Injury - one of the most common types of injuries. With such damage, soft tissues suffer, but the integrity of the skin is not compromised. Such injuries often occur when struck with a blunt object, falls from a height onto a flat surface and can be combined with fractures, dislocations, scratches, and abrasions.
In addition to bruises of individual parts of the body, there are also bruises of internal organs.
As a rule, special treatment for bruises is not required. However, if you have pain for a long time after the injury, for example, a sore elbow or back pain, you should consult a doctor.
1
Treatment of bruises and hematomas
2 Treatment of bruises and hematomas
3 Treatment of bruises and hematomas
Causes
Hemorrhage usually occurs after injury. This could be a bruise of the skin, internal organs, a concussion or bruise of the brain, an injection with thin (sharp) objects. Sometimes blood leaves the vessels and pours into the skin and internal organs as a result of infections, autoimmune diseases, and poisoning. The occurrence of hemorrhages and bruises is promoted by increased fragility of blood vessels, fasting, lack of vitamins in food, high blood pressure, and congenital bleeding disorders.
At CELT you can get a consultation with a traumatologist-orthopedic specialist.
- Initial consultation – 3,000
- Repeated consultation – 2,000
Make an appointment
Symptoms
A bruise on the skin is always clearly visible. At first it has a purplish-blue color, and then begins to “bloom”, acquiring yellow and green colors. If a sufficiently large amount of blood accumulates under the skin, a protruding lump forms. At first it is very painful to feel, but later the pain goes away.
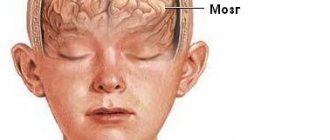
The outpouring of blood into the internal organs and into the substance of the brain is preceded by trauma. The main symptom is pain. In this case, the hematoma is not visible externally. If bleeding continues, the victim becomes pale, weak, and dizzy. With chronic internal bleeding, anemia comes to the fore. Bleeding in the brain is especially dangerous. Compression of brain structures may occur, sometimes leading to death.
Types and typology
The classification of hematomas is varied and depends on factors such as: clinical signs, the condition and substance of the blood that has been shed, and the location of the hematoma.
The following types are distinguished:
- Pulsating hematoma. It is characterized by pale skin around the source of inflammation, low temperature in relation to the body. Sometimes doctors mistake it for an abscess or inflammatory infiltrate (accumulation of blood and lymph in the tissues). The limb may not be fully functional. On palpation, pulsation is felt;
- Non-pulsating. Has the same signs, except for pulsation;
- Curled up. Occurs in a cavity with thickened (coagulated) blood;
- Infected hematoma. Occurs in old age or in people with weak immunity. It develops when an infection gets into damaged tissues.
- Suppurative is the definition of a hematoma, the symptoms of which are characterized by the release of pus from the wound, and blood clots may also appear. To prevent the festering area from leading to death or amputation, surgical intervention is necessary. After the operation, so that the wound stops festering, the doctor will prescribe special ointments and medications.
- Subserous subcutaneous hematoma. It differs in the location of blood accumulation. It is located under the surface layer and increases towards the abdominal or thoracic cavity. In this case, medical assistance is mandatory.
- Intramuscular hematoma. It is characterized by increased body temperature, the appearance of a bluish swelling, pain on palpation and decreased mobility of the injured area of the body.
- Subdural - occurs as a result of traumatic brain injury, blood flows into the cavity between the arachnoid and dura mater of the brain. The consequences may be increased pressure in the cranial cavity, damage to the brain substance, as well as swelling. Hematomas in this area of the body are divided into the following subtypes:
- Spicy. They have a high mortality rate (60%) and require surgical intervention, namely decompression. Venous hemorrhage in acute subdural hematomas develops very quickly;
- Chronic. After an injury, chronic SDH can form from several days to several weeks. In this case, the person will not even realize that his life is in danger in the form of a developing hematoma in the cranial area. Therefore, after a head injury, it is always recommended to undergo a medical examination;
- Subacute. Characterized by the slow development of compression syndrome. Sometimes doctors mistake it for a regular bruise, or even meningitis or the flu. Symptoms appear within three days.
Separately, subcutaneous, intracranial, submucosal, tension, paraorbital, intracerebral, epidural and retrochorial hematomas should be identified.
- Subcutaneous hematoma is the concentration of blood in the subcutaneous fat tissue, regardless of its substance (liquid, coagulated). A subcutaneous hematoma is formed as a result of injury and further purulent-necrotic inflammation of the skin and tissue. It is detected using ultrasound, MRI, and puncture. Subcutaneous hematoma has a longer “blooming” period, so it is not always possible to recognize it immediately. This is due to large hemorrhage in the affected area.
- Intracranial (internal hematoma) - formed as a result of a bruise and further hemorrhage into the cranial cavity, damaging the nervous tissue and disrupting its blood supply. Medical attention required.
- Submucosa. The localization site is the mucous membranes, which makes it difficult to access for surgical intervention.
- Intracerebral. It is detected based on tomography results, which indicate that the focus of the hemorrhage has reached the cellular elements of the brain and has an increased density. It can develop either quickly or delayed – over several months.
- Tension hematoma - such hematomas are located on the hip area, as well as in the buttocks area.
- Paraorbital. It forms in the eye area and has nothing in common with an ordinary bruise. It is distinguished by hemorrhage into the periorbital tissue surrounding the eye.
Predisposing factors
The formation of hematomas occurs after injuries, including pinching, blows, squeezing, and bruises. Subarachnoid hemorrhage does not fall into this category, since it does not appear due to trauma, but due to damage to an unchanged vessel. Often small hematomas appear due to eating large quantities of food or drinking alcoholic beverages. This is due to stretching of the gastrointestinal tract and the appearance of cracks.
The development of pathology is influenced by vascular weakness and problems with blood clotting. Often due to a weakened immune system due to infections or age-related changes, the likelihood of pus accumulating in the affected area increases.
Classification of hematomas
In modern medicine, when classifying hematomas, the following are taken into account:
- Relation to the vessel - pulsating and non-pulsating hematomas.
- Localization - in the cranial cavity, internal organs, under the skin or mucous membrane.
- The state of the blood in the affected area is suppurated, clotted, fresh, infected.
- Symptoms – limited, encysted, diffuse.
There are hematomas that do not fall into this classification. For example, intracerebral, intracranial, intraventricular. They are of the epidural or subdural type and cause serious complications.
Treatment of hematoma
The best remedy for hematomas under the skin is rest, cold compresses, a pressure bandage and an elevated position of the limb. Additionally, you can use painkillers (paracetamol). An ointment for hematomas from the group of NSAIDs or antithrombotic drugs will also help. Folk remedies include compresses made from cottage cheese, onion, garlic, St. John's wort, wormwood, celandine and aloe.
How to treat a hematoma that has arisen in the abdominal cavity: if it is small in size and the patient’s condition is stable, doctors limit themselves to observation; if symptoms of blood loss or shock develop, they provide appropriate treatment in a hospital.
Treatment of a hematoma that occurs inside the skull also depends on its size and the degree of impairment of brain function. Some patients only require observation; in other cases, surgery to remove the blood clot is indicated.
Soft tissue hematomas
Soft tissue hematomas are divided into 3 types:
- Lungs - appear 24 hours after injury and are accompanied by mild pain. No special treatment is required.
- Medium - appear within 5-6 hours and are accompanied by pain and swelling. The motor function of the limb deteriorates. Consultation with a traumatologist is required.
- Heavy - formed within 2 hours after tissue damage. The function of the limb is impaired, acute pain and diffuse swelling are observed. You should immediately consult a doctor to determine a treatment strategy.
Immediately after the injury, swelling appears, and the skin acquires a purplish-bluish tint. After 5 days, the skin takes on a green tint as hemoglobin breaks down. Gradually, the hematoma resolves and “flows” down.
If there are no complications, the hematoma will resolve on its own. In the worst case, a hard area appears that causes discomfort and impairs motor function. When an intramuscular lump forms, external symptoms are rarely observed, but the limb swells significantly and an area forms inside, the touch of which causes severe pain.
Note! For chronic intramuscular hematomas, an MRI is prescribed to determine the location and extent of tissue damage.
When large lumps form, surgical intervention is required. Treatment is carried out by a traumatologist. The opening of infected seals is performed by a surgeon after a comprehensive diagnosis. The operation is performed on an outpatient basis, but for large hematomas hospitalization is required. An autopsy is performed, during which blood clots are removed and washing is carried out. Drainage and suturing are required. Sutures are not applied only for infected hematomas. Antibiotics are often prescribed in combination to eliminate the infection.
Causes, symptoms and diagnosis of hematomas
Vessels are often damaged, leading to hemorrhages into the surrounding tissue. Depending on their type, size and location, hematomas can be minor or even cause life-threatening damage. The highest risk of this pathology is in people who constantly take blood thinners. Head injuries must be taken especially seriously, since they can be accompanied by bleeding with subsequent formation of intracranial and intracerebral hematomas.
The most common causes of hematoma:
- vascular injury due to soft tissue contusion;
- taking anticoagulant and antiplatelet drugs;
- decreased platelet count (thrombocytopenia);
- platelet dysfunction (thrombopathy);
- disorders of the plasma hemostasis (for example, hemophilia);
- some infectious diseases, for example, panaritium, ankylosing spondylitis, fungal nail infection;
- trauma to the nose, blunt injuries to the abdomen from a blow;
- bone fracture or hematoma after surgery on the musculoskeletal system;
- hematoma during early pregnancy;
- complications of pregnancy in the 3rd trimester.
Retrochorial hematoma occurs in a quarter of pregnant women. This is the most common anomaly detected by ultrasound. Typically, such hemorrhage is small in size, resolves on its own and does not harm the health of the mother and fetus.
The most dangerous hematoma during pregnancy occurs in the 3rd trimester. It may accompany placenta previa or placental abruption and requires urgent medical attention.
Symptoms of extracerebral hematomas depend on their location, size, and degree of compression of surrounding tissues. They cause redness, increased local temperature, pain and swelling of the tissues, but resolve over time. At first they have a dense structure, which then softens. The color of the skin over the hemorrhage changes from purple-bluish to yellow and brown as the blood clot disintegrates.
After a skull injury, the following signs may appear:
- severe headache, nausea, vomiting, impaired consciousness;
- different pupil diameters;
- limb paralysis;
- drowsiness;
- hearing loss;
- speech or swallowing disorders and others.
If they appear, you must urgently contact a traumatologist or neurologist.
Most hematomas do not require additional diagnostics. In some cases, a blood test and coagulogram are examined. Ultrasound or CT is used to recognize internal hemorrhages.
Intracranial hematomas
Intracranial hematomas are divided into the following types:
- Epidural.
- Subdural.
- Intracerebral.
- Intraventricular.
Epidurals appear in 1-3% of cases and are due to injury to the middle meningeal artery. Pathology is often observed with skull fractures or depressed fractures. A hematoma develops in 2-3 hours or within 24 hours. Lack of treatment leads to coma. The first symptoms are confusion and weakness. Children rarely lose consciousness after a severe blow. Significant swelling of the brain does not lead to the detection of a light gap (which is rare in adults).
Subdurals appear in 1-7% of cases and pose a threat to human life, since death occurs in 60% of cases. There is an acute, subacute and chronic form of the pathology. Bleeding occurs due to a rupture of a vein or artery in the damaged area. People report nausea and severe headaches. Symptoms characteristic of compression of the brain stem are often observed. Lack of treatment and worsening symptoms lead to coma.
Intracerebral are observed extremely rarely with severe traumatic brain injuries. The light gap is not visible, the development of pathology occurs quickly. Hemiplegia or hemiparesis often occurs, as well as extrapyramidal symptoms.
Intraventricular diseases are rarely diagnosed due to the serious condition of patients. There are acute disturbances of consciousness, an increase in body temperature, a decrease in heart rate, and an increase in blood pressure. To establish a diagnosis, a survey of close people is carried out, since the patient is unconscious. To establish the location of the hematoma, MRI is used. In the most severe cases, lombal puncture is used.
What are the symptoms of intracerebral hematoma formation?
Typically, the first symptoms begin to appear from the onset of hemorrhage, although their intensity directly depends on the severity of the lesion. Sometimes, from the moment the hematoma forms until characteristic symptoms are observed, a time may pass (from several hours to months), called the “light interval.” It is customary to distinguish symptoms:
1. cerebral – manifests itself:
- headache of sufficient intensity
- dizzy
- nausea, vomiting
- general weakness and drowsiness
- confused consciousness (sometimes preceded by psychomotor agitation), with a possible transition to coma (as with hemorrhage in the ventricles of the brain)
2. focal – correlated with the volume and localization of the hematoma, manifests itself:
- speech disorders
- difficulty swallowing
- hearing disorders (hard of hearing) and vision (nystagmus, drooping upper eyelid)
- behavior disorder
- loss of sensation in the limbs
- epilepsy attacks
- memory loss
- increased temperature (when blood enters the ventricles of the brain)
Diagnostics
A hematoma is diagnosed by visual examination. If the hemorrhage is located deep under the skin, in internal organs, or in a joint, it is often very difficult to assess its size and possible consequences.
Patients are prescribed an examination, which may include:
- Ultrasound of internal organs, joints;
- computed tomography and magnetic resonance imaging;
- puncture (puncture with a needle): for example, a puncture of the knee joint is often done if there is a suspicion that blood has accumulated in it after an injury.
Treatment
Minor bruises can be treated conservatively: physiotherapeutic procedures and medications are prescribed.
In case of large accumulations of blood, the hematoma is treated surgically: it is opened, the blood or pus is evacuated, washed with antiseptics and drainage is installed. Antibiotics are prescribed if necessary.
When hemorrhaging into internal organs, it is often necessary to perform surgical intervention, during which it is necessary not only to remove the spilled blood, but also to stop the bleeding.
The multidisciplinary CELT clinic employs experienced traumatologists and surgeons who perform operations on hematomas of various locations. Modern techniques used in our clinic help provide effective treatment and minimize the risk of complications.
3.Basic techniques for open removal of intracerebral hematomas
As already mentioned, the decision to choose a treatment method for a hematoma is based on an analysis of a number of factors. The main method of access to a hematoma for its subsequent removal is osteoplastic trephination
. During this operation, a trepanation hole is formed in the skull bone using a cut of the bone plate, through which the hematoma is then removed by aspiration (suction). After this, coagulation of the bleeding vessels is performed, the resulting blood clots are removed with special windowed tweezers, the wound is thoroughly washed with a medical saline solution (sodium chloride) and a hemostatic (hemostatic) tissue - gauze or sponge - is temporarily placed in the cavity of the removed hematoma. The stronger the compression, the wider the trepanation is performed.
There is also a less traumatic method for removing intracerebral hematoma - stereotactic aspiration
. This surgery is usually indicated for certain types of strokes. When carrying out such a surgical intervention, a special probe up to 6 mm in diameter is inserted into the hematoma cavity using monitoring equipment, through which the escaping blood is aspirated. The undoubted advantage of this technique, as already mentioned, is that it is much less traumatic compared to osteoplastic trepanation, but its disadvantage is that the surgeon is not able to carry out thorough hemostasis, which increases the risk of hematoma recurrence.
About our clinic Chistye Prudy metro station Medintercom page!
Orthopedics and traumatology services at CELT
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with a surgical doctor (primary, for complex programs) | 3 000 |
| X-ray of the chest organs (survey) | 2 500 |
| Ultrasound of soft tissues, lymph nodes (one anatomical zone) | 2 300 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions