the fore.
- For muscle spasms, muscle relaxants are needed.
- For myofascial syndrome, a set of measures is indicated: blockade of trigger points, dry puncture, taping, massage, manual therapy.
- Central sensitization has a very complex mechanism and is the hypersensitivity of central sensory neurons (allogenia, hyperalgesia, hyperpathia). In pharmacotherapy of this domain, drugs such as pregabalin, gabapentin are used, which close calcium channels, reduce the release of pain mediators, and reduce the excitability of central sensory neurons.
- The neuropathic domain (radiculopathy) is represented by pain associated with compression/damage of nerve fibers.
To diagnose this domain, it is important to have a certain clinical picture in combination with objective symptoms identified during examination.
Characteristics of pain associated with radiculopathy:
- ✅ burning, shooting character, reminiscent of an “electric shock”, with irradiation to the foot;
- ✅ combination of pain with other neurological symptoms (for example, tingling sensation, numbness, muscle weakness);
- ✅ the spread of pain along the corresponding dermatomes is typical.
Objective signs revealed during examination of the patient:
- ✅ neurological symptoms: hypoesthesia (decreased various types of sensitivity: temperature, pain, tactile, etc.);
- ✅ provocation of pain using motor tests (for example, the Lasegue symptom, which is considered positive if pain occurs when slowly lifting an outstretched leg with the patient in the supine position, associated with tension of the sciatic nerve).
Assessing the components of the patient’s social status domain, such as psychosocial factors, duration and quality of night sleep, physical activity, cognitive functions, the presence of comorbid pathology, especially if corrected, also helps eliminate chronic pain syndrome.
Thus, a personalized pain treatment program provides an individual approach.
Functional disorders in neurological practice
G.M. DUKOVA
, Doctor of Medical Sciences, Professor,
First Moscow State Medical University named after.
THEM. Sechenov The article discusses the main clinical manifestations, approaches to diagnosis and modern methods of treating functional disorders.
More than 30% of patients visiting a neurologist complain of somatic symptoms that cannot be explained by any organic disease [19, 20]. Such patients are often recommended expensive research and treatment, consultations with various specialists, which, as a rule, do not lead to a positive result, causing dissatisfaction for both the patient and the doctor [1]. The most common disorders in this category of patients are tension headaches and other chronic pain syndromes, conversion disorders, hyperventilation syndrome, dizziness, asthenia, depression, anxiety and somatoform disorders [16, 19].
In domestic medicine, such disorders are most often referred to as “vegetative dystonia syndrome” (G-90.9) or “astheno-neurotic reactions”; in therapeutic practice the term “neurocirculatory dystonia” is used. Some authors use the term “psychovegetative syndrome”, proposed in the 60s of the last century by German internists [2].
In foreign literature there is also no uniform terminology to refer to this group of disorders. In recent decades, authors have increasingly resorted to terms such as “medically unexplained symptoms” [18] or “subjective health complaints” [22], however, these are not satisfactory, because they are based not on positive, but on negative criteria.
Recently, it has been proposed to use the term “functional” and designate disorders in the somatic sphere with the term “functional somatic symptoms”, and in the neurological sphere with the term “functional neurological symptoms”. The advantage of this term is its “positive” meaning and patient acceptability, since dysfunction is emphasized, there is no definition of “unexplained” that worries the patient, as well as the mention of a psychogenic factor, which usually causes internal resistance of the patient, even if this is not realized by the patient.
Main clinical manifestations of functional disorders:
— Autonomic (permanent and paroxysmal) — Chronic pain syndromes — Motivational — Functional-neurological — Emotional-affective — Behavioral
Autonomic disorders
The main characteristic of autonomic disorders is their polysystemic nature. Table 1
The main manifestations of autonomic disorders are presented.
| Table 1. Clinical syndromes of autonomic disorders |
| Cardiovascular system: cardiorhythmic, cardiac, cardiosenestopathic syndromes, as well as arterial hypertension and hypotension or amphotonia. Respiratory system: hyperventilation disorders - a feeling of lack of air, shortness of breath, a feeling of suffocation, difficulty breathing. Gastrointestinal system: dyspeptic disorders (nausea, vomiting, dry mouth, belching, etc.), abdominal pain, flatulence, rumbling, constipation, diarrhea. Thermoregulation and sweating: non-infectious low-grade fever, periodic chills, diffuse or local hyperhidrosis. Vascular regulation: distal acrocyanosis and hypothermia, Raynaud's phenomenon, hot and cold flashes. Vestibular system: non-systemic dizziness, feelings of one’s own instability and instability of the surrounding world, a feeling of “lightheadedness”, pre-fainting states. Urogenital system: pollakiuria, cystalgia, itching and pain in the anogenital area, dyspareunia. |
Analysis of the semiotics of autonomic disorders requires determining the type of their course: permanent and/or paroxysmal. Permanent autonomic disorders mean subjective and objectively recorded disorders of autonomic functions that are permanent or occur sporadically. These disorders may manifest predominantly in one system or have a distinct multisystem nature.
Paroxysmal autonomic disorders, autonomic crises or panic attacks (PA) are the most striking and dramatic manifestation of the psychovegetative syndrome.
The following criteria are used to diagnose panic disorders:
1. Sudden, sometimes unexpected appearance of 4 or more symptoms: - vegetative (cardiovascular, respiratory, vasomotor, etc.); - vestibular (dizziness, instability, etc.) - emotional-affective (panic, fear, aggression, etc.) - dissociative (derealization, depersonalization) 2. Anticipation and repetition of these episodes 3. Constant worry about the consequences of attacks 4. Behavior changes in connection with panic attacks (agoraphobia and restrictive behavior) 5. The appearance of attacks regardless of any organic factor (for example, caffeine intoxication or hyperthyroidism).
Attacks consisting of several symptoms are called “abortive” or “minor”. If during an attack the patient experiences most of the above symptoms, then they speak of “extended”, “large” PA.
There are several types of PA depending on the dominant symptoms: respiratory, vestibular, cognitive and “non-insured”, as well as by the time of occurrence: night/day attacks [9].
Outside of attacks, agoraphobic syndrome is most often observed, which ultimately manifests itself as fear of a situation potentially threatening the development of PA and difficulty in obtaining medical care. Such situations can be being in a crowded room, in a store, transport, cinema, alone at home or in the country. Agoraphobia is the factor that determines the psychological and social consequences of PA, namely restrictive behavior and secondary depression. It is these consequences that are the target for therapeutic interventions (psychotherapy and psychopharmacotherapy).
Chronic pain syndromes
In clinical practice, chronic pain syndromes make up a significant proportion of patients. Beyond the clearly defined somatogenic and neuropathic pain, there are a variety of chronic pain syndromes labeled as “functional,” “medically unexplained,” “dysfunctional,” “somatoform,” “somatized,” “psychogenic,” etc.
Chronic pain syndromes observed in clinical practice
— Headaches — Atypical facial pain — Pain in the left side of the chest (“non-cardiac pain”) — Back pain — Abdominal pain — Pain in the lower abdomen (pelvic pain) — Anogenital pain — Pain throughout the body (fibromyalgia) Currently the above chronic pain syndromes of different localization, together with other symptoms (mental, autonomic, motivational and neuroendocrine) are regarded as functional based on common factors that are naturally observed in all these forms. These include: the frequent combination of different syndromes in the same patient, both simultaneously and sequentially, the predominance of women, emotional disorders and a history of childhood psychotrauma, the leading role in the pathogenesis of these syndromes of dysfunction of certain cerebral systems (limbic parts of the brain, prefrontal and parietal cortex ) and the therapeutic effectiveness of antidepressants.
Currently, there are 2 groups of factors that are involved in the chronicization of pain syndromes: biological and psychosocial, the structure of which is presented in Table 2
.
| Table 2. Biological and psychosocial factors of pain chronification | |
| Biological factors | Psychosocial factors |
| Genetically inherited features of nociceptive and antinociceptive systems | Psychogenic factors of childhood (physical, moral and sexual abuse) |
| Processes of peripheral and central sensitization, inflation (Wind-up) | Personality characteristics of patients (anxious suspiciousness, sensitivity, passive-aggressive traits, masochism, hypochondriasis, social dependence, pessimism, demonstrativeness) |
| Inclusion of muscle factor | Current stress and conflicts |
| Abuse factor (abuse of analgesics) | Rental installations |
| Availability of medical care | |
Diagnosis of chronic pain syndrome includes the following:
1. Exclusion of possible somatic (organic) factors causing pain. 2. Clarification of the temporal characteristics of pain. Duration of pain: most of the day, at least 15 days per month, lasting at least 6 months. 3. Qualitative characteristics of pain: monotonous pain, periodically intensifying before an attack, in the description of pain the use of non-pain terms (“cotton head”, “stuffiness” in the left half of the chest, “unpleasant tickling” in the lumbar region, etc.), senestopathic coloring of pain. 4. The localization of pain during examination and palpation is always much wider than the patient presents. 5. Painful behavior - marking a “sick” organ - immobilizing it, constantly rubbing the skin in the heart area, regularly taking analgesics, and if they have no effect, regularly calling an ambulance. 6. Psychogenesis of pain. Presence of close relatives suffering from pain. Often the patient himself experienced pain, or observed it in emotionally charged situations, for example, the death of a parent from a myocardial infarction with severe pain. 7. Beaten paths. Debut or exacerbation of chronic pain after injuries, surgical interventions, infectious diseases. 8. Syndromic environment, including psychovegetative and motivational disorders.
Functional neurological symptoms
This term refers to neurological symptoms that do not have an underlying organic cause. In the practice of a neurologist, such symptoms account for up to 19% of outpatient visits [16] and 9% of hospitalized patients [10]. In modern classifications, they belong to the headings of “dissociative (conversion)” disorders in ICD-10 or “somatoform” disorders in DSM-IV.
The clinical phenomenology of functional neurological disorders (FNS) is presented as follows:
1. Paralysis and paresis 2. Paroxysmal disorders (seizures) 3. Gait disorders 4. Sensory disorders 5. Visual and oculomotor disorders 6. Dyskinesia 7. Speech and voice disorders 8. Impairments of consciousness 9. Cognitive impairments
Functional neurological disorders can be observed both in the structure of PA and in the permanent version. A special study showed that in the structure of a typical panic attack, up to 30% of symptoms can be classified as FNS [23]. Often they are the subject of special concern for relatives and diagnostic errors of doctors.
Diagnosis of these disorders requires special awareness of the typical neurological manifestations of hysteria, as well as the use of specific tests and samples [25, 21].
Violation of biological motivations
There are 4 basic biological motivations that are basic for preserving life, the full functioning of the body and procreation. These include the need for food intake, the need for sleep and sexual activity. Separate and important for human existence is the need for activity, action, participation in society, etc. The mechanisms of motivation at the cerebral level are primarily associated with the activity of the limbic-reticular complex systems, which regulate adaptive behavior in response to any type of stress.
With functional disorders, disturbances occur in the sphere of motivation. Their syndrology is presented below:
— Eating disorders (anorexia with weight loss or bulimia with weight gain) — Dissomnia disorders (difficulty falling asleep, early awakenings, shallow sleep, hypersomnia, parasomnia) — Sexual disorders (decreased libido, potency, anorgasmia, etc.) — Asthenia (weakness, fatigue) As a rule, patients do not focus attention on them, but with active questioning it is possible to reveal that “there is no appetite, and even the smell of food causes nausea” or, conversely, “you constantly want to eat and even have to get up at night to do this” , patients often talk about certain sleep disorders. Problems in the area of intimate life often appear before the onset of the disease, and during the course of the disease, sometimes sexual life “comes to naught.”
Separately, it is necessary to dwell on the violation of motivation for activity. Clinically, this manifests itself as asthenic syndrome. Asthenic syndrome is one of the most common syndromes in the clinical practice of any doctor. The key words in asthenia are “weakness” and “fatigue,” which are characterized by the fact that they occur not only with exertion, but also without it, and do not go away after rest. Since the feeling of fatigue is a key trigger for rest, the essence and meaning of the feeling of fatigue and weariness is an urge to stop activity, activity, any effort, etc. Reducing activity is a universal psychophysiological mechanism for preserving the vital activity of the system in the event of any threatening situation, operating according to the principle : less activity means less energy requirement. With asthenia, not only the real threat of depletion of energy reserves, but also an imaginary threat (emotional overstrain, stress, conflicts) are triggers for feelings of fatigue and weakness. It has been shown that changes in the sphere of motivation are key to the formation of asthenia in humans [26, 27, 6].
Emotional, affective and behavioral disorders
Patients with functional disorders usually turn to a neurologist with specific somatic complaints, such as pain, dizziness, shortness of breath, lump in the throat, sleep disturbances, etc. and, as a rule, do not complain about emotional disorders and do not associate symptoms that worry them with them. Moreover, they regard even fear in the structure of PA as secondary to “increased pressure,” “choking,” “palpitations,” or “dizziness.” This is what causes misdiagnosis and inadequate treatment. The identification of emotional disorders is complicated by the alexithymia inherent in such patients. Alexithymia refers to the patient’s difficulty in recognizing, expressing and describing (verbalizing) his own feelings, state of mind and emotions experienced by himself or other people, as well as difficulties in distinguishing between emotions and bodily sensations. Psychometric tests are usually used to identify emotional disorders and alexithymia. However, clinically it is also possible to get an idea of the patient’s disturbing thoughts, threats, perceptions and associated emotions. To do this, it is enough to purposefully ask the patient how he behaves at the moment the symptom appears, in what situation the symptom appears, how the symptom affects his physical and social functioning, what actions the patient takes to avoid the “consequences of the disease” he imagines. It is often possible to identify distinct restrictive behavior, repeated tests that bring relief for a short time, obsessive rituals (constant measurement of blood pressure, precautionary use of painkillers), etc.
Thus, in the practice of a neurologist, many patients experience a variety of autonomic, neurological, motivational and behavioral disorders, in which all available research methods do not reveal an organic cause and which today are designated as functional disorders.
Therapy for functional disorders
The vast majority of patients with functional disorders are observed and treated either by neurologists or general practitioners. The dominance of asthenia, pain and autonomic syndromes in the clinical picture, the hidden nature of emotional disorders often prompts doctors to use predominantly somatotropic drugs in therapy: antihypertensive and vegetotropic drugs, analgesics, vascular-metabolic therapy, antioxidants, adaptogens, etc. And only in the case of obvious For emotional disorders, tranquilizers may be included in therapy. Such therapy often turns out to be ineffective, undermining the patient’s faith in the possibility of a cure and contributing to the chronicity of the process.
Already at the first contact, the doctor must determine the further strategy for managing the patient. At the first stage, it is absolutely necessary to exclude an organic disease, which can manifest itself with similar symptoms. A detailed clinical and paraclinical examination of the patient also has a psychotherapeutic value, showing the seriousness of the doctor’s attitude towards the patient and objectively convincing the patient of the absence of a threatening disease.
Despite the fact that pain and autonomic disorders are the most obvious in the clinical picture, psychopharmacology is currently the basic method of treatment. Psychotherapy also plays a significant role.
The main goals of therapy for functional disorders are:
1. Relief of the leading symptom or syndrome 2. Impact on secondary syndromes (agoraphobia, depression, anxiety, asthenia). 3. Prevention of relapses and further progression of the disease. For this purpose, symptomatic, pathogenetic and preventive therapy is used. Sometimes an explanatory conversation with a doctor about the essence of the disease, possibly in combination with placebo therapy, is sufficient. Our studies have shown that in 35-42% of patients suffering from panic disorder, significant improvement was achieved only with the help of placebo therapy [4].
Symptomatic therapy
aimed at quickly relieving the leading symptom. This stage of therapy has several goals. Firstly, rapid relief of the patient’s condition, which in itself has a psychotherapeutic effect, since it removes the fear of a threatened and incurable disease. Secondly, relief of the leading symptom prevents the process from becoming chronic. Thus, rapid and early relief of acute back pain prevents the development of persistent muscle spasm, which is an important pathogenetic mechanism for the formation of chronic back pain. Early and successful relief of panic attacks prevents the development of agoraphobic syndrome and restrictive behavior, which are the main factors of social disability in patients with panic disorders.
Symptomatic therapy can be represented by a variety of techniques. Thus, to relieve hyperventilation disorders, it is advisable to teach the patient breathing exercises, which he can use both to relieve panic attacks and to correct respiratory disorders outside of an attack. For most functional symptoms, pharmacological drugs are used as symptomatic therapy - the so-called “treatment on demand”: to relieve nausea - prokinetics (cerucal), to reduce tachycardia - beta-blockers, to relieve pain - non-steroidal anti-inflammatory drugs and muscle relaxants, for relief paroxysms (panic attacks) - tranquilizers. It is necessary to remember and explain to the patient that this treatment operates on the “here and now” principle and is a short-term therapy, which will be canceled as the main pathogenetic therapy takes effect. Moreover, the patient’s healing process is characterized by a decrease in the need for these “life-saving” drugs. Often the patient himself does not yet realize a noticeable improvement in his condition, and the doctor can make him understand this if in a conversation he focuses the patient’s attention on the number of symptomatic medications taken in the last week. Thus, the effectiveness of pathogenetic therapy is substantively proven to the patient.
Pathogenetic therapy
is focused on preventing the reappearance of paroxysmal manifestations (panic attacks, psychogenic seizures, pain attacks, etc.), regression of the abusive factor, relief of anticipation anxiety, agoraphobic syndrome and restrictive behavior, secondary depression, asthenia and other motivational disorders.
Therapy aimed at the formation of new patterns and stereotypes
of motor behavior, cognitive aspects of thinking, motivation, emotional-affective and behavioral reactions is important.
Numerous multicenter placebo-controlled studies have shown that antidepressants (ADs) are the basic drugs in the treatment of functional disorders. It has been found that AD can be effective in chronic pain syndromes of various localizations [3], panic disorders [8, 7, 17], asthenia [15] and appetite disorders [11]. Moreover, ADs are effective regardless of whether these syndromes are combined with depression or not, and the doses used for the treatment of functional disorders are lower than for the treatment of depression.
It should be noted that the pronounced side effects of a number of ADs, in particular tricyclic ADs, significantly reduce the possibility of their use, especially in outpatient practice. Therefore, the drugs of first choice are currently drugs from the group of selective serotonin reuptake inhibitors - SSRIs (fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram and escitalopram).
Escitalopram belongs to the second generation of SSRIs, since it has a slightly different mechanism of action than other serotonergic antidepressants: it interacts not only with the primary binding locus of the serotonin transporter protein, but also with the secondary (allosteric) one, which leads to faster, more powerful and persistent blockade of serotonin reuptake due to the modulating effect of allosteric binding. At the same time, escitalopram is the most selective of the SSRI antidepressants, since it practically does not bind to serotonin (5-HT), dopamine (D-1 and D-2), α-adrenergic, histamine, m-cholinergic receptors, as well as benzodiazepine and opiate receptors. receptors [14].
M. Mazza et al. [12] revealed the effectiveness of escitalopram at a daily dose of 20 mg in the treatment of chronic lumbar pain. Therapy with escitalapram has been shown to be effective in patients with panic disorders [24]. Muller et al. studied the effectiveness of escitolapram in patients with “multisomatoform disorders,” which refers to “medically unexplained symptoms,” in a double-blind, placebo-controlled manner. At the 12th week of treatment, escitalopram was effective in 84.0% of patients, in contrast to 26.9% on placebo [13].
The most common side effects when taking escitalopram were nausea and headache, which were mild, transient and disappeared within 2-3 weeks. Escitalopram does not cause significant inhibition of the activity of the main isoenzymes of the cytochrome P 450 family in vitro, and therefore it is unlikely to be involved in clinically important pharmacokinetic drug interactions in patients.
Thus, high efficiency at a minimum dose, minor and quickly passing side effects, as well as the absence of drug interactions make escitalopram an indispensable drug in the treatment of elderly and somatically burdened patients. Treatment adherence in patients taking escitalopram is significantly higher than in similar studies with other antidepressants.
In 2014, a domestic generic version of escitalopram appeared on our market - the drug Asipi (JSC Veropharm). Based on comparative pharmacokinetics, it is shown that the drug Asipi is bioequivalent to the original drug Cipralex.
When determining the tactics of blood pressure therapy, it is necessary to resolve two main issues: choosing a drug and determining the dose.
The choice of drug is determined mainly by the clinical picture of the disease and the characteristics of the drug. When determining the dose of the drug, the following rules may be useful:
1. Taking into account the individual sensitivity and anxious suspiciousness of this category of patients, it is advisable to begin therapy with small doses (1/2-1/4 of the planned dose) with a gradual increase over 3-5 days. 2. The criterion for limiting the dose may be the severity of side effects that do not disappear within 3-5 days. 3. A daily distribution of the drug is recommended depending on the hypnogenic effect.
Before prescribing a course of drug therapy, the doctor must explain to the patient the basic principles of treatment and warn about possible difficulties in the treatment process. In this conversation, it is necessary to emphasize the following points:
1. The essence of the treatment is that it is aimed at preventing the recurrence of attacks and the social adaptation of the patient. 2. The effect of therapy may be delayed, since in most ADs the effect appears with a latent period of 14-21 days from the start of their use. 3. The course of treatment should be long, sometimes it can last up to a year. 4. Abrupt withdrawal of drugs at any stage of treatment can lead to exacerbation of the disease, therefore, at the end of treatment, drug withdrawal is carried out very gradually. Psychotherapeutic approaches to the treatment of functional disorders
can be conditionally divided into 3 types: 1) psychotherapy aimed at relieving individual symptoms and improving the general condition of the patient 2) aimed at pathogenetic mechanisms; 3) person-oriented (reconstructive) psychotherapy.
Symptomatic psychotherapy includes techniques aimed at influencing individual neurotic symptoms and the general condition of the patient. This is auto-training (in individual and group modes), hypnosis, suggestion and self-hypnosis. With the help of such techniques, anxiety is relieved, optimism and self-confidence are imparted, and the patient’s motivation for recovery is enhanced.
The second group includes cognitive behavioral psychotherapy, conditioned reflex techniques, body-oriented methods, and neurolinguistic programming. The main goal of cognitive behavioral therapy is to help the patient change the pathological perception and interpretation of painful sensations, since these factors play a significant role in the maintenance of symptoms. Cognitive behavioral therapy may also be useful in teaching the patient more effective coping strategies, which in turn may lead to increased adaptive capacity.
The third group consists of methods aimed directly at the etiological factor. The essence of these techniques is person-oriented psychotherapy with the reconstruction of the basic motivations of the individual. These techniques are aimed at revealing early childhood conflicts or current personality problems; their main goal is the reconstruction of personality. This group of methods includes psychodynamic therapy, Gestalt therapy, and family psychotherapy.
When functional disorders are combined with obvious hysterical, senesto-hypochondriacal, obsessive and/or phobic manifestations, small doses of antipsychotics are used as an addition to basic pharmacotherapy with antidepressants - Melleril (Sonapax), Theralen, Eglonil, Tiapridal, Chlorprothixene, Seroquel, Etaparazine, Neuleptil.
Non-drug therapy
Methods of non-drug therapy include information and educational programs, physical training, massage, therapeutic exercises, hydrotherapy (water gymnastics, swimming, contrast showers, Charcot shower), breathing exercises, acupuncture, complex treatment with thermo-, odorous, music and light effects carried out in a specially designed capsule, biofeedback methods, exposure to transcranial magnetic stimulation, etc. Thus, most modern researchers believe that physical activity is a priority in the treatment of asthenia. Empirical evidence and analysis of randomized controlled trials suggest that 12 weeks of graded exercise therapy, especially when accompanied by patient education programs, can significantly reduce feelings of fatigue and tiredness.
Thus, at present, a large group of patient complaints and physical symptoms are united on the basis of the absence of organic pathology and the presence of common pathophysiological mechanisms in their origin. Comprehensive treatment, in which the treatment of blood pressure is a priority, makes it possible to successfully cope with these socially disabling sufferings.
Literature
1. Barsky AJ, Orav EJ, Bates DW: Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Archives of General Psychiatry, 2005, 62: 903-910. 2. Delius L. Fahrenberg J. Psychovegetative Syndrome Thieme, 1966: 290. 3. Dharmshaktu P, Tayal V, Kalra BS. Efficacy of antidepressants as analgesics: a review. J Clin Pharmacol, 2012, 52(1): 6-17. Epub 2011 Mar 17. 4. Dyukova GM, Shepeleva IP, Vorob'eva OV. Treatment of vegetative crises (panic attacks). Neurosci Behav Physiol, 1992, 22(4): 343-5. 5. Fishbain D. Evidence-based data on pain relief with antidepressants. Ann Med, 2000, 32(5): 305-16. 6. Floris P de Lange, Joke S Kalkman, Gijs Bleijenberg, Peter Hagoort, Sieberen P vd Werf, Jos WM van der Meer and Ivan Toni Neural correlates of the chronic fatigue syndrome—an fMRI study. Brain, 2004, 127(9): 1948-1957. 7. Freire RC, Hallak JE, Crippa JA, Nardi AE. New treatment options for panic disorder: clinical trials from 2000 to 2010. Expert Opin Pharmacother, 2011, 12(9): 1419-28. 8. Gorman JM. The use of newer antidepressants for panic disorder. J Clin Psychiatry 1997, 58 Suppl 14:54-8; discussion 59. 9. Kircanski K. Craske MG, Epstein A. Wittchen HU. Subtypes of Panic Attacks: A critical review of the empirical literature. Depression and Anxiety, 2009, 26: 878–887. 10. Lempert T, Dieterich M, Huppert D, Brandt T. Psychogenic disorders in neurology. Frequency and clinical spectrum. Acta Neurol Scand 1990, 82: 335–340. 11. Leombruni P, Piero A, Lavagnino L, Brustolin A, Campisi S, Fassino S. A randomized, double-blind trial comparing sertraline and fluoxetine 6-month treatment in obese patients with binge eating disorder. Prog Neuropsychopharmacol Biol Psychiatry, 2008, 32(6): 1599–1605. 12. Mazza M, Mazza O, Pazzaglia C, Padua L, Mazza S. Escitalopram 20 mg versus duloxetine 60 mg for the treatment of chronic low back pain. Expert Opin Pharmacother, 2010, 11(7): 1049-52. 13. Muller JE, Wentzel I, Koen L, Niehausb DJH. Seedat S and Stein DJ. Escitalopram in the treatment of multisomatoform disorder: a double-blind, placebo-controlled trial. Int Clin Psychopharmacol 2008, 23: 43–48. 14. Owens MJ, Knight DL, Nemeroff CB. Second-generation SSRIs: human monoamine transporter binding profile of escitalopram and R-fluoxetine. Biol.Ps., 2001, 50: 345–50. 15. Pae CU, Marks DM, Patkar AA, Masand PS, Luyten P, Serretti A.Pharmacological treatment of chronic fatigue syndrome: focusing on the role of antidepressants. Expert Opin Pharmacother, 2009, 10(10): 1561-70. 16. Perkin GD. An analysis of 7836 successful new outpatient referrals. J Neurol Neurosurg Psychiatr 1989, 52:447-448. 17. Pollack MH, Allgulander C, Bandelow B, Cassano GB, Greist JH, Hollander E, Nutt DJ, Okasha A, Swinson RP; World Council of Anxiety. WCA recommendations for the long-term treatment of panic disorder. CNS Spectr, 2003, 8(8): 17-30. 18. Sharpe M, Mayou R, Bass C. Concepts, theories and terminology. In: Mayou R, Bass C, Sharpe M, eds. Treatment of functional somatic symptoms. Oxford: Oxford University Press, 1995: 3–16. 19. Stone J, Carson A, Duncan R, Coleman R, Roberts R, Warlow C, Hibberd C, Murray G, Cull R, Pelosi A, Cavanagh J, Matthews K, Goldbeck R, Smyth R, Walker J, MacMahon AD. Sharpe M. Symptoms 'unexplained by organic disease' in 1144 new neurology out-patients: how often does the diagnosis change at follow-up? Brain, 2009, 132: 2878–2888. 20. Stone J et al. “Who is referred to neurology clinics?—the diagnoses made in 3781 new patients.” Clin Neurol Neurosurg, 2010, 112(9): 747-51. 21. Stone J, Carson A, Sharpe M. Functional symptoms and signs in neurology: assessment and diagnosis. J Neurol Neurosurg Psychiatry 2005, 76: 2-12. 22. Ursin H, Eriksen HR. Sensitization, subjective health complaints, and sustained arousal. Ann NY Acad Sci 2001, 933: 119-29. 23. Vein AM, Dyukova GM, Vorobieva OV. Is panic attack a mask of psychogenic seizures? A comparative analysis of phenomenology of psychogenic seizures and panic attacks. Functional neurology, 1994, IX(3): 153-161. 24. Waugh J, Goa KL. Escitalopram: a review of its use in the management of major depressive and anxiety disorders. CNS Drugs, 2003, 17(5): 343-62. 25. Dyukova G. M. Basic principles for diagnosing hysteria in neurology. Selected lectures. Eidos-Media, 2006: 316-337. 26. Kulikovsky V.V. Clinical and pathogenetic aspects of asthenic syndrome of psychogenic and somatogenic genesis. Moscow, 1994. Diss. doc. med. sc. P. 482. 27. Rodshtat I.V. Questions of the clinic and pathogenesis of asthenic conditions (neurological and psychological analysis). M. Diss. Ph.D. med. sc. 1967. P. 265.
Source
: Medical Council, No. 5, 2015
TEMPORARY LOSS OF CONSCIOUSNESS
Short-term loss of consciousness can be caused by many reasons, which are within the competence of different specialists: cardiologists, therapists, neurologists, endocrinologists, gynecologists, etc., however, neurological diseases can be a common cause of fainting.
Thus, a mandatory indication for consultation with a neurologist is attacks of loss of consciousness, accompanied by signs characteristic of epilepsy (sudden onset, convulsions, tongue biting, loss of urine, disorientation).
A transient ischemic attack (TIA) may manifest as a short-term loss of consciousness. It should be noted that convulsive twitching can occur in patients with vasovagal syncope that occurs against the background of emotional stress and orthostatic load. Such patients do not need to consult a neurologist.
Considering the fact that loss of consciousness before finding out its cause poses a threat to the patient’s life, a mandatory consultation with a neurologist is necessary.
Diseases of the nervous system and their symptoms
Neurologists often have to treat migraines, neuralgia, neuritis, vegetative-vascular dystonia, neuroses, and neuropathies. They are treated with Alzheimer's disease, Parkinson's disease, cerebral palsy, degenerative diseases of the spine, epilepsy, and insomnia. Specialists diagnose and treat encephalitis, meningitis, epilepsy, consequences of stroke, and head injury.
Diseases of the nervous system manifest themselves in a number of syndromes:
- vegetative (dizziness, breathing problems, tachycardia, changes in blood pressure);
- motor (tremors, convulsions, paralysis, paresis, numbness of body parts);
- pain (headache, discomfort in the heart, neuralgia);
- general (increased fatigue, decreased performance, deterioration of memory and concentration, hearing and vision impairment, loss of consciousness, nausea, vomiting, bowel disorders, problems falling asleep and waking up at night, tinnitus, mood swings, speech disorders, panic attacks, phobias) .
SUDDEN Dizziness
Referral to a neurologist requires sudden onset of dizziness in combination with focal neurological disorders, such as ataxia, deafness, vertical or rotational nystagmus, etc., which may be a manifestation of TIA or stroke.
It should be noted that isolated dizziness without the listed neurological disorders is a symptom of more than 80 diseases and is an interdisciplinary problem dealt with by doctors of various specialties: therapists, otolaryngologists, otoneurologists, neurosurgeons, etc. This is also due to the fact that the word “dizziness” » The patient often understands completely different sensations, such as staggering and unsteadiness.
ACUTE VESTIBULAR SYNDROME
As a rule, it is a manifestation of peripheral dizziness and is associated with vestibular neuronitis, but in rare cases this syndrome (dizziness, nausea, vomiting, gait instability (dysbasia)) can be a manifestation of a stroke.
Therefore, adults with sudden-onset acute vestibular syndrome should have the HINTS test performed without attempting to self-administer any symptomatic medications. If it turns out to be positive, immediate neuroimaging and consultation with a neurologist is required to rule out stroke.
Causes of the disease
The contribution of a number of factors to the development of post-coronavirus syndrome is currently being discussed:
- long-term persistence of SARS-Cov-2 (the causative agent of COVID-19) in the human body with the development of a direct cytopathic effect on cells and tissues;
- immunological disorders and excessive inflammatory response directed against SARS-Cov-2;
- post-resuscitation syndrome is a set of pathological changes that developed as a consequence of severe acute coronavirus infection in patients receiving inpatient treatment in the intensive care unit.
Despite the fact that one of the significant risk factors for the development of post-coronavirus syndrome is the severe course of acute COVID-19, it should be noted that it also often develops after a mild course of acute coronavirus infection that did not require hospitalization of the patient in a hospital.
SUDDEN LIMB WEAKNESS AND FACIAL ASYMMETRY
Sudden or increasing facial asymmetry in combination with arm weakness and speech impairment first of all requires the exclusion of a stroke. To confirm the diagnosis when identifying the earliest signs of the disease, it is enough to carry out very simple tests:
- ❗ Does your face look unusual? — Ask the patient to smile.
- ❗ Does this sound strange? — Ask the patient to repeat the phrase.
- ❗ One hand falls down? —Ask the patient to raise both arms.
If a stroke is suspected, it is necessary to urgently refer the patient for neuroimaging and to a neurologist.
Asymmetry of one half of the face can be observed with damage to the facial nerve (neuropathy), which occurs suddenly and may be accompanied by other symptoms: the palpebral fissure on the affected side does not close, water and liquid food pour out of the mouth, lacrimation and impaired taste are observed.
It is very important to immediately refer the patient to a neurologist, because treatment started later than 3 days from the onset of the disease may be ineffective, which threatens not only facial asymmetry, but also ophthalmological problems (conjunctivitis, keratitis and even loss of vision). Slowly progressive damage to the facial nerve is observed with cancer of the brain (for example, with a tumor of the cerebellopontine angle).
Causes of attention deficit disorder
Today, no one can say for sure why a child develops ADHD symptoms. Among the factors that give impetus to the development of attention deficit disorder are:
- heredity. Researchers have noted that the presence of this disorder in parents several times increases the likelihood of its development in children. Attention deficit disorder is often genetic in nature and can therefore be inherited;
- drinking alcohol and smoking during pregnancy can lead to impaired brain function in the fetus, which leads to the appearance of ADHD symptoms in the child in the future;
- a difficult pregnancy, infectious diseases suffered by a woman during this time can also lead to the child developing attention deficit disorder. The risk of developing this mental disorder increases several times among children born prematurely;
- Predisposition to the development of the disorder is increased by brain injuries of varying severity suffered by a child at an early age, as well as diseases of an infectious nature.
In some cases, attention deficit disorder occurs as a symptom of another mental disorder, for example, delayed speech or psycho-speech development. Some life circumstances or pathological processes in the body can manifest themselves in the same way as the symptoms of ADHD. Among them are:
- A sudden change in lifestyle, moving, parental divorce or death of a loved one.
- Malfunction of the thyroid gland.
- Poisoning with heavy metals, in particular lead.
- Depression and sleep disorders.
Experts believe that it is impossible to completely eliminate the symptoms of ADHD. This disorder is considered an incurable pathology. But it is still possible to help a child. Properly organized therapy will allow the patient to learn better, gain the necessary social skills and adapt to society.
SPEECH DISORDERS
They can have different manifestations: aphasia, alalia, bradyllia, dysarthria, dysorthography, dysgraphia, dyslexia, dyslalia, etc. In adults, they almost always indicate various neurological diseases. Thus, a sudden speech disorder may be associated with a transient ischemic attack or be an early sign of a stroke, and a progressive one may be a manifestation of amyotrophic lateral sclerosis. Therefore, in the case of this serious neurological syndrome, it is imperative to refer the patient to a neurologist.
Forms and complications
The main clinical manifestations of post-coronavirus syndrome:
- respiratory disorders: persistence or increase in shortness of breath, respiratory failure, cough, ventilation disorders and interstitial changes (including fibrosis) in the lungs according to chest computed tomography (CT CT), development of pulmonary hypertension;
- thrombotic complications, including pulmonary embolism;
- heart rhythm disturbances, orthostatic hypotension;
- anxiety-depressive disorders, sleep disorders;
- exacerbation of chronic diseases, primarily of the respiratory and cardiovascular systems;
- nonspecific asthenic manifestations, vegetative dystonia.
PAIN AND NUMBITY IN THE FACE
If the facial pain is intense, manifests itself in attacks lasting from 3 to 30 seconds, occurs during conversation, or is provoked by touch, then the probable diagnosis is trigeminal neuralgia (trigeminal neuralgia).
This independent neurological problem is often associated with compression of the vessels of the trigeminal nerve root. In elderly patients, with hypersensitivity of the skin in the temporal region, chewing disorders and accelerated ESR, one can suspect temporal arteritis, which is often confused with migraine. It is necessary to perform a blood test to evaluate ESR and refer the patient to a neurologist to exclude this pathology.
It should be noted that a normal ESR does not exclude the diagnosis of giant cell arteritis. Pain and numbness in the face in combination with other neurological disorders (facial asymmetry, eye movement disorders, etc.) require urgent neuroimaging to exclude cancer.
Types of Neurological Diseases
Clinical classification of pathologies of the central and peripheral nervous system:
- Vascular diseases of the brain (transient and progressive cerebrovascular accidents, strokes).
- Epilepsy (partial and generalized seizures).
- Infectious diseases of the nervous system (meningitis, myelitis, encephalitis, epiduritis, poliomyelitis, multiple sclerosis).
- Diseases of the peripheral system (vertebrogenic pathologies, lesions of nerve roots, nerves, cranial nerves).
- Tumors of the central nervous system (gliomas, neoplasms of the spinal and cranial nerves, meninges, pituitary gland).
- Pathologies of the autonomic nervous system (migraine, neuroses, hereditary neuropathies, systemic and autoimmune diseases).
- Injuries of the central nervous system (craniocerebral, spinal cord).
- Headache (tension headaches, cluster headaches, migraine, pain associated with metabolic or vascular disorders, cranial neuralgia).
- Hereditary degenerative diseases (Huntington's chorea, Refsum's disease, Gaucher's disease, Marfan's disease, myasthenia gravis).
- Diseases of the nervous system of childhood and developmental defects (cerebral palsy, hydrocephalus).
- Impaired consciousness (stupor, coma).
INSTABILITY, STABLISHING (DYSBASIA)
Sudden onset and increasing instability and staggering is a dangerous signal that may indicate a TIA or stroke, which requires urgent referral of the patient to a neurologist.
Neurological symptoms also include a gradually increasing unsteady gait, indicating alcoholic polyneuropathy, B12-deficiency anemia and normal pressure hydrocephalus. Such patients also need consultation with an appropriate specialist. For complaints of instability, a postural response test after short jolts is recommended.
NUMBNESS
As a rule, a complaint of numbness of the limbs does not cause serious concern to the doctor, however, this symptom may be a manifestation of the following neurological diseases:
- ✅ epilepsy (with repeated episodes of short-term numbness lasting up to 2 minutes);
- ✅ tunnel syndrome (with constant numbness combined with pain in one place);
- ✅ polyneuropathy (with constant numbness in the legs and arms like “socks” and “gloves”), including Guillain-Barre polyneuropathy in case of increasing numbness in the legs (hours - days) combined with weakness.
Thus, if you complain of numbness, the patient must be referred to a neurologist.
DISORDERS IN HEAD OR NECK POSTURE
Poor posture of the head and neck, difficulty writing and involuntary movements not associated with injuries and/or musculoskeletal pathology are dystonia syndromes. This very interesting group of diseases associated with damage to the central nervous system is characterized by continuous involuntary muscle contractions, often causing “twisting” of the affected part of the body and the formation of pathological postures. More recently, patients with torticollis (a form of focal dystonia) were diagnosed with “osteochondrosis” and subsequently prescribed appropriate ineffective therapy. Currently, this pathology can be corrected, so patients with dystonia must be referred to a neurologist.
Treatment of astheno-neurotic syndrome in the clinic
Astheno-neurotic syndrome can be considered as a pathologically modified version of the adaptation of the nervous system in response to physical and mental stress, intoxication, vascular and hormonal disruptions or disorders. Recently, asthenic and neurotic disorders of the nervous system have become particularly widespread. Therefore, in the treatment of astheno-neurotic conditions, the need to use specific complex drug therapy is of particular importance. Due to the fact that the main leading link of astheno-neurotic syndrome are pathological processes associated with the functioning of higher nervous activity, the need to use complex neurometabolic therapy comes to the fore.
Treatment of astheno-neurotic syndrome requires the use of both medicinal and non-medicinal methods. Biological therapy involves the use of immunomodulators, vitamin therapy and correctors, as well as the use of other means depending on the symptoms and causes of the pathology. In mild cases, staying in sanatorium-resort institutions, where a set of specific procedures are carried out, may be effective.
Non-medicinal methods
Treatment of astheno-neurotic syndrome without the use of medications usually does not bring good, lasting results. However, in a set of measures to combat this pathology, the need for non-drug methods is obvious. The choice of these methods is made together with the attending physician on an individual basis. The range of such tools is quite wide.
Basic non-drug methods of treating astheno-neurotic syndrome
- Psychotherapy;
- Hypnotherapy;
- Selection of daily routine;
- A set of physical activities;
- Music therapy;
- Physiotherapy;
- Light therapy;
- Physiotherapy;
- Water procedures;
- Massage.
DIFFICULTIES WHEN WRITING
Difficulty writing—“writer’s cramp”—is another form of focal dystonia. “Writer’s cramp” occurs only during active writing, after writing a few words or lines. In this case, the fingers are constrained and take an unusual position, writing becomes impossible. The violation may be limited to only one hand. A similar pathology occurs when printing. Today, this complex central regulatory disorder is treatable. Difficulty writing is also common in Parkinson's disease.
Thus, patients are referred to a neurologist in whom hand position problems when writing and handwriting problems are not associated with musculoskeletal pathology.
TREMOR
Tremors are rhythmic, rapid contractions of the muscles of the trunk or limbs of an involuntary nature. Tremor occurs when autonomic support is disrupted, metabolic disorders and damage to the central nervous system. It is necessary to distinguish between essential (“autonomous”) tremor, which is more common in clinical practice, and tremor in Parkinson’s disease.
Essential tremor increases with movement, and tremor in Parkinson's disease, on the contrary, is stronger at rest and disappears (or significantly decreases) with the onset of activity. In addition, in Parkinson's disease, tremor may initially seem to be an isolated symptom and usually begins in the hands. Later, a head tremor develops. It is necessary to carry out differential diagnosis of these conditions, since they have different natures and, accordingly, different approaches to treatment. Tremor can occur in practically healthy people due to anxiety, emotional and physical stress. A patient who has persistent tremors in the arms and/or legs should be referred to a neurologist.
Thus, the main neurological syndromes and screening tests that have a high diagnostic value are structured and presented, which will help to competently route the patient to a specialized specialist, which will significantly reduce the time the patient spends in the corridors of the clinic and the time required for the doctor to make the correct diagnosis and prescribe adequate therapy .
This will also contribute to the fulfillment of A. M. Wein’s dream: “I would like the slogan of medicine to be improving the quality of life.”
Astheno-neurotic syndrome: we recommend
It is recommended to eat foods rich in vitamin B and tryptophan (meat, bananas, beans, cheese and cottage cheese, dairy products, etc.). The amino acid tryptophan is responsible for the normal functioning of the nervous system - sleep, relaxation and emotional state, and is a source of the “happiness hormone” - serotonin.
Qualified specialists at the Transfiguration Clinic will help you create an effective therapeutic program, taking into account both the true cause of the disease and individual factors.