MRI of cerebral vessels is a diagnostic procedure that allows you to assess the condition of the vessels of the head. There are no harmful factors such as radiation during MRI. The procedure is intended to identify various diseases, which will be discussed further. You will also find out what an MRI of cerebral vessels shows and when it is prescribed.
The accuracy of MRI is due to the fact that the tomograph works with signals from hydrogen nuclei (protons). While a person is in the magnetic field of the device, the protons of his body emit electromagnetic waves. With their help, the device builds an image of internal organs on a computer screen.
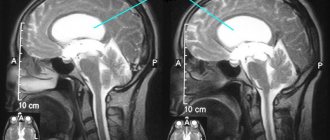
In addition to standard MRI, which is used when a tumor, multiple sclerosis and other brain pathologies are suspected, a type of method is used to examine the blood vessels of the brain. Magnetic resonance angiography (MRA) shows the arteries, magnetic resonance venography (MRV) shows the veins. From the outside it seems that there is no difference in these studies. In fact, these are separate procedures in different operating modes of the tomograph.
Image of the vessels of the head during MRI
Cerebrovascular diseases
Headache is often overlooked. Patients believe that such pain, if it is not too intense, can be ignored. People live with “ordinary” headaches for years, and during this time pathological processes occur in their brain. MRI makes it possible to distinguish migraine from, for example, an aneurysm, and psychosomatic headache from tumors and impaired blood supply to the brain.
What diseases are detected using MRI of cerebral vessels?
Most often, cerebral vessels suffer due to three pathologies: atherosclerosis, high blood pressure, type 2 diabetes, which can lead to the development of serious complications.
Stroke
A stroke is an acute circulatory disorder in the brain, a very dangerous condition that can lead to serious health consequences. MRI is often used to diagnose strokes as a high-tech method that allows one to obtain accurate images of the pathology.
Stroke is divided into several types depending on the cause:
- Ischemic. It occurs when an area of the brain stops receiving blood due to blockage of a vessel by a blood clot or cholesterol plaque. The brain matter dies, not receiving oxygen through the bloodstream. Heart failure, diabetes mellitus and atherosclerosis can contribute to the occurrence of the disease.
- Hemorrhagic. Occurs due to hemorrhage into the brain tissue from a damaged vessel. A risk factor for this type of stroke is hypertension.
Timely diagnosis of stroke is very important. Timely measures taken to identify and assess the consequences of a stroke help to begin early rehabilitation and restore damaged functions.
In the event of a stroke, MRI gives a clear and detailed picture of the course of the disease, the location and extent of brain damage.
Atherosclerosis
This disease develops to one degree or another in almost every adult, but the severity of the disease and the speed of its development are strictly individual. When the disease occurs, cholesterol and fats are deposited in the artery wall and a plaque forms. The following options for the development of the disease are possible:
- the plaque narrows the lumen of the vessel, the brain does not have enough blood;
- expansion of the artery walls (aneurysm) is formed;
- the vessel wall ruptures with subsequent bleeding;
- a blood clot forms at the site of the plaque, further interfering with the movement of blood;
- the contents of the plaque and/or the thrombus breaks off and clogs the vessel.
The following diseases contribute to the emergence and rapid progression of atherosclerosis:
- High blood pressure (arterial hypertension, hypertension) damages the vessel wall, which becomes less elastic and cannot cope with the load. Fats are deposited in it more easily and atherosclerosis develops. Due to high pressure, thin or severely damaged vessels, such as vessels with an aneurysm, rupture.
- Diabetes mellitus type 2. Excess glucose also damages the vessel wall. People with type 2 diabetes mellitus develop atherosclerosis and hypertension more quickly. Often one person has a combination of atherosclerosis, hypertension and type 2 diabetes mellitus. They reinforce each other and increase the risk of stroke.
- Heart diseases (heart rhythm disturbances, myocardial infarction, heart defects).
Conditions that are less common: autoimmune diseases (vasculitis, systemic lupus erythematosus, type 1 diabetes, etc.), infectious diseases, sepsis, traumatic brain injuries.
Cerebral small vessel disease
A new diagnostic method sometimes opens up a whole world of diseases about which not much was known before. MRI technology helps study a group of diseases of small vessels in the brain, those with a diameter of less than 2 mm.
Small vessel disease of the brain is dangerous for cognitive decline and/or stroke. About a quarter of ischemic strokes occur due to capillary damage. There are many causes of damage to small vessels and they are still being studied.
Some older people may develop cerebral amyloid angiopathy. It affects approximately 20% of people 61-70 years old; The older the age, the more often it is detected. A special protein called amyloid is deposited in the brain vessels, gradually the blood supply to the brain is disrupted and neurons die.
Aneurysm
An aneurysm is a pathological enlargement of an artery, which occurs on average in 2-3 people out of 100. The disease occurs more often in women, as well as in the age group over 30 years. Aneurysms can be congenital, but over time, the vessel wall is also deformed by atherosclerosis, blood pressure, trauma, and an infectious process, which aggravates the course of the disease.
A vessel affected by an aneurysm may burst. Most often, the gap occurs between the ages of 20-40 years. Before this, a person may suffer from headaches similar to a migraine attack. MRI is indispensable for early diagnosis of the disease. Modern tomographs are capable of visualizing even the slightest pathological lesions in the brain with great accuracy.
Risk factors for the formation of aneurysms include smoking, high blood pressure, the use of hormone replacement therapy during the postmenopausal period, and if there are people in the family with aneurysms and other diseases of the cardiovascular system.
Angioma (vascular malformation)
A benign tumor consisting of overgrown and intertwined veins and arteries of the brain. The formation does not pose a threat to life, but as it grows, it can compress the structures of the brain, resulting in headaches and disrupting the normal functioning of the areas of the brain near which the pathology is located.
Based on size, malformations are divided into:
- Capillary. They consist of tiny vessels and usually do not cause symptoms.
- Venous. Includes larger veins and arteries. May cause specific symptoms.
- Tricky. The vessels intertwine so closely that they form entire cavities in which blood accumulates. Such a tumor can grow quite strongly and put pressure on the brain tissue.
The causes of angiomas have not been fully studied. Often the disease is congenital or occurs in early childhood. A small percentage of angiomas occur after infectious diseases.
MRI of the brain vessels will accurately show not only the location, size and shape of the tumor, but also the degree of compression of the surrounding tissues. Thanks to magnetic resonance imaging, the attending physician will be able to develop an effective plan for subsequent therapy.
Discirculatory changes
Focal changes in the white matter of the brain due to impaired vascular trophism are the most common occurrence when analyzing MRI scans in older patients. They are considered to be caused by chronic hypoxia and dystrophy due to damage to small arteries and arterioles.
decreased blood flow is one of the main causes of age-related changes in the brain
MRI signs of vascular lesions:
- Multiple focal changes in white matter, mainly in the deep structures of the brain, not involving the ventricles and gray matter;
- Lacunar or border areas of necrosis;
- Diffuse lesions in the deep sections.
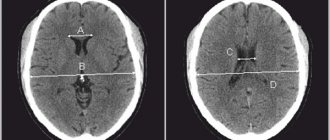
foci of lacunar microstrokes in the brain
The described picture may resemble that of age-related atrophy, therefore it can be associated with dyscirculatory encephalopathy only if the corresponding symptoms are present. Lacunar infarctions usually occur against the background of atherosclerotic lesions of cerebral vessels. Both atherosclerosis and hypertension give similar changes on MRI in a chronic course, can be combined and are characteristic of people after the 50th birthday.
Diseases accompanied by demyelination and a diffuse dystrophic process often require careful differential diagnosis, taking into account symptoms and medical history. Thus, sarcoidosis can simulate a variety of pathologies, including multiple sclerosis, and requires contrast-enhanced MRI, which shows characteristic focal changes in the basal ganglia and meninges.
In Lyme borreliosis, the most important facts are a tick bite shortly before the onset of neurological symptoms and a skin rash. Focal changes in the brain are similar to those in multiple sclerosis, measure no more than 3 mm and are combined with changes in the spinal cord.
How to do an MRI of cerebral vessels
After the patient enters the radiologist's office, the doctor asks several questions about bothersome symptoms and contraindications for the procedure. The patient is asked to remove all metal objects and lie down on the tomograph bed. Normal operation of the tomograph is accompanied by noise, knocking and other loud sounds; this should not be alarmed. In our medical center, each patient is given headphones that play pleasant, calm music during the examination.
Preparation for MRI of the head and blood vessels
The patient is given a special button in his hand, which can be pressed during the procedure to inform the doctor about a sudden deterioration in health.
MRI of cerebral vessels - indications and contraindications
Magnetic resonance imaging of cerebral vessels is used in the presence of a wide range of symptoms that may indicate vascular pathology and circulatory disorders.
- headaches of varying duration and severity;
- dizziness;
- noise in ears;
- seizures similar to epileptic;
- unsteady gait, loss of coordination;
- changes in sensation of temperature, touch;
- deterioration of attention, memory;
- difficulties with understanding speech and pronouncing words;
- traumatic brain injuries.
If one or more of the symptoms described above occurs, you should consult a doctor and undergo an MRI scan to make sure there are no cerebral vascular pathologies.
Despite its safety, MRI still has a number of contraindications, in the presence of which the procedure is impossible.
- The tomograph is not designed for body weight more than 130 kg or chest (hips, abdomen) girth more than 150 cm.
- The magnetic field of the tomograph can disrupt the functioning of a pacemaker, neurostimulator, or cochlear implant - the presence of these devices is an absolute contraindication for the study.
- Magnetic metal (shards, shot, metal shavings) inside the body can shift under the influence of a magnetic field and damage surrounding tissue.
- MRI is not done in the 1st trimester of pregnancy and in children under 5 years of age.
Prostheses made of non-ferromagnetic materials allow MRI to be performed if the following conditions are met:
- there are documents for the prosthesis;
- more than 3 months have passed since installation;
- the prosthesis is not installed in the scanning area.
There are MRI-compatible pacemakers and other electronic implants. If there are any medical devices in the patient’s body, it is necessary to study the product passport for the possibility of conducting magnetic resonance imaging.
Manifestations of focal changes in brain matter
The brain is supplied with blood from two vascular basins - the carotid and vertebral arteries, which already have anastomoses in the cranial cavity and form the Circle of Willis. The possibility of blood flow from one half of the brain to the other is considered the most important physiological mechanism that allows one to compensate for vascular disorders, so the clinical picture of diffuse small-focal changes does not appear immediately and not in everyone.
At the same time, the brain is very sensitive to hypoxia, so long-term hypertension with damage to the arterial network, atherosclerosis, which impedes blood flow, inflammatory changes in blood vessels and even osteochondrosis can lead to irreversible consequences and cell death.
Since focal changes in brain tissue occur due to a variety of reasons, the symptoms may be different. Dyscirculatory and senile changes have similar features, but it is worth remembering that lesions in relatively healthy people are unlikely to have any manifestations.
Often changes in brain tissue do not manifest themselves at all, and in elderly patients they are even regarded as an age-related norm, therefore, with any MRI conclusion, its result should be interpreted by an experienced neurologist in accordance with the symptoms and age of the patient.
If the report indicates focal changes, but there are no signs of trouble, then there is no need to treat them, but you will still have to see a doctor and periodically monitor the MRI picture in the brain.
Often, patients with focal changes complain of persistent headaches, which are also not necessarily associated with the identified changes. You should always rule out other causes before you start “fighting” an MRI picture.
In cases where the patient has already been diagnosed with arterial hypertension, cerebral or neck atherosclerosis, diabetes, or a combination of these, it is very likely that an MRI will show corresponding focal changes. Symptoms may include:
- Emotional disorders - irritability, mood swings, tendency to apathy and depression;
- Insomnia at night, drowsiness during the day, circadian rhythm disturbances;
- Decreased mental performance, memory, attention, intelligence;
- Frequent headaches, dizziness;
- Disorders of the motor sphere (paresis, paralysis) and sensitivity.
Initial signs of dyscirculatory and hypoxic changes do not always cause concern in patients. Weakness, fatigue, bad mood and headaches are often associated with stress, overwork at work and even bad weather.
As diffuse changes in the brain progress, behavioral inappropriate reactions become more pronounced, the psyche changes, and communication with loved ones suffers. In severe cases of vascular dementia, self-care and independent existence become impossible, the functioning of the pelvic organs is disrupted, and paresis of certain muscle groups is possible.
Cognitive impairment almost always accompanies age-related degenerative processes with brain dystrophy. Severe dementia of vascular origin with multiple deep foci of rarefaction of nervous tissue and atrophy of the cortex is accompanied by memory impairment, decreased mental activity, disorientation in time and space, and the inability to solve not only intellectual, but also simple everyday problems. The patient ceases to recognize loved ones, loses the ability to produce articulate and meaningful speech, becomes depressed, but can be aggressive.
Against the background of cognitive and emotional disorders, the pathology of the motor sphere progresses: gait becomes unstable, trembling of the limbs appears, swallowing is impaired, paresis increases up to paralysis.
Focal changes of a post-ischemic nature are usually associated with strokes suffered in the past, so symptoms include paresis and paralysis, disorders of vision, speech, fine motor skills, and intelligence.
In some sources, focal changes are divided into post-ischemic, dyscirculatory and dystrophic. You need to understand that this division is very arbitrary and does not always reflect the symptoms and prognosis for the patient. In many cases, dystrophic age-related changes accompany dyscirculatory changes due to hypertension or atherosclerosis, and post-ischemic foci may well arise from existing disseminated vascular origin. The emergence of new areas of neuronal destruction will aggravate the manifestations of existing pathology.
Contrast MRI of cerebral vessels
Magnetic resonance angiography (MRA) creates images based on signals from hydrogen atoms, which are abundant in blood and other fluids. The image on the monitor screen is very clear, so a contrast agent is rarely required. When performing computed tomography, unlike MRI, contrast is used much more often.
In MRI diagnostics, substances based on gadolinium are used. A contrast agent is injected into a vein, changing the magnetic properties of the tissue for a short time, and is excreted through the kidneys. It was possible to create gadolinium compounds that rarely cause unwanted and allergic reactions. There is no evidence that they cause neurological problems after contact with the human body. However, they are used with caution in severe kidney disease.
Before a contrast study, be sure to tell your doctor about:
- pregnancy (confirmed or probable);
- breastfeeding;
- kidney diseases;
- previous allergic reactions to any medications.
Contrast makes it easier to decipher images, as it shows the condition of the vessels in more detail.
Gadolinium-based contrast agent
Clinic, diagnosis and treatment of chronic fatigue syndrome
N.V. PIZOVA
, MD, PhD, Professor,
Department of Neurology and Medical Genetics with a Course of Neurosurgery, Yaroslavl State Medical University
The article discusses the causes, clinical manifestations and modern approaches to the diagnosis and treatment of patients suffering from chronic fatigue syndrome (CFS). The data from studies confirming the positive effect of multivitamin complexes on cognitive and other neurological functions in patients with CFS are presented.
Chronic fatigue syndrome (CFS) is a common disease, the main symptom of which is unmotivated severe general weakness, which takes a person out of active daily life for a long time, and is associated with significant socio-economic problems [1, 2]. The prevalence of CFS ranges from 0.007 to 2.8% among adults [3–5] and depends on different definitions [6], the target population and the research methods used [7]. CFS affects predominantly young, most able-bodied people in professions that require increased intelligence, a high level of emotional stress, and often speed of response and intelligence (doctors, teachers, lecturers, journalists, managers, etc.). The majority of people diagnosed with CFS are between 25 and 45 years of age, and most studies show that women are predominantly affected [3, 5]. The incidence of CFS in women is 522 cases per 100,000 and 291 in men [5]. CFS also occurs in children and adolescents, but more rarely [8]. For the first time, such diverse symptoms as chronic (recurrent, but always debilitating) fatigue, musculoskeletal pain, sleep disturbance, deterioration of short-term memory and concentration, headache, were combined into a single syndrome called “neurasthenia” in 1860 by George Beard. CFS was first identified as an independent disease in 1988 by the Centers for Disease Control (CDC, Atlanta, USA). In recent years, it has been defined as a separate nosological entity (ICD10 code D86.9).
The causes of CFS still remain unknown. One of them remains the infectious, or viral, theory. Epstein-Barr virus, cytomegalovirus, herpes simplex viruses types I, II, VI, Coxsackie virus, hepatitis C, enterovirus, retrovirus can serve as trigger factors for CFS [9]. In most studies, the main etiological reasons noted a decrease in cerebral blood flow in certain areas of the brain [10-13], an increase in lactate in the cerebrospinal fluid [14], a disrupted rhythm of cortisol release and a decrease in its amount in the blood of patients due to increased activity of the hypothalamus. pituitary-adrenal system [15-17], decrease in brain-derived neurotrophic factor (BDNF) [18, 19], changes in the serotonergic neurotransmitter system [20-22], activation of the brain cytokine system [23, 24].
Numerous data point to the role of immunological disorders in CFS [25]. In the literature, objective indicators describe a decrease in IgG due primarily to G1 and G3 classes, the number of lymphocytes with the CD3 and CD4 phenotype, natural killer cells, an increase in the level of circulating complexes and antiviral antibodies of various types, an increase in β-endorphin, interleukin-1 and interferon , as well as tumor necrosis factor [26].
Some researchers have noted the presence of an imbalance in the autonomic nervous system in CFS. M. Pagani et al. (1999) showed that in CFS, there is a predominance of sympathetic stimulation from the sinoatrial node at rest and a decrease in the response of the heart muscle to excitatory stimuli [27]. Data have been obtained on the lack of endorphins and other neurotransmitters in people with CFS.
Magnesium deficiency plays an important role in the pathogenesis of CFS. A significant portion of magnesium (39%) is found inside cells, and about 80-90% of intracellular magnesium is formed in complex with ATP. Magnesium is a cofactor for more than 300 enzymes that regulate various body functions [28]. It plays a leading role in energy, plastic and electrolyte metabolism, acts as a regulator of cell growth, and is necessary at all stages of protein synthesis. It is believed that the symptoms of CFS are, at least in part, a consequence of impaired cellular metabolism [29]. Several nutrients are required to produce ATP, including magnesium, malic acid, and active forms of vitamin B. Deficiencies of these ingredients contribute to metabolism switching to the less efficient anaerobic pathway [30]. This, in turn, contributes to a pathological increase in lactic acid levels even after slight physical exertion, which is clinically manifested by fatigue, weakness, pain and muscle spasms.
A number of studies indicate that oxidative stress plays a central role in the development of CFS [31–33]. Oxidative stress leads to damage to the most important polymers - nucleic acids, proteins and lipids of cell membranes, polyunsaturated fatty acids, inactivation of endogenous nitric oxide (NO) with the formation of toxic peroxynitrites. Recent studies have shown that patients with CFS have lower plasma transferrin levels and higher lipoprotein oxidability [34]. Pall et al. [35] believe that a vicious cell cycle with excessive accumulation of nitrogen nitrite, its oxidation products, and peroxynitrite underlies the manifestations of CFS.
Studies of patients with CFS have established a clear connection between plasma carnitine levels and the risk of developing CFS. Moreover, it was found that the degree of carnitine deficiency is directly related to the severity of CFS symptoms. That is, the less carnitine (and its esters) is contained in a person’s blood plasma, the lower his performance and the worse his health [36].
Early studies showed the presence of changes in the white matter of the brain in individuals with CFS [37–40]. In recent years, studies have appeared on the state of the gray matter of the brain in such individuals ( Table 1
) [41—45].
| Table 1. Changes in brain gray matter volume in CFS according to various studies | ||||
| Year, author | Result | Result | ||
| Gray matter | Region | White matter | Region | |
| Okada et al, 2004 [41] | Decrease | Bilateral prefrontal | Not significant | |
| de Lange et al, 2005 [43] | Decrease | Global, no special regions | Not significant | |
| de Lange et al, 2008 [44] | Increase | Prefrontal | Not significant | |
| Barnden et al, 2011 [45] | Not significant | Not significant | ||
| Puri et al, 2012 [42] | Decrease | Occipital lobes, right angular gyrus and posterior parts of the left parahippocampal gyrus | Decrease | Left occipital lobe |
According to the literature of recent years, important aspects related to the volume of gray matter of the brain in patients with CFS and its symptoms such as the presence of chronic pain, personality, stress, mental disorders, physical activity and sleep disorders are summarized ( Table 2
).
| Table 2. Changes in the volume of gray matter of the brain under various factors | |
| Factor | Region |
| Chronic pain | Cingulate cortex, prefrontal cortex, insula, dorsal pons [46] |
| Personality Features | Orbitofrontal region, occipital and parietal cortex, anterior prefrontal cortex (in women) [47] |
| Stress | Right orbitofrontal region of the prefrontal cortex [48–50] |
| Mental disorders | Amygdala, hippocampus and parahippocampal region, ventral, medial temporal lobe, insular cortex [51] |
| Physical activity | Right prefrontal and cingulate cortex, left prefrontal cortex, cingulate cortex, bilateral occipitotemporal regions, cerebellum, right anterior frontal cortex, middle prefrontal gyrus, anterior cingulate cortex, supplementary motor area [52, 53] |
| Sleep disorders | Left orbitofrontal cortex, bilateral anterior parts of the precuneus parietal cortex, occipito-parietal cortex [54] |
Typical risk factors for the development of CFS are unfavorable environmental and hygienic living conditions, frequent and prolonged stress leading to maladaptation, disruption of the physiological response to stress, monotonous hard work, physical inactivity with excessive poor nutrition, lack of life prospects and a wide range of interests in life.
To diagnose CFS, the criteria of the Center for Disease Control (USA) are used, which include a set of major, minor and objective criteria ( Table 3
) [55, 56]. The diagnosis of CFS is established by the presence of major criteria as well as minor symptomatic criteria: 6 (or more) of 11 symptomatic criteria and 2 (or more) of 3 physical criteria or 8 (or more) of 11 symptomatic criteria.
| Table 3. Criteria for diagnosing CFS | |
| Large criteria | 1) unmotivated fatigue and decreased performance, motor activity (by at least 50%) in previously healthy people during the last four months in adults and three months in children 2) exclusion of other causes or diseases that can cause chronic fatigue |
| Small criteria | - increase in body temperature up to 38 ° C - sore throat, sore throat - slight enlargement (up to 0.3-0.5 cm) and tenderness of the cervical, occipital and axillary lymph nodes - unexplained generalized muscle weakness - myalgia - polyarthralgia - recurrent headaches new, unusual for the patient - rapid physical fatigue followed by prolonged (more than 24 hours) fatigue - sleep disorders (hypo- or hypersomnia) - neuropsychological disorders (photophobia, memory loss and inability to concentrate, increased irritability, depression) - rapid development ( for hours or days) of the entire symptom complex |
| Objective criteria | 1) low-grade fever 2) non-exudative pharyngitis 3) palpable cervical or axillary lymph nodes (up to 2 cm in diameter) |
In the blood serum of 20-25% of patients with CFS, leukocytosis is observed, in approximately the same percentage of cases lymphocytosis occurs, almost half of the patients have monocytosis, and a third of patients have lymphopenia. In 20% of cases, an increase in ESR and/or transaminase activity in the blood serum is observed. When analyzing laboratory data from 579 CFS patients in 4 clinics in the United States, it was not possible to obtain a specific laboratory profile characteristic of this disease [57]. The immunogram was characterized by a chronically low level of activity of the humoral and cellular immunity. A biochemical study of urine in patients with CFS revealed a decrease in the excretion of amino acids, especially aspartic amino acid, phenylalanine, succinic acid with an increase in 3-methylhistidine and tyrosine, which is a reflection of metabolic disorders in muscle tissue that occur in CFS [58].
Possible complications of CFS, which makes the prognosis for this disease quite serious, include depression, severe cognitive impairment, social maladaptation, disability, side effects and reactions due to drug therapy.
Patients with complaints of unexplained fatigue need a detailed and in-depth examination. This is necessary not only to exclude other causative diseases, but also to choose treatment tactics. The diagnosis of CFS can only be made by excluding many other diseases: infectious and parasitic processes, thyroid diseases accompanied by hypofunction, sleep apnea, autoimmune diseases, cancer, hematological diseases, neurological diseases, psychiatric diseases (depression, schizophrenia, alcohol abuse, sleeping pills or drugs), poisoning with heavy metals, industrial poisons, effects of radiation and chemotherapy, metabolic myopathies (enzyme defects, deficiency of vitamin D, B vitamins, iron, etc.), drug myopathies (corticosteroids, anesthetics, clofibrate, allopurinol , chloroquine, D-penicillamine, vincristine, etc.).
If the severity of fatigue or other symptoms do not meet the criteria for CFS, then such fatigue should be classified as idiopathic chronic fatigue. The term “prolonged fatigue” is used in cases where it is observed for 1 month. and more (but less than 6 months), which corresponds to international recommendations ( Table 4
).
| Table 4. Distinctions between different types of fatigue | |
| 0 Unexplained fatigue | Routine assessment of acute physical and psychological illnesses. Control after 1 month. |
| 1 month Long-term fatigue | Detailed assessment of common somatic (for example, hypothyroidism, anemia) and psychological diseases (depression, etc.). Control every month |
| 3 months Chronic fatigue | Detailed diagnosis of fatigue: somatic history and examination, psychological history and examination, laboratory tests. Control every month |
| 6 months Chronic fatigue syndrome | Diagnosis and management of CFS: making a specific diagnosis of CFS, accessing information on CFS, contacting support groups (if available). Monitoring dynamics and treatment monthly |
Treatment of a patient with CFS should be rational and comprehensive. One of the important conditions for treatment is also compliance with the protective regime and constant contact of the patient with the attending physician. The treatment program for chronic fatigue syndrome must necessarily include: normalization of rest and physical activity, fasting and dietary therapy, vitamin therapy with vitamins B1, B6, B12 and C, general or segmental massage together with hydrotherapy and physical therapy, autogenic training or others active methods of normalizing the psycho-emotional background, psychotherapy, general immunocorrectors with an adaptogenic effect, other auxiliary agents (daytime tranquilizers, enterosorbents, nootropic drugs, antihistamines in the presence of allergies).
To date, there is insufficient evidence on the benefits of taking vitamins B12, C, CoQ10, magnesium, or multivitamin or mineral supplements for people with CFS. However, a number of researchers who have identified a deficiency of antioxidants, L-carnitine, B vitamins, and magnesium believe that the addition of drugs containing these nutrients can significantly reduce the symptoms of CFS [59-61].
A universal remedy is multivitamins with macro- and microelements. Of these, Berocca Plus is suitable for the treatment of CFS [62]. The pharmacological effect is determined by the complex of vitamins and minerals that make up the drug. The drug contains 7 B vitamins, vitamin C, calcium and magnesium. One effervescent tablet of the Berocca Plus multivitamin complex contains 500 mg of ascorbic acid (vitamin C), 15 mg of thiamine (vitamin B1), 15 mg of riboflavin (vitamin B2), 23 mg of pantothenic acid (vitamin B5), 10 mg of pyridoxine hydrochloride (vitamin B6), 40 mg folic acid (vitamin B9), 10 mg cyanocobalamin (vitamin B12), 50 mg niacinamide (vitamin B3), 15 mg biotin (vitamin B8), 100 mg calcium, 100 mg magnesium and 10 mg zinc. Vitamin B1 normalizes the activity of the heart and contributes to the normal functioning of the nervous system. Vitamin B2 promotes tissue regeneration processes, including skin cells. Vitamin B6 helps maintain the structure and function of bones, teeth, gums, normal functioning of the nervous system, and affects erythropoiesis. Vitamin C (ascorbic acid) is a biological antioxidant and plays an important role in the inactivation of free radicals, increases the absorption of iron in the small intestine, affects the metabolism of folic acid and the function of leukocytes. Stimulates the formation of connective and bone tissue, normalizes capillary permeability. Calcium is involved in many physiological processes, enzyme systems, and in combination with magnesium and vitamin B6 - in the process of transmitting nerve impulses. Magnesium is involved in various reactions, including protein synthesis, fatty acid metabolism, and sugar oxidation. Zinc as a catalyst activates more than 200 enzymes and is a component of many proteins, hormones, neuropeptides, hormonal receptors, and is also directly involved in the synthesis of coenzymes derived from vitamin B6. The drug is recommended as an adjuvant therapy for severe or chronic diseases accompanied by states of fatigue, irritability, insomnia, prolonged stress, prolonged infectious disease, fever.
In recent years, there has been growing interest in the possible modulatory effects of multivitamins on mood and cognitive performance [63, 64]. In cases of borderline or more severe deficiency, multivitamins have been shown to enhance cognitive function [65]. More recent evidence suggests that such supplements may improve behavioral functioning (i.e., mood and cognition/performance) even in the absence of vitamin deficiency. One study found that taking a multivitamin for 33 days improved mood and attention in men [66, 67]. In the same study, perceived stress levels decreased in the active treatment group, which is consistent with several other studies. For example, taking multivitamin supplements reduced scores on the Depression, Anxiety and Stress (DASS) scale in an eight-week study [68], reduced occupational stress in a 90-day trial [69], and improved negative mood in response to acute laboratory stress factors after nine weeks of supplementation [70].
Convincing data on the role of B vitamins in maintaining and improving cognitive functions was presented by C. McGarel et al. (2015) [71]. In a double-blind, placebo-controlled, randomized, balanced crossover study design, 20 participants (mean age 29 ± 5.54 years) received a multivitamin (Berocca®) and a placebo. Thirty minutes after taking the drugs, they completed a cognitive assessment consisting of a 10-minute battery of cognitive tests, immediately before and after which participants were assessed for mood using a mood rating scale. Five additional participants underwent post-treatment fMRI scans during Rapid Visual Information Processing (RVIP) and Inspection Time (IT) activating tasks. Multivitamin therapy was associated with significantly improved performance on the Sequential Subtraction of Threes test and self-reported personal satisfaction. fMRI showed that both types of multivitamin therapy increased activation in areas associated with short-term memory for attentional processing. It was also the first time that increased brain activation was demonstrated after taking a multivitamin supplement, as measured by fMRI. Thus, A. Scholey et al. convincingly showed that Berocca’s vitamin and mineral complexes objectively have a positive effect on the cognitive functions of individuals, which is confirmed by data from neurocognitive and functional MRI studies [72].
In addition to the vitamin component, Berocca Plus contains minerals such as calcium (Ca), magnesium (Mg) and zinc (Zn), the positive effect of which on cognitive and other neurological functions has been repeatedly described in the literature [73-75].
Berocca Plus is prescribed one effervescent tablet daily, dissolved in a sufficient amount of liquid. The duration of treatment is up to 30 days and is determined individually, on average 7-10 days. Berocca Plus in film-coated tablets - children aged 15 years and older, as well as adults, are prescribed 1 tablet orally (with water). Repeated courses are prescribed at the discretion of the doctor.
For all patients with CFS, mandatory daily walking for 2-3 hours, exercise therapy courses, massage, hydrotherapy and autogenic training are recommended, since the latter, like other active methods of normalizing the psycho-emotional background, based on the pathogenesis of CFS, are the most important pathogenetic elements of therapy in the corresponding category patients.
The prognosis for a patient with chronic fatigue syndrome with a reverse development of symptoms during the first years of the disease (1-2 years) is usually favorable. With a long course of the syndrome, its appearance after 40 years, and signs of depression, the chances of a full recovery decrease.
Thus, taking into account the complexity of diagnosing and treating CFS, prevention and early treatment, the search for effective drugs for this syndrome, and additional clinical studies of the therapeutic capabilities of various drug and non-drug treatment regimens are relevant.
Literature
1. Bombardier CH, Buchwald D. Chronic fatigue, chronic fatigue syndrome, and fibromyalgia. Medical Care, 1996, 34(9): 924–930. 2. Buchwald D, Pearlman T, Umali J, Schmaling K, Katon W. Functional status in patients with chronic fatigue syndrome, other fatiguing illnesses, and healthy individuals. The American Journal of Medicine, 1996, 101(4): 364–370. 3. Steele L, Dobbins JG, Fukuda K et al. The epidemiology of chronic fatigue in San Francisco. The American Journal of Medicine, 1998, 105(3): 83–90. 4. Fukuda K, Dobbins JG, Wilson LJ, Dunn RA, Wilcox K, Smallwood D. An epidemiologic study of fatigue with relevance for the chronic fatigue syndrome. Journal of Psychiatric Research. 1997, 31(1): 19–29. 5. Jason LA, Richman JA, Rademaker AW et al. A community-based study of chronic fatigue syndrome. Archives of Internal Medicine. 1999, 159(18): 2129–2137. 6. Christley Y, Duffy T, Martin CR. A review of the definitional criteria for chronic fatigue syndrome. Journal of Evaluation in Clinical Practice. 2012, 18(1): 25–31. 7. Richman JA, Flaherty JA, Rospenda KM. Chronic fatigue syndrome: have flawed assumptions been derived from treatment-based studies? The American Journal of Public Health. 1994, 84(2): 282–284. 8. Jordan KM, Landis DA, Downey MC, Osterman SL, Thurm AE, Jason LA. Chronic fatigue syndrome in children and adolescents: a review. Journal of Adolescent Health. 1998, 22(1): 4–18. 9. Manian FA Simultaneous measurement of antibodies to Epstein-Barr virus, human herpesvirus 6, herpes simplex virus types 1 and 2, and 14 enteroviruses in chronic fatigue syndrome: is there evidence of activation of a nonspecific polyclonal immune response? Clin Infect Dis. 1994 Sep, 19(3): 448-53. 10. Biswal B, Kunwar P, Natelson BH. Cerebral blood flow is reduced in chronic fatigue syndrome as assessed by arterial spin labeling. Journal of the Neurological Sciences. 2011, 301(1-2): 9–11. 11. Yoshiuchi K, Farkas J, Natelson BH. Patients with chronic fatigue syndrome have reduced absolute cortical blood flow. Clinical Physiology and Functional Imaging. 2006, 26(2): 83–86. 12. Schmaling KB. Single-photon emission computerized tomography and neurocognitive function in patients with chronic fatigue syndrome. Psychosomatic Medicine. 2003, 65(1): 129–136. 13. Lewis DH, Mayberg HS, Fischer ME et al. Monozygotic twins discordant for chronic fatigue syndrome: regional cerebral blood flow SPECT. Radiology. 2001, 219(3): 766–773. 14. Mathew SJ, Mao X, Keegan KA et al. Ventricular cerebrospinal fluid lactate is increased in chronic fatigue syndrome compared with generalized anxiety disorder: an in vivo 3.0 T 1H MRS imaging study. NMR in Biomedicine. 2009, 22(3): 251–258. 15. Jerjes WK, Taylor NF, Wood PJ, Cleare AJ. Enhanced feedback sensitivity to prednisolone in chronic fatigue syndrome. Psychoneuroendocrinology. 2007, 32(2): 192–198. 16. Jerjes WK, Taylor NF, Peters TJ, Wessely S, Cleare AJ. Urinary cortisol and cortisol metabolite excretion in chronic fatigue syndrome. Psychosomatic Medicine. 2006, 68(4): 578–582. 17. Cleare AJ. The HPA axis and the genesis of chronic fatigue syndrome. Trends in Endocrinology & Metabolism. 2004, 15(2): 55–59. 18. Chen R, Moriya J, Yamakawa JI et al. Brain atrophy in a murine model of chronic fatigue syndrome and beneficial effect of Hochu-ekki-to (TJ-41) Neurochemical Research. 2008, 33(9): 1759–1767. 19. Tang SW, Chu E, Hui T, Helmeste D, Law C. Influence of exercise on serum brain-derived neurotrophic factor concentrations in healthy human subjects. Neuroscience Letters. 2008, 431(1): 62–65. 20. Katafuchi T, Kondo T, Take S, Yoshimura M. Brain cytokines and the 5-HT system during poly I:C-induced fatigue. Annals of the New York Academy of Sciences. 2006, 1088: 230–237. 21. Cleare AJ, Messa C, Rabiner EA, Grasby PM. Brain 5-HT1A receptor binding in chronic fatigue syndrome measured using positron emission tomography and [11C]WAY-100635. Biological Psychiatry. 2005, 57(3): 239–246. 22. Yamamoto S, Ouchi Y, Onoe H et al. Reduction of serotonin transporters of patients with chronic fatigue syndrome. NeuroReport. 2004, 15(17): 2571–2574. 23. Rostène W, Kitabgi P, Parsadaniantz SM. Chemokines: a new class of neuromodulator? Nature Reviews Neuroscience. 2007, 8(11): 895–903. 24. Natelson BH, Weaver SA, Tseng CL, Ottenweller JE Spinal fluid abnormalities in patients with chronic fatigue syndrome. Clinical and Diagnostic Laboratory Immunology. 2005, 12(1): 52–55. 25. Buchwald D, Komaroff AL. Review of laboratory findings for patients with chronic fatigue syndrome. Rev Infect Dis. 1991, 13(1): 12-8. 26. Moroz I.N., Podkolzin A.A. New in the diagnosis and treatment of chronic fatigue syndrome. Prevention of aging. 1999, 1: 45-47. 27. Pagani M, Ospedale L. Sacco. Chronic fatigue syndrome: a hypothesis focusing on the autonomic nervous system. Clin. Sci (Colch). 1999, 96(1): 117-125. 28. Altura BM. Basic biochemistry and physiology of magnesium: a brief review. Magnesium & Trace Elements. 1991, 10: 167-171. 29. Manuel y Keenoy B, Moorkens G, Vertommen J, Noe M, Nuve J, De Leeuw I. Magnesium status and parameters of the oxidant-antioxidant balance in patients with chronic fatigue: effects of supplementation with magnesium. J. Am. Coll. Nutr. 2000, 19(3): 374-82. 30. Abraham G, Flechas J. Management of fibromyalgia: Rationale for the use of magnesium and malic acid. J. Nutr. Med. 1992, 3: 49-59. 31. Fulle S, Mecocci P, Fanó G, Vecchiet I, Vecchini A, Racciotti D, Cherubini A, Pizzigallo E, Vecchiet L, Senin U, Beal MF. Specific oxidative alterations in vastus lateralis muscle of patients with the diagnosis of chronic fatigue syndrome. Free Radic Biol Med. 2000, 29(12): 1252-9. 32. Richards RS, Roberts TK, McGregor NR, Dunstan RH, Butt HL. Blood parameters indicative of oxidative stress are associated with symptom expression in chronic fatigue syndrome. Redox Rep. 2000, 5(1): 35-41. 33. Logan AC, Wong C. Chronic fatigue syndrome: oxidative stress and dietary modifications. Altern Med Rev. 200, 6(5): 450-9. 34. Manuel y Keenoy B1, Moorkens G, Vertommen J, De Leeuw I. Antioxidant status and lipoprotein peroxidation in chronic fatigue syndrome. Life Sci. 2001, 68(17): 2037-49. 35. Pall ML, Satterlee JD. Elevated nitric oxide/peroxynitrite mechanism for the common etiology of multiple chemical sensitivity, chronic fatigue syndrome, and posttraumatic stress disorder. Ann NY Acad Sci. 2001 Mar, 933: 323-9. 36. Kuratsune H, Yamaguti K, Takahashi M, Misaki H, Tagawa S, Kitani T. Acylcarnitine deficiency in chronic fatigue syndrome. Clin. Infect. Dis. 1994, 18(1): 62-7. 37. Lange G, Deluca J, Maldjian JA, Lee HJ, Tiersky LA, Natelson BH. Brain MRI abnormalities exist in a subset of patients with chronic fatigue syndrome. Journal of the Neurological Sciences. 1999, 171(1): 3–7. 38. Lange G, Holodny AI, DeLuca J et al. Quantitative assessment of cerebral ventricular volumes in chronic fatigue syndrome. Applied Neuropsychology. 2001, 8(1): 23–30. 39. Cope H, Pernet A, Kendall B, David A. Cognitive functioning and magnetic resonance imaging in chronic fatigue. The British Journal of Psychiatry. 1995, 167: 86–94. 40. Cope H, David AS. Neuroimaging in chronic fatigue syndrome. Journal of Neurology Neurosurgery and Psychiatry. 1996, 60(5): 471–473. 41. Okada T, Tanaka M, Kuratsune H, Watanabe Y, Sadato N. Mechanisms underlying fatigue: a voxel-based morphometric study of chronic fatigue syndrome. BMC Neurology. 2004, 4(1, article 14). 42. Puri BK, Jakeman PM, Agour M et al. Regional gray and white matter volumetric changes in myalgic encephalomyelitis (chronic fatigue syndrome): a voxel-based morphometry 3 T MRI study. The British Journal of Radiology. 2012, 85(1015): e270–e273. 43. de Lange FP, Kalkman JS, Bleijenberg G, Hagoort P, van der Meer JWM, Toni I. Gray matter volume reduction in the chronic fatigue syndrome. NeuroImage. 2005, 26(3): 777–781. 44. de Lange FP, Koers A, Kalkman JS et al. Increase in prefrontal cortical volume following cognitive behavioral therapy in patients with chronic fatigue syndrome. Brain. 2008, 131, part 8: 2172–2180. 45. Barnden LR, Crouch B, Kwiatek R et al. A brain MRI study of chronic fatigue syndrome: evidence of brainstem dysfunction and altered homeostasis. NMR in Biomedicine. 2011, 24(10): 1302–1312. 46. May A. Chronic pain may change the structure of the brain. Pain. 2008, 137(1): 7–15. 47. Gardini S, Cloninger CR, Venneri A. Individual differences in personality traits reflect structural variance in specific brain regions. Brain Research Bulletin. 2009, 79(5): 265–270. 48. Geuze E, Vermetten E, Bremner JD. MR-based in vivo hippocampal volumetrics: 1. Review of methodologies currently employed. Molecular Psychiatry. 2005, 10(2): 147–159. 49. Kitayama N, Vaccarino V, Kutner M, Weiss P, Bremner JD. Magnetic resonance imaging (MRI) measurement of hippocampal volume in posttraumatic stress disorder: a meta-analysis. Journal of Affective Disorders. 2005, 88(1): 79–86. 50. Smith ME. Bilateral hippocampal volume reduction in adults with post-traumatic stress disorder: a meta-analysis of structural MRI studies. Hippocampus. 2005, 15(6): 798–807. 51. Sprengelmeyer R, Steele JD, Mwangi B et al. The insular cortex and the neuroanatomy of major depression. Journal of Affective Disorders. 2011, 133(1-2): 120–127. 52. Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: a meta-analytic study. Psychological Science. 2003, 14(2): 125–130. 53. Colcombe SJ, Erickson KI, Scalf PE et al. Aerobic exercise training increases brain volume in aging humans. Journals of Gerontology A: Biological Sciences and Medical Sciences. 2006, 61(11): 1166–1170. 54. Altena E, Vrenken H, van der Werf YD, van den Heuvel OA, van Someren EJW. Reduced orbitofrontal and parietal gray matter in chronic insomnia: a voxel-based morphometric study. Biological Psychiatry. 2010, 67(2): 182–185. 55. Fukuda K, Straus SE, Hickie I et al. The chronic fatigue syndrome: a comprehensive approach to its definition and study. Ann. Intern. Med. 1994, 121: 953-9. 56. Turnbull N, Shaw EJ, Baker R, Dunsdon S, Costin N, Britton G, Kuntze S. and Norman R. Chronic fatigue syndrome/myalgic encephalomyelitis (or encephalopathy): diagnosis and management of chronic fatigue syndrome/myalgic encephalomyelitis (or encephalopathy) in adults and children. London: Royal College of General Practitioners, 2007. 57. Bates DW, Buchwald D, Lee J et al. Clinical Laboratory Test Findings in Patients with Chronic Fatigue Syndrome. Arch. Intern. Med. 1995, 155: 97-103. 58. Suzanne H. Niblett, Katrina E. King, R. Hugh Dunstan, Phillip Clifton-Bligh, Leigh A. Hoskin, Timothy K. Roberts, Greg R. Fulcher, Neil R. McGregor, Julie C. Dunsmore, Henry L. Butt, Iven Klineberg and T. B. Rothkirch. Hematologic and Urinary Excretion Anomalies in Patients with Chronic Fatigue Syndrome. Experimental Biology and Medicine. 2007, 232: 1041-1049. 59. Jacobson W, Saich T, Borysiewicz LK, Behan WM, Behan PO, Wreghitt TG. Serum folate and chronic fatigue syndrome. Neurology. 1994, 44(11): 2214-5. 60. Vecchiet J, Cipollone F, Falasca K, Mezzetti A, Pizzigallo E, Bucciarelli T, De Laurentis S, Affaitati G, De Cesare D, Giamberardino MA. Relationship between musculoskeletal symptoms and blood markers of oxidative stress in patients with chronic fatigue syndrome. Neurosci Lett. 2003, 335(3): 151-4. 61. Werbach MR. Nutritional strategies for treating chronic fatigue syndrome. Altern. Med. Rev. 2001, 6(1): 4-6. 62. www.berocca.ru. 63. Grima NA, Pase MP, Macpherson H, Pipingas A. The effects of multivitamins on cognitive performance: A systematic review and meta-analysis. J. Alzheimer's Dis. 2012, 29: 561-569. 64. Kennedy DO, Haskell CF. Vitamins and cognition: What is the evidence? Drugs 2011, 71, 1957-1971. 65. Heseker H, Kubler W, Pudel V, Westenhofer J. Interaction of vitamins with mental performance. Bibl. Nutr. Diet 1995, 52, 43-55. 66. Kennedy DO, Veasey R, Watson A, Dodd F, Jones E, Maggini S, Haskell CF. Effects of high-dose B vitamin complex with vitamin C and minerals on subjective mood and performance in healthy males. Psychopharmacology 2010, 211, 55-68. 67. Kennedy DO, Veasey RC, Watson AW, Dodd FL, Jones EK, Tiplady B, Haskell CF. Vitamins and psychological functioning: A mobile phone assessment of the effects of a B vitamin complex, vitamin C and minerals on cognitive performance and subjective mood and energy. Hum. Psychopharmacol. Clin. Exp. 2011, 26, 538-547. 68. Harris E, Kirk J, Rowsell R, Vitetta L, Sali A, Scholey AB, Pipingas A. The effect of multivitamin supplementation on mood and stress in healthy older men. Hum. Psychopharmacol. Clin. Exp. 2011, 26, 560-567. 69. Stough C, Scholey A, Lloyd J, Spong J, Myers S, Downey LA. The effect of 90 day administration of a high dose vitamin B—Complex on work stress. Hum. Psychopharmacol. Clin. Exp. 2011, 26, 470-476. 70. Haskell CF, Robertson B, Jones E, Forster J, Jones R, Wilde A, Maggini S, Kennedy DO. Effects of a multi—Vitamin/mineral supplement on cognitive function and fatigue during extended multi—Tasking. Hum. Psychopharmacol. Clin. 2010, 25, 448-461. 71. McGarel C, Pentieva K, Strain JJ, McNulty H. Emerging roles for folate and related B-vitamins in brain health across the lifecycle. Proc. Nutr. Soc. 2015. 74(1): 46-55. 72. Scholey A, Bauer I, Neale C, Savage K, Camfield D, White D, Maggini S, Pipingas A, Stough C, Hughes M. Acute effects of different multivitamin mineral preparations with and without Guaraná on mood, cognitive performance and functional brain activation. Nutrients. 2013. 5(9). 3589-3604. 73. Studenikin V.M., Kurbaytaeva E.M. Calciopenic conditions and their correction. Attending Physician, 2010, 10: 54-56. 74. Studenikin V.M., Tursunkhuzhaeva S.Sh., Shelkovsky V.I. Zinc in neuropediatrics and neurodietology. Attending doctor. 2012: 44-47. 75. Studenikin V.M., Tursunkhuzhaeva S.Sh., Zvonkova N.G., Pak L.A., Shelkovsky V.I. Magnesium and its preparations in psychoneurology. Effective pharmacotherapy. Neurology and psychiatry. 2012. 4: 8-12, 58-60.
Source:
Medical Council, No. 2, 2015
Besides MRI, how to check the vessels of the head?
To study the veins and arteries of the brain, ultrasound research methods are also used, which are easily tolerated, have no contraindications and do not require special training.
The simplest study - Doppler ultrasound (USDG) shows in which main arteries and veins of the head the blood flow is impaired. The main method of ultrasound diagnosis of a wide variety of cerebral vascular diseases is duplex scanning. It detects blood supply disorders when there are no symptoms yet. Transcranial Doppler ultrasound (TCUSDG or TCDG) additionally evaluates blood flow in large intracranial vessels.
Comparison of images obtained using: ultrasound (left), MRI (center), CT (right)
Ultrasound examination is safe, but does not provide a three-dimensional picture and is significantly inferior to MRI in terms of information content.
Computed tomography (CT) is also used to study blood vessels - this is an X-ray scan. Multislice CT is a more advanced type of examination and is capable of recreating three-dimensional images on a computer screen. The disadvantage of this method is the radiation exposure to the body.
MRI or CT scan of cerebral vessels?
MRI and CT have their advantages in different situations. People who have electronic devices (pacemaker) or objects made of magnetic metals in their body are allowed only CT scanning.
An MRI scan takes tens of minutes and requires you to lie still. A CT scan takes less time, but this procedure uses X-rays. CT scans should not be done too often. The procedure is contraindicated for pregnant women at any stage. MRI is performed as many times as necessary; it is contraindicated only in the 1st trimester of pregnancy.
MRI of cerebral vessels is a safe procedure that will provide a detailed picture of the disease. At the medical office, you can undergo an MRI scan by appointment on any convenient day and time.