The pontocerebellar angle is the depression between the pons, medulla oblongata, and cerebellum. This area is often affected by neoplasms that compress the nerves, blood vessels and cerebrospinal fluid pathways passing there. The urgency of the issue of removing tumors of the cerebellopontine angle is due to the impossibility of treating them with modern radiosurgical methods, including a gamma knife and a linear accelerator. Thus, the method in this case is surgical treatment, which in turn requires adequate anesthesia and technical equipment.
I, Gavrilov Anton Grigorievich, neurosurgeon at the N. N. Burdenko Research Institute of Neurosurgery, have 20 years of practical experience, including the removal of tumors of the cerebellopontine angle. My clinical base (the aforementioned research institute) allows for complex interventions: high-tech equipment in operating rooms in combination with a well-coordinated team of anesthesiologists and resuscitators is an essential condition for achieving an optimal result.
Types of tumors of the cerebellopontine angle
Approximately every tenth brain tumor develops in the cerebellopontine angle. At the same time, the most common tumor localized in this area is neuroma of the vestibulocochlear nerve—it accounts for 85–95%. Meningiomas and cholesteatomas of the cerebellopontine angle are much less common.
In most cases, neuroma of the vestibulocochlear nerve is benign. Most often it develops in people of working age, usually women. Removal of tumors of the cerebellopontine ganglion can be either unilateral or bilateral.
Magnetic resonance imaging (MRI) in St. Petersburg
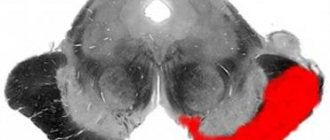
MRI of the brain. T1-weighted axial MRI (fragment). The cerebellopontine angles are normal. Color processing of the image.
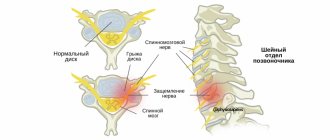
The pontocerebellar angle (MCA) is the junction of the pons, medulla oblongata and cerebellum. The main reason for research in this area is sensorineural hearing loss. ENT methods allow you to narrow the search by determining that hearing loss is associated with nerve damage retrocochlearly (in the MMU, not in the ear), or in the structures of the ear. In the latter case it is used more often. MRI St. Petersburg allows you to choose the location of the MRI; we recommend that you be examined with us, where the possibilities for targeted research are greater than in many other MRI centers. When performing MRI in St. Petersburg in our centers for retrocochlear hearing loss, the method of choice is MRI of the brain, since the 8th cranial nerve (vestibular-cochlear) is affected.
Typical tumors in this area are neuromas (schwannomas) and meningiomas. With neuromas, there may be a tumor fragment in the internal auditory canal, which is visible, especially with contrast-enhanced MRI of the brain.
MRI of the brain. T1-dependent MRI with contrast. Schwannoma with compression of the 4th ventricle.
MRI of the brain. Schwannoma with a component inside the tubule.
MRI of the brain. T1-weighted coronal MRI with contrast. Completely intracanalicular neuroma.
Tumors of the endolymphatic sac, cholesteatoma, paraganglioma, lipoma and aneurysm of the internal carotid artery are also found in the area of the apex of the temporal bone.
Tumors of the endolymphatic sac are benign, slow-growing, bilateral and associated with Hippel-Lindau disease, which belongs to the group of phakomatoses. A CT scan shows bone erosion of the apex of the pyramid, and an MRI of the brain with contrast enhances the formation well.
MRI. T1-dependent with contrast. Tumor of the endolymphatic sac.
Cholesteatomas (epidermoid cysts) are often found in the area of the petrous apex. Their display on MRI depends on the amount of cholesterol present.
MRI. T2-dependent tomogram. Cholesteatoma.
Lipomas are typically bright on T1-weighted MRI and T2-weighted MRI of the brain.
MRI of the brain. T1-dependent MRI. Lipoma.
Rarely occurring chondrosarcomas destroy the apex of the pyramid, which is visible on MRI and CT scans of the brain.
MRI of the brain. T2-dependent MRI. Chondrosarcoma.
Leave feedback.
MRI in St. Petersburg USA
Clinical picture
Timely removal of tumors of the cerebellopontine angle is complicated by the slow development of the disease without severe clinical manifestations. The patient may experience noise in one ear for several months or even years (so-called cochleovestibular syndrome). Then comes a period when the signs of the disease become more pronounced (deafness, facial nerve paresis). In most cases, diagnosis and then removal of tumors of the cerebellopontine angle are carried out precisely at this stage.
Other consistently occurring symptoms of the disease include:
- headache;
- loss of corneal and conjunctival reflexes;
- cerebellar phenomena - unilateral hemiataxia and general cerebellar ataxia, adiadochokinesia, unsteady gait, decreased muscle tone, dizziness;
- paralysis of limbs.
Syndromes of damage to the base of the skull with metastases
Introduction
Syndromes of lesions of the skull base, occurring in various pathologies (primary and metastatic tumors of the skull base, infectious lesions of vascular diseases) were described at the turn of the 19th – 20th centuries [1]. Due to the close proximity of the cranial nerves and vessels of the skull base, damage to the latter is usually clinically manifested by dysfunction of several structures.
The base of the skull is traditionally divided into the anterior, middle and posterior cranial fossae; their tumor lesions cause specific symptoms due to the involvement of a certain anatomical zone in the pathological process. In 1981, describing the clinical and neurological picture of metastatic lesions of the skull base, H. Greenberg et al. identified five characteristic neurological syndromes, most often found in metastases: 1) orbital syndrome; 2) parasellar syndrome; 3) middle cranial fossa syndrome (Gasserian node syndrome); 4) jugular foramen syndrome; 5) occipital condyle syndrome [4].
The table shows known neurological syndromes of damage to the base of the skull in comparison with the classification of H. Greenberg et al. (Table 1) [1, 4].
Table 1. Neurological syndromes with lesions of the base of the skull.
| Name of neurological syndrome | Cranial nerve damage | Localization of pathology | The name of neurological syndromes according to the classification of H. Greenberg et al. |
| Reder syndrome | 5 + sympathetic fibers (Horner's sign) | SCHYA | No |
| Superior orbital fissure | 3, 4, 6 and 1 branch of 5 nerves | PCHYA, SCHYA | Orbital, parasellar |
| Rollet orbital apex syndrome | 3, 4, 6 and 2 nerves | PCHYA, orbit | Orbital |
| Bonnet cavernous sinus syndrome | 3, 4, 6, 1st branch of 5th nerve, exophthalmos, chemosis | SCHYA | Parasellar |
| Foix cavernous sinus lateral wall syndrome | 3, 4, 6, 1 branch of the 5th nerve, | SCHYA | Parasellar |
| Jefferson torn hole syndrome | 3, 4, 6 and 1 branch of the 5th nerve | SCHYA | No |
| Vernet jugular foramen syndrome | 9, 10, 11 | ZCHYA | Jugular foramen syndrome |
| Collet-Sicard syndrome | 9, 10, 11, 12 | ZCHYA | Combination of STS and occipital condyle syndrome |
| Villaret syndrome | 9, 10, 11, 12 and Horner's syndrome | ZCHYA | No |
| Jacod syndrome | 3, 4, 6, 1 and 2, sometimes 3 branches of the trigeminal nerve, 2 nerve, hearing loss (due to obstruction of the auditory tube) | PCHYA, SCHYA | SCN syndrome |
| Gradenigo syndrome | 5, 6 nerves, rarely paresis of 3, 4, 7 nerves | SCHYA | SCN syndrome |
| Foster–Kennedy syndrome | 1, 2 nerves on one side, congestive nipple on the other | PCHYA | No |
| Pontocerebellar angle syndrome | 7, 8 and intermediate nerve, cerebellar syndromes on the affected side and pyramidal signs on the opposite side | ZCHYA | Pyramidal temporal bone syndrome |
| Hunt's geniculate ganglion syndrome | Pain syndrome and characteristic skin herpetic manifestations, possible involvement of the 7th and 8th nerves, sometimes the 5th nerve and Horner's syndrome | SCHYA | No |
| Garsin syndrome | Unilateral multiple cranial nerve syndrome | SCHYA, ZCHYA | Combination of several syndromes (orbital, parasellar, Gasserian node, Collet - Sicard) |
| Idiopathic cranial polyneuropathy | 3, 4, 6 nerves, then 5 and 7 nerves and 2 lower cranial nerves (9, 10, 11, 12) | SCHYA, ZCHYA | No |
Subsequently, in all works devoted to metastatic tumors at the base of the skull, the authors, as a rule, take as a basis the classification of H. Greenberg et al. , but at the same time they allow some changes in the form of adding, deleting or combining syndromes.
Material and methods
From 2001 to 2013 at the Research Institute of Neurosurgery named after. acad. N. N. Burdenko operated on 163 patients with metastatic tumors of the skull base. The ratio of men: women was 1: 1, 3. The median age of patients was 51 years (minimum 2 years 7 months, maximum 87 years). The largest group consisted of patients with metastases of breast cancer - 36 (22%) patients, followed by patients with metastases of tumors of the genitourinary system - 26 (16%) (of which metastases of renal cell cancer - 18, prostate cancer - 4), melanoma metastases – 12 (7.3%), gastrointestinal cancer metastases – 10 (6.1%). There were isolated patients with metastases of differentiated thyroid cancer, Ewing's sarcoma, medulloblastoma, germinoma, adenocarcinoma and poorly differentiated cancer from unidentified primary foci.
By location, metastases were distributed in the following proportions: anterior cranial fossa (ACF) - in 39 (24%) cases, middle cranial fossa (MCF) - 78 (47.9%) (of which there were 27 CSF), posterior cranial fossa (MCF) ) – 30 (18.4%). Combinations of lesions of adjacent cranial fossae were observed, including the PFC and SCN - 10 (6.1%), SCN and PFC - 5 (3%). Damage to 3 fossae was observed in 1 (0.6%) case.
The clinical picture was represented by local, cerebral symptoms and syndromes of cranial nerve damage. The incidence of various syndromes in metastatic tumors of the skull base is presented in Table 3.
Table 3. Frequency of occurrence of the main clinical manifestations of skull base metastases.
| Predominant clinical manifestations | Number of patients | Percentage |
| Cranial nerve syndrome | 104 | 63, 8% |
| General cerebral symptoms | 41 | 25% |
| Local pain syndrome | 34 | 21% |
| Local deformation | 48 | 29% |
| Focal hemispheric symptoms | 27 | 16, 6% |
The most common syndromes with metastatic tumors of the skull base are syndromes of damage to the cranial nerves in combination with symptoms of involvement in the pathological process of other adjacent structures of the skull base - the contents of the orbit, pituitary gland, cavernous sinus, paranasal sinuses, infratemporal and pterygopalatine fossa. Such combinations, as a rule, appear as described by H. Greenberg et al. syndromes.
In the series of 163 patients with metastatic tumors of the skull base that we analyzed, cranial nerve lesion syndromes were observed in 104 (63.8%) cases. In the remaining patients, the disease manifested itself with general cerebral symptoms, symptoms of focal brain damage and local changes.
The identified focal neurological syndromes were divided into 7 groups according to that proposed by H. Greenberg et al. classifications. Considering the number of observations and the difference in clinical manifestations, we decided to consider sellar and parasellar syndromes separately. It should be noted that in our series there were no cases of numb chin syndrome, which is described by F. Laigle - Donadey et al.
It is safe to say that none of the syndromes of cranial nerve damage manifests itself in isolation, in a “pure” form. As a rule, there are combinations of lesion syndromes, for example, orbital and parasellar, sellar and parasellar, Gasserian ganglion and parasellar syndrome, occipital condyle and jugular foramen syndrome. The combination of the last two syndromes in neurology is known as Collat-Sicard syndrome.
The work examines patients with histologically verified metastases to the base of the skull. All patients underwent neurological, neuro-ophthalmological and otoneurological examinations. The absolute numbers and percentages of the different syndromes in our series are presented in Table 3.
Table 3. Frequency of occurrence of skull base lesion syndromes with metastases.
| Cranial nerve syndromes | Number of patients | |
| abs | % | |
| 41 | 25% |
| 19 | 11, 7% |
| 11 | 6, 7% |
| 9 | 5, 5% |
| 9 | 5, 5% |
| 10 | 6, 2% |
| 5 | 3, 1% |
results
In patients with identified symptoms of damage to the base of the skull in our series, the most common syndrome was orbital syndrome ( OC ); it occurred in a quarter of observations (41 patients). OS syndrome was observed in metastatic tumors localized directly in the orbit in 3 (7.4%) cases, with metastasis growing into the orbit from the structures of the anterior cranial fossa (ACF) - in 20 (48.7%) cases, from the middle cranial fossa ( SCHY) in 18 (43.9%) cases.
Orbital or cranio-orbital metastases occurred in breast cancer in 7 cases, renal cell carcinoma in 6 cases, melanoma in 3 cases, and in tumors from an undetected primary site in 7 cases. There were single metastases of prostate cancer, leiomyosarcoma, plasmacytoma, histocytoma, and retinoblastoma.
Spread into the orbit from the anterior cranial fossa occurred when the tumor was localized in the area of the orbital roof, in the ethmoid bone, through destruction of the walls of the orbit and invasion into it. As a rule, with such a localization, the tumor affected the dura mater of the anterior cranial fossa, the basal parts of the frontal lobe, which led to a combination of orbital syndrome with symptoms of damage to the basal parts of the frontal lobes, signs of intracranial hypertension.
In 3 patients, metastases were initially localized in the lateral wall of the orbit and, destroying it, penetrated into the orbit. In these patients, the tumor did not invade the dura mater and brain, did not cause general cerebral and focal symptoms, and was clinically manifested only by exophthalmos and mild oculomotor disturbances.
A common cause of orbital syndrome was metastases in the middle cranial fossa. There were 18 of them in our series. From the middle cranial fossa, tumors spread into the orbit in several ways: through the superior orbital fissure, through the optic nerve canal, by destroying the lesser or greater wings of the sphenoid bone. Since the initial location of tumors spreading into the orbit is the middle cranial fossa, orbital syndrome in these patients was combined with a clinical picture of damage to the temporal lobe, branches of the trigeminal nerve, and oculomotor nerves.
In 5 cases, metastases initially localized in the chiasmal-sellar region spread into the orbit through the superior orbital fissure. In such cases, orbital syndrome manifests itself as severe oculomotor disturbances and is combined with sellar-parasellar syndrome in the form of diabetes insipidus, hypopituitarism, oculomotor and visual disturbances.
Of the known neurological syndromes of damage to the base of the skull, the orbital syndrome described by H. Greenberg et al. includes syndromes of the apex of the orbit and the superior orbital fissure.
Orbital syndrome consists of several symptoms that occur with different frequencies. This is exophthalmos of varying severity, arising due to one or more reasons: the presence of a tumor mass in the orbit, swelling of the orbital tissue, when the tumor spreads inside Tenon's capsule and due to venous stagnation in the orbit when the tumor spreads into the orbit from the middle cranial fossa through the superior orbital fissure. In our series, exophthalmos was a constant symptom of orbital syndrome and occurred in all cases.
The second characteristic symptom of orbital syndrome is oculomotor disturbances . They occur more often and are more severe when the tumor spreads into the orbit through the superior orbital fissure. Ophthalmoplegia was observed in 4 cases, ophthalmoparesis - in 33 (80.5%) cases. It should be noted that diplopia can occur as a result of damage to the nerves involved in the innervation of the extraocular muscles, and due to mechanical compression of the eyeball by a tumor.
Decreased vision is often observed as part of orbital syndrome. The cause of visual impairment is damage to the optic nerve in the orbit, the optic nerve canal, in the orbit and in the chiasmal-sellar region. Decreased vision was noted in 22 (53.4%) cases, while unilateral vision loss was observed in 17 (41.1%) cases. In 5 (12.2%) cases, visual disturbances were caused by compression of the optic nerves and chiasma in the chiasmatic sellar region and were combined with a narrowing of the visual fields. Amaurosis was observed in 3 (7.3%) patients.
In some cases, a dense formation is palpated in the orbit. In our observations, through the soft tissue of the tumor, the orbits were accessible for palpation in 15 cases.
Pain in orbital syndrome can be either local or a manifestation of damage to the first branch of the trigeminal nerve. If local pain is characterized by severity and dull pain in the orbit, then damage to the supraorbital nerve is characterized by impaired sensitivity, paraesthesia and pain in the frontal region. A decrease in sensitivity in the zone of innervation of the 1st branch of the trigeminal nerve was observed in 19 (46.3%) cases. 14 (34%) patients had pain and paresthesia in the frontal region due to decreased sensitivity.
Sellar syndrome. Metastases to the sellar region are often identified with metastases to the pituitary gland. We observed 19 patients with sellar syndrome. In 5 cases, metastases of breast cancer were noted, in 5 cases - metastases of cancer from the genitourinary tract (in 3 cases of renal cell cancer, in 1 case of cervical cancer and in 1 case of prostate cancer). There were isolated observations of metastasis of melanoma, germinoma, adenocarcinoma of unknown origin, nasopharyngeal cancer, glioblastoma, and medulloblastoma.
Sellar syndrome can be identified with the so-called “chiasmal-sellar” syndrome, manifested by endocrine and visual disturbances.
Diabetes insipidus is a common manifestation of metastases to the pituitary gland; according to some authors, it occurs in 70% of cases. In our series, diabetes insipidus was observed in 7 (37%) cases.
Manifestations of dysfunction of the adenohypophysis are rarely observed, since it occurs only when it is completely destroyed. In patients with sellar syndrome, dysfunction of the adenohypophysis in the form of panhypopituitarism or impaired secretion of certain hormones was observed only in 4 (21%) cases
Visual disturbances in the form of chiasmal syndrome are a characteristic component of metastatic tumors of the sellar region. They are manifested by decreased vision (in some patients to the point of blindness) and/or narrowing of visual fields due to suprasellar tumor growth and compression of the chiasm. Decreased vision is a common syndrome when metastases are localized in CSR; in our series of 16 (84%) cases of visual impairment, 5 cases had unilateral lesions, and 11 cases had bilateral lesions. Decreased visual acuity was observed in 9 patients, narrowing of visual fields in 13 cases.
The spread of metastasis to the pituitary gland laterally into the cavernous sinus causes neuropathy of the oculomotor nerves, therefore sellar and parasellar syndromes often appear together, which leads to the occurrence of neuroendocrine disorders in combination with visual and oculomotor disorders. This combination was observed in 4 patients.
Parasellar syndrome is caused by metastases located in the cavernous sinus. We observed this syndrome in 11 cases (6.7%). The tumors were represented by metastases of breast cancer (3), renal cell carcinoma (2), Ewing's sarcoma (2), poorly differentiated nasopharyngeal cancer (2), metastases of adenocarcinoma from an unknown source (2).
Parasellar syndrome is a combination of two known syndromes - Bonnet cavernous sinus syndrome and Foix lateral wall cavernous sinus syndrome.
Often the first sign of parasellar metastasis is unilateral pain in the frontal region, which is sharp, shooting in nature. In most cases (8), pain in the frontal region is combined with numbness. In 2 patients with large tumors growing into the cranial cavity and causing compression of the brain, diffuse headache was also noted.
Characteristic of parasellar syndrome are oculomotor disorders, which in our series resulted from damage to the oculomotor nerve in 5 cases, the abducens nerve in 2 cases, and all nerves involved in the innervation of the oculomotor muscles in 4 patients.
In 2 cases, oculomotor disorders in the form of ophthalmoplegia were accompanied by exophthalmos, due to tumor growth into the orbital cavity from the cavernous sinus through the superior orbital fissure. Oculomotor disorders of varying degrees were detected in all patients. Ophthalmoplegia was observed in 6 cases, ophthalmoparesis was observed in 5 cases.
Diplopia was observed in all patients with parasellar syndrome.
In 3 patients, periorbital venous congestion was noted, which arose due to the invasion of the cavernous sinus.
Visual disturbances in parasellar syndrome occurred when it was combined with sellar or orbital syndromes. During a neuro-ophthalmological examination, unilateral papilledema was detected in the fundus of 7 patients.
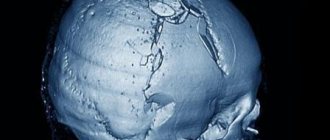
Syndrome of the pyramid of the temporal bone. In our observations, there were 12 patients with pyramidal temporal bone syndrome . The histostructure of metastases is varied, the maximum number of tumors of the same type is 2 (Ewing's sarcoma). There were single metastases of lung cancer, leiomyosarcoma, melanoma, adenoid cystic cancer, fibrous histiocytoma, glioblastoma, and synovial sarcoma. In two cases, cancer metastases were from an undetected primary site.
Clinically, this syndrome is similar to the cerebellopontine angle syndrome, although the mechanism of damage to the facial and vestibulocochlear nerves in these syndromes is different. With pyramidal temporal bone syndrome, the nerves are affected inside the bone structures, and with cerebellar-pontine angle syndrome, the effect on the 7th and 8th nerves occurs intracranially in the cerebellar-pontine angle without involving bone structures.
The clinical picture consists of symptoms of damage to the facial and auditory nerves. Dysfunction of the facial nerve is manifested by paresis or paralysis of facial muscles. In 10 of our patients, dysfunction of the facial nerve was noted from 2 to 5 points on the Hause-Brakmann scale.
In case of pyramidal temporal bone syndrome, hearing loss is often neurosensory in nature due to damage to the cochlear nerve (8 patients). Sensorineural hearing loss is always combined with damage to the facial nerve. But conductive hearing loss is also possible due to damage to the middle ear with a intact cochlear nerve (4 patients). In this case, hearing impairment may not be combined with paresis of the facial nerve (2 observations).
In 8 cases, patients complained of dizziness, possibly due to damage to the vestibular nerve or labyrinth.
Otalgia occurred due to irritation of the dura mater of the temporal bone pyramid or due to compression of the auditory tube.
Tinnitus on the affected side (in 7 patients) is a characteristic complaint for such patients; it occurred and was caused by conductive or sensorineural hearing loss.
Periauricular edema was observed when the tumor destroyed the lateral parts of the pyramid of the temporal bone and spread to the soft tissues of the temporal bone (3 patients).
Middle cranial fossa syndrome (Gasserian node syndrome) is observed when a metastatic tumor is localized in the middle cranial fossa, in Meckel's cavity. Isolated syndrome was observed in 5 cases. In 3 cases this was caused by metastasis of breast cancer, in 1 case by renal cell carcinoma and in 1 case by metastasis of fibrosarcoma.
Of the classic skull base lesion syndromes, this syndrome is similar to Jacob and Gradenigo syndromes.
The leading symptoms of this syndrome are sensory disturbances in the zone of innervation of the 2nd and 3rd branches of the trigeminal nerve and pain, often of a neuropathic nature. Often Gasserian ganglion syndrome is combined with parasellar syndrome and with the syndrome of damage to the pyramid of the temporal bone.
3 patients had numbness and paresthesia in the face, accompanied by constant or paroxysmal pain. In all cases, neurological symptoms were localized in the area of innervation of the 2nd and 3rd branches of the trigeminal nerve. In 2 patients, there was numbness in the cheek, chin, and temporal region, accompanied by dull pain in the cheek or lower jaw.
Weakness of the masticatory muscles was observed in 2 patients.
Rarely, sensory disturbances occurred in the area of innervation of the 1st branch of the trigeminal nerve. Often sensory disorders along the first branch were combined with disorders in the innervation zone of the 2nd and 3rd branches of the trigeminal nerve.
In 3 cases, due to intracranial spread of the tumor, severe cerebral symptoms such as headache and nausea were noted. In 1 case there was an isolated lesion of the abducens nerve due to tumor spread into the Dorello canal.
In 3 cases, Gasserian ganglion syndrome was combined with parasellar syndrome, when the patient had decreased sensitivity in the frontal region and oculomotor disorders.
In 2 cases, middle cranial fossa syndrome was combined with a syndrome involving the pyramid of the temporal bone due to invasive tumor growth into the latter. With this combination of syndromes, trigeminal nerve dysfunction was combined with sensorineural hearing loss and facial nerve paresis.
Jugular foramen syndrome (JHS) was observed in 9 cases. In 4 cases, STS was caused by metastases of breast cancer, in 2 cases of lung cancer, in one case by metastases of prostate cancer, renal cell cancer, and in one patient by metastases of cancer from an undetected primary site.
Vernet's jugular foramen syndrome (JFS) is known and occurs not only with metastatic tumors, but with glomus tumors, glossopharyngeal nerve neuroma, phlegmon and lymphadenopathy in this area.
The jugular foramen can be the area of primary tumor growth, and metastases can also spread into it from the pyramid of the temporal bone, the condyle of the occipital bone. Depending on the initial location of the tumor, isolated jugular foramen syndrome or its combination with occipital condyle or temporal bone syndromes are possible.
Isolated jugular foramen syndrome is characterized by dysfunction of the IX, X, XI nerves, which is manifested by dysphonia, dysphagia, and hoarseness of voice.
An otoneurological examination reveals unilateral weakness of the soft palate, deviation of the uvula in the direction opposite to the lesion,
unilateral vocal cord paresis. Damage to the XI nerve led to noticeable weakness of the sternocleidomastoid and upper trapezius muscles in 2 cases. The literature describes glossopharyngeal pain in jugular foramen syndrome, but this symptom was not encountered in our observations.
In 2 patients, papilledema was detected due to compression of the jugular vein or transverse sinus.
When STS is combined with pyramidal syndrome, patients complain of hearing loss and facial asymmetry. Such a widespread lesion in our series occurred in 2 cases with metastasis of breast cancer and adenocarcinoma from an undetected primary site.
Occipital condyle syndrome (OCS) is the most stereotypical and easily diagnosed syndrome with metastases to the base of the skull. Its first description belongs to H. Greenberg.
We observed 9 patients with occipital condyle syndrome, in 7 of whom it manifested itself in isolation, in 2 cases it was combined with jugular foramen syndrome. The cause of SPM was metastases of uterine leiomyosarcoma (1), metastasis of thyroid cancer (2), poorly differentiated cancer (1) and adenocarcinoma (1) from an undetermined primary site, renal cell carcinoma (1), lung cancer (1), breast cancer (1) .
Occipital condyle syndrome has 2 components. First, unilateral pain appears in the cervical-occipital region, which intensifies with head movements. Over time, pain in the neck progressively increases and subsequently a peripheral lesion of the 12th nerve occurs, which is manifested by deviation of the tongue towards the lesion, hemiatrophy of the tongue. Due to impaired innervation of the tongue, 3 patients had slurred speech.
In 2 cases, occipital condyle syndrome was combined with jugular foramen syndrome. This combination is called Collet-Sicard syndrome, characterized by unilateral damage to the IX, X, XI, XII nerves. The symptoms in these patients consisted of a characteristic cervical-occipital pain syndrome in combination with dysphonia, dysphagia, and peripheral damage to the hypoglossal nerve.
The discussion of the results
In patients with metastatic tumors of the skull base, the disease, as a rule, has a variety of clinical manifestations, which depend on the location and nature of the primary lesion, the presence of distant metastases, and the stage of the disease. Damage to the structures of the base of the skull during metastases, as a rule, manifests itself as dysfunction of the cranial nerves in combination with damage to vascular structures, the pituitary gland, and the orbit. Some of these syndromes, despite the fact that they can manifest themselves in various pathologies and are not specific, are quite characteristic of metastatic lesions of the skull base and, in combination with an oncological history and other signs of cancer, contribute to early diagnosis.
The study of the problem of metastatic tumors of the skull base begins in 1979, when B. Vikram and F. Chu published the results of radiation treatment of 46 patients with metastases at the skull base, observed at Memorial Sloan-Kettering Cancer Center from 1971 to 1976 [9] . In 1981, H. Greenberg et al. described and systematized these tumors in more detail by location and neurological picture, identifying five neurological syndromes most often observed in metastatic lesions of the skull base. Classification by H. Greenberg et al. is still used by all authors who describe more or less large series of metastases to the base of the skull [4]. Some authors take this classification as a basis when describing the neurological picture in primary tumors of the skull base [2].
Over time, in the classification of H. Greenberg et al. changes were made. So, in 2004 F. Hanbali, later in 2011 B. Roukoz described middle cranial fossa syndrome, in 2005 F. Laigle – Donadey et al. described numb chin syndrome [4, 5, 6, 8]. In addition to H. Greenberg, who described parasellar syndrome, all subsequent authors also added sellar syndrome to this syndrome (Table 4).
Table 4. Neurological syndromes in metastatic tumors of the skull base
| Syndromes | H. Greenberg [4] (n=43) | F. Laigle – Donadey [6] (n=279) | K. Mitsuya [7] (n=97) | Our series |
| Orbital | 3 (7%) | 35 (12, 5%) | 4 (20%) | 39, 4% |
| Parasellar and sellar | 7 (16%) | 81 (29%) | 7 (35%) | 9, 6% +18.2% (s) |
| Gasserian node (middle cranial fossa) | 13 (30%) | 17 (6%) | 4 (20%) | 4, 8% |
| Jugular foramen | 9 (21%) | 10 (3, 5%) | 3 (15%) | 8, 6% |
| Occipital condyle | 9 (21%) | 45 (16%) | 2 (10%) | 8, 6% |
| Numb chin syndrome | 0 | 39 (14%) | 0 | 0 |
| Temporal bone syndrome (pyramid of the temporal bone) | 0 | 0 | 0 | 9, 6% |
| OTHER | 0 | 33% | 0 | 0 |
In our series, we did not observe patients with numb chin syndrome. We consider sellar and parasellar syndromes separately, due to the fairly large number of patients in each of these groups and the prevalence of symptoms characteristic of one syndrome.
Literary data on the histogenesis of tumors in various syndromes are extremely scarce. Only in the work of F. Laigle - Donadey et al. the percentage of metastases causing orbital syndrome is indicated: prostate cancer (56%), lymphoma (23%), breast carcinoma (15%) [6].
We tried to find a pattern in the distribution of metastases in different areas of the skull base and it turned out that it reflects the general distribution of metastases rather than the tropism of any metastasis to certain areas of the skull base. Most syndromes are caused by metastases of breast cancer - orbital - 7, sellar - 5, jugular foramen - 4, parasellar - 4, Gasserian node syndrome - 3. Metastases of renal cell cancer are relatively common in orbital syndrome - 6, sellar syndrome - 5. In the literature, we found only one explanation for a certain pattern of distribution of metastases at the base of the skull. The authors believe that metastases from the breast and genitourinary tract are often localized in the sellar region, and they associate this fact with a favorable hormonal background for the development of metastases in this area [6].
From Table 4 it follows that in different series of skull base metastases, the syndromes occur with different frequencies.
In our series, orbital syndrome ranks first in frequency (25%), while in the series of H. Greenberg this syndrome is the rarest (7%), in the series of other authors it ranks 2 (K. Mitsuya -20%) and 4 places (F. Laigle-Donadey – 12.5%) [4, 6, 7].
For most authors, the most common is sellar-parasellar syndrome (16-35%), which is probably due to the fact that, due to the similarity of clinical symptoms, they combined these 2 syndromes into one. If we had done the same, then in our series sellar-parasellar syndrome with a number of 30 (28.7%) patients would have taken 2nd place after orbital syndrome.
The third place in frequency in our series is occupied by pyramidal temporal syndrome. This syndrome is described only by authors from MD Andersen Cancer Center and is not mentioned by other authors [8].
The largest variation is observed in the incidence of Gasserian ganglion syndrome – from 6% (F. Laigle – Donadey) to 30% (H. Greenberg) [4, 6]. In our series, this syndrome is the smallest - 4.8%. We found the following explanation for this: Gasserian ganglion syndrome and parasellar syndrome are very similar in damage to the oculomotor nerves and branches of the trigeminal nerve. Diagnosis at the time of H. Greenberg (1981) was based on data from craniography and clinical analysis [4]. Modern neuroimaging methods make it possible to more accurately determine the location of the tumor, due to which the areas of the Gasserian ganglion and parasellar tumors with similar clinical manifestations of the tumor are differentiated.
The incidence of other syndromes also varies widely: occipital condyle syndrome - 10-21%, and jugular foramen syndrome - 3.5-21%. Numb chin syndrome in 14% of cases is described in the work of F. Laigle – Donadey et al. , while in other authors, including in our series, this syndrome does not occur [6].
The percentage of various syndromes in our series differs significantly from the data of H. Greenberg et al. Considering that the number of patients we observed was 104, and in H. Greenberg’s series – 43, perhaps our data more reliably reflects the distribution of clinical syndromes [4]. This is confirmed by the closeness of our results to those in larger series by F. Laigle-Donady et al. , and K. Mitsuya et al [6, 7].
We did not find significant differences in the description of clinical syndromes in our series and in the literature data.
It can be said that the sensitivity and specificity of the described syndromes for metastases at the base of the skull are different. The most specific of these syndromes is occipital condyle syndrome, which occurs only with metastases of the skull base. D. Capobianco et al. this syndrome is called “stereotypic” for metastases at the base of the skull [3]. All other syndromes are observed with other, both benign and malignant tumors of the skull base. And only their comparison with signs characteristic of the oncological process, such as an oncological history, rapid tumor growth, rapid progression of symptoms, and other distant metastases, allows us to assume the metastatic genesis of the lesion at the base of the skull.
Conclusion
Metastatic tumors of the skull base are neurologically manifested mainly by cranial nerve lesion syndromes. Neurological symptoms are determined by the topography of the metastasis. Metastases in the orbital area are clinically manifested by orbital syndrome, and when localized in the middle cranial fossa - sellar, parasellar syndromes, syndromes of damage to the Gasserian ganglion and the pyramid of the temporal bone. When a tumor of the middle cranial fossa grows into the orbit, a combination with orbital syndrome occurs. Metastases of the base of the posterior cranial fossa are manifested by the syndrome of the occipital condyle and the jugular foramen, in some cases a combination of the latter in the form of Collet-Sicard syndrome.
The syndromes described above are characteristic of lesions of the base of the skull by metastatic tumors. If a patient with a history of cancer experiences one of the syndromes described above, this gives reason to suspect a possible metastatic lesion of the base of the skull. Early diagnosis of tumors of the skull base is the key to timely and successful treatment of the disease.
Bibliography
- Golubev V. L., Vein A. M. Neurological syndromes. Moscow 2002. 523-525.
- Mudunov A. M. Tumors of the skull base. Clinic, diagnosis, treatment. Abstract diss……. doctors med. Sci. Moscow, 2010. 41
- Capobianco DJ, Brazis PW, Rubino FA. et al. Occipital condyle syndrome.
//Headache. 2002. N. 42. P. 142-146.
- Greenberg HS, Deck F, Vickram B, Chu FCH. et al. Metastasis to the base of the skull: clinical findings in 43 patients. // Neurology. 1981. N. 31 P. 530-537.
- Hanbali F., DeMonte F. Metastatic tumors of the skull base. Intracranial metastases. // Current management strategies. Blackwell Publishing 2004. 415-430.
- Laigle-Donadey F, Taillibert S, Martin-Duverneuil N, Hildebrand J, Delattre JY. Skull-base metastases. // J Neurooncol. 2005. N75. P. 63–69.
- Mitsuya K, Nakasu Y, Horiguchi S, Harada H. et al. Metastatic skull tumors: MRI features and a new conventional classification. // J. Neurooncol. 2011 V. 104. N1. P. 239-245.
- Roukoz B., DeMonte F. Management of skull base metastases. // Neurosurg Clin N Am. 22. 2011. 61–66.
- Vikram B, Chu FC: Radiation therapy for metastases to the base of the skull. Radiology 130:465–468, 1979
Features of surgery to remove a tumor of the cerebellopontine angle
Removal of the tumor of the cerebellopontine angle is carried out surgically. Before surgery, patients of this profile undergo general clinical and neurootological examination, CT and MRI. According to indications, myo- and angiography and neuropsychological testing are prescribed.
Removal of a tumor of the cerebellopontine angle is performed using modern methods of endoscopic microsurgery under conditions of constant neurophysiological monitoring (including stimulation and EMG of the facial nerve). After neuroimaging, the doctor develops a surgical plan, determines its volume and the point of best access. The intervention is carried out using high-speed drills and pneumatic drills, which ensure minimal invasiveness and reduce the extent of damage to nearby tissues.
Removal of a tumor of the cerebellopontine angle is carried out under endotracheal anesthesia in a closed circuit using Propofol and inhalational anesthetics (Sevoflurane, Isoflurane). Necessary conditions for the operation, which is performed in a sitting position, are also Doppler ultrasound of the heart and a special surgical table with supports for the surgeon’s hands. During the removal of a tumor of the cerebellopontine angle, it is possible to perform a rapid analysis of the removed fragment of the tumor with subsequent correction of the course of the operation.
The final result of surgical intervention is determined by the characteristics of tumor growth, the degree of damage to the base of the skull, and its fusion with neurovascular structures. In most cases, I, together with a team of assistants at the N. N. Burdenko Research Institute of Neurosurgery, manage to solve all the problems facing us.
Surgical treatment
Treatment of a tumor of the cerebellopontine angle is predominantly surgical. Surgery is performed after a complete neurological examination. Surgical treatment of the cerebellopontine angle includes surgical operations using modern endoscopic equipment. High-quality neuroimaging allows you to select the appropriate medical tactics and determine the approach for the best removal of the tumor.
The neurosurgeon primarily uses endotracheal anesthesia and modern inhalation anesthetics. The patient is in a sitting position. The removed tumor tissue can be subjected to additional studies in order to make a full prognosis for the future.
It is very important to contact a neurosurgeon at the first signs of the development of the disease. At the initial stage of tumor growth, microsurgical techniques are used to preserve the functionality of the nerve structures. In this case, specialists use translabyrinthine access to the tumor. If the size of the tumor does not exceed a few centimeters, it is possible to maintain full hearing for the patient. The severe stage of the disease requires the use of the posterior cranial fossa as a surgical approach.
The method of surgical treatment of a tumor is determined by the size of the tumor and its location. The neurosurgeon selects the appropriate tactics based on the results of a comprehensive diagnosis and assessment of the patient’s general condition.
Radiation therapy is used for subtotal removal of a tumor and is an auxiliary technique. But their effectiveness has not been proven to date. The only reasonable solution is to have surgery performed in a qualified medical facility. Most of such operations in the country are carried out at the Burdenko Research Institute. It has the necessary technical equipment for effective surgical treatment of brain tumors of various locations. Specialists use all available capabilities of modern neurosurgery to treat patients and prevent life-threatening complications.
Post-Covid syndrome
Many people who have recovered from coronavirus, even in a mild form, note that they experience various negative sensations in the body even months after recovery. Currently, a specialized term has emerged to define this condition—post-Covid syndrome.
Post-Covid syndrome
(English Post-COVID-19 syndrome), also known as Long Covid, is the consequences of coronavirus infection (COVID-19), in which up to 20% of people who have had coronavirus infection suffer from long-term symptoms lasting up to 12 weeks and 2. 3% of cases are longer. But there is no exact time frame for when post-Covid syndrome will appear. This can happen shortly after discharge and after three months. Moreover, a mild form of Covid is not a guarantee of the absence of post-Covid syndrome. In December, the UK Office for National Statistics estimated that one in 10 people who contracted coronavirus went on to suffer long-term symptoms that lasted three months or more.
The main damage caused by coronavirus infection is diagnosed in the lungs. But among all Covid patients, severe lung damage is only a few percent. The majority were ill without such lung damage. The virus, entering the nervous system through the olfactory receptors in the superior nasal concha, can directly damage the structures of the brain, respiratory and other centers. The virus causes inflammation of the heart muscle (myocarditis) and cerebral ischemia. ACE2 receptors, to which the covid virus attaches, are found in any human tissue. Their maximum number is in the intestines, with the heart and lungs in second and third place. And since blood is delivered to all organs and tissues, absolutely any body system can be affected.
Post-Covid symptoms include problems that arise in waves or on an ongoing basis, such as:
Ø Weakness
, paralyzing weakness - many patients who have suffered a covid infection continue to have such severe weakness that it does not allow them to perform their usual activities, even reducing the ability to perform normal self-care, and not being able to visit a store or other essential places.
Ø Shortness of breath, feeling of lack of air
, incomplete inspiration, apnea, heaviness behind the sternum,
discomfort in the chest
, and all this can be without significant damage to the lungs, normal indicators in control x-rays and CT studies.
Ø In varying degrees of severity, almost all those who have recovered from the disease experience mental disorders
: tearfulness, bad mood, depressed mood, sleep disturbance, suicidal thoughts;
Cognitive impairment
is often observed (memory loss, brain fog, spatial disorientation, anxiety and panic attacks).
Ø Violation of body thermoregulation
: not only an increase of 37.0 -37.4 C, but also a decrease in body temperature: 35.5 C or 36.0 C. And this can persist for a long time; Such a temperature during post-Covid syndrome, as a rule, is not regulated by anything.
Ø Loss of smell, distortion of smell/taste
may remain the same for quite a long time, but occurs much less frequently than other symptoms.
Ø Severe headaches
, not in any way related to temperature or increased blood pressure,
muscle
pain joint pain
;
paresthesia
is noted - a feeling of “pins”, “goosebumps”, burning and other unpleasant symptoms that everyone has experienced in life, for example, after serving a leg or resting an arm. But if in such cases the sensations quickly pass, then after Covid such neurology appears again and again.
Ø Some people who have been ill may develop skin lesions
, various rashes: vascular and vasculitic manifestations on the skin, other skin reactions (extensive urticaria, capillary networks). Sometimes, due to infection, the skin on the hands and feet becomes like frostbitten: the top layer peels off, and red or purple painful bumps appear on the fingers and another “skin” symptom is dry and “scaly” lips. They may also have small cracks.
Ø In patients who have suffered severe forms of coronavirus infection, hair loss
;
Some people experience tooth loss
and cystic formations in the jaw cavity.
Ø Gastrointestinal disorder
, diarrhea that occurs in waves and does not depend on diet or medication is more common in patients who previously suffered from gastrointestinal pathology and (or) received massive antibiotic therapy during the acute period of the disease.
Ø In patients, even those who have not previously suffered from arterial hypertension, there are sharp jumps in pressure and pulse, arrhythmias , tachycardia
(including orthostatic tachycardia, i.e. palpitations when changing body position), dizziness, and in some recovered patients
an increase in cholesterol levels
in the blood is detected.
Should those who have been ill asymptomatically be concerned?
If there are no symptoms (of post-Covid syndrome), then you should live peacefully. Because the race for examinations is already a hypochondriacal topic.
But if a person has suffered from Covid
and he has some symptoms, then
you should consult a general practitioner
or medical specialists
in the profile of the most significant symptoms you have
. Currently, there are no approved protocols for the treatment of post-Covid syndrome; specialists in various fields are treating the consequences.
Therefore, it is worth talking a little more about the causes and manifestations of post-Covid syndrome and what to do when they appear.
Persistent weakness and shortness of breath
may indicate decreased cardiac function. Mainly concerns patients who have recovered from moderate and severe forms of Covid. In many patients, there is also a tendency to increase blood pressure due to a decrease in the elasticity of the vascular walls throughout the body. German doctors, in a recent study, found heart damage in 78 out of 100 people who had the infection, even if they had no previous heart problems. Delayed diagnosis of complications and lack of treatment can cause irreversible changes in the heart muscle and lead to chronic rhythm disturbances and heart failure, while uncontrolled hypertension and high cholesterol levels can cause stroke and heart attack. Such people are recommended to have an ECG and detailed echocardiography (the same as an ultrasound of the heart), and visit a cardiologist in order to identify signs in time and begin treatment.
Long-lasting shortness of breath
may also be a sign of the development of fibrosis of the lung tissue, and this is the most dangerous because this change is already irreversible. Pulse oximetry can determine the presence of lung damage. A blood saturation level below 94% is considered alarming. A persistent decrease in oxygen saturation may indicate ongoing lung damage. But in this case, you should not immediately panic, since in most cases, covid does not reach fibrosis, the lungs are restored. However, it is worth trying using various methods to prevent further deterioration of the condition by obtaining treatment recommendations from a general practitioner or pulmonologist. Therapy, as a rule, includes taking acetylcysteine, vitamins E, antioxidants - all this really allows you to achieve improvement until complete recovery. But this does not happen quickly - up to six months.
In most cases, the sense of smell is restored on its own: sometimes in 2-3 weeks, sometimes in a month, in rare cases - in 2-3 months. Loss of smell
You should not try to forcefully return smells in the first 2-3 weeks of illness. And then gradually and carefully you can try different recovery methods. According to the recommendation of Pavel Evdokimov, a member of the Russian Academy of Medical and Technical Sciences, the process can be accelerated by using eucalyptus if you do not have allergies. You need to drop 10-15 drops of eucalyptus tincture into a glass of hot water and just breathe over this glass for 2-3 minutes. You can also use a nebulizer device for these purposes. Another way is to buy saline solution at the pharmacy and drop it shallowly into your nose through a pipette twice a day, then hold it for a little while and blow your nose thoroughly. You can also replace the saline solution with a glass of warm boiled water, half a teaspoon of salt and a drop of iodine. If these steps do not help you, you need to contact an otolaryngologist and neurologist.
Reduced temperature
after covid, this is, as a rule, not a dangerous symptom, but simply a special reaction of the body. This often occurs after a viral infection: the body is too exhausted, it has nowhere to get strength, there is a general decrease in body functions due to improper production of hormones, and there is no need to equalize the temperature and activity, which warmth gives us. A decrease in temperature may also indicate that during illness the regulation of metabolism in the body is disrupted. However, do not forget that low temperature also occurs in hypothyroidism, oncology, central nervous system oncology, central nervous system injuries and liver diseases, and is a symptom of the use of certain medications. Therefore, in the event of a violation of post-Covid thermoregulation, it is necessary to carefully monitor the general condition of the body and undergo a minimum of tests that monitor the functioning of the thyroid gland and liver, and, if necessary, consult an endocrinologist and immunologist.
Nervous tissue is most susceptible to toxins; general intoxication of the body has a detrimental effect on nervous tissue. For memory loss and similar cognitive impairments
, for example, loss of orientation in space, poor sleep, those who suffered from moderate or severe Covid complain. Today it is believed that cognitive impairment in those who have recovered from the disease will disappear, but the exact time frame for self-recovery has not yet been announced. To speed up recovery, the manifestation of these syndromes is treated by neurologists and psychotherapists who prescribe courses of nootropic drugs, sedatives, sedatives, antidepressants and other drugs.
We are all different, and the consequences of coronavirus infection manifest themselves differently in everyone. The same symptom, for example, difficulty breathing, can be either a minor symptom of disturbances in the functioning of the autonomic nervous system - autonomic dystonia, or a serious symptom of inflammation of the heart muscle - viral myocarditis. Therefore, under no circumstances should you self-medicate.
, haphazardly take medications - especially coagulants. This can cause bleeding disorders and internal bleeding.
To speed up recovery, we advise you to analyze your condition and follow all the recommendations of your doctor. The list of rehabilitation measures depends on the individual characteristics of the patient and may consist of the following elements:
· therapeutic exercises;
· breathing exercises using respiratory simulators;
· massage;
· psychotherapy;
· diet therapy;
· physiotherapeutic procedures.
To make it easier for the doctor to select a therapeutic regimen, patients are advised to
:
1. Monitor lung function, blood pressure and heart rate. The presence of signs of difficulty breathing indicates that you need to do more breathing exercises and spend more time in the fresh air.
2. If muscle weakness occurs, slowly and gradually increase physical activity.
3. Take vitamin-mineral and amino acid complexes that help strengthen the immune system. The most important vitamins for post-Covid syndrome are A, D, E, C. Amino acid complexes compensate for the lack of protein in the body, which affects the production of immunological protective antibodies.
4. In case of loss of voice and difficulties with swallowing, it is recommended to correct the diet - switching to fractional meals and small portions to relieve the muscles of the larynx. The exercise therapy complex includes exercises for ligaments.
5. If previously unknown symptoms appear or existing symptoms intensify, consult a medical specialist in a timely manner.
Thus, Post-Covid syndrome is a rather complex and dangerous condition that can affect the physical and psychological state of a person. If you are unable to recover from coronavirus on your own, then you should contact a specialist who will develop an individual course of rehabilitation therapy.
Deputy Head of Medical Sciences,
cardiologist of the highest category
Zabiran Irina Vasilievna