Currently, more and more attention is being paid to how immunity affects various processes in our body. Disturbed immune responses discovered in new studies become the missing link in pathogenesis. This stimulates the search for new drugs and other preventive and therapeutic effects. In this text we will discuss the special immune status of the brain - its isolation from systemic immune processes. In addition, let's talk about disorders that violate the immune sovereignty of the central nervous system - autoimmune encephalitis.
Privileged body
The brain is an organ that is remarkable in many ways [1]. The infinite complexity of the device, its functionality and the connection between our lives and its state attract the attention of researchers to the brain. The relationship between the brain and the immune system of our body is also special: the brain is an immune-privileged organ. Immune reactions that easily develop in other tissues (liver cells, muscles, fatty tissue) rarely occur in the brain. Along with the brain, the thyroid gland, testicles and some eye tissues, in particular the cornea, found themselves in such a special relationship with the immune system.
In the minds of doctors in the second half of the twentieth century, the brain was a structure completely isolated from the immune processes of the rest of the body. At the beginning of the last century, Japanese scientists conducted experiments on implanting sarcoma cells (a malignant tumor of muscle tissue) into various organs of mice [2]. It turned out that when sarcoma cells are placed in brain tissue, the tumor actively develops, but when they are implanted under the skin of rodents or into muscle tissue, the tumor does not develop. The researchers suggested that the “center” (the brain) is isolated from the immune processes that successfully fought off the sarcoma “in the periphery” (other tissues). Further research only confirmed this conclusion. The brain, in the minds of scientists, has become a “clean zone” in which an immune response does not develop. In the 1950s, the term “immunological privilege” arose, coined by British scientists named Billingham and Boswell [3].
Overcoming barriers
It has long been believed that the basis of the immune privilege of the brain is the presence of the blood-brain barrier (BBB). The BBB is a complex of cellular and extracellular structures that separate the blood flowing in the capillaries from the neurons of the brain parenchyma. The cells of the vascular walls, the basement membrane on which they lie, and astrocytes participate in the formation of the BBB. The immune privilege of parts of the central nervous system was in good agreement with the extent of the BBB within it. The brain parenchyma is reliably protected by the BBB, and inflammatory processes (encephalitis) rarely occur in it. The choroid plexus, which produces cerebrospinal fluid, and the membranes of the brain do not have such cover, and their inflammation (choroiditis, meningitis) is much more common (Fig. 1).
Figure 1. Structure of the central nervous system. The parts that are well protected by the BBB include the gray and white matter. Other components do not have this protection.
[2]
There are cases in which even the BBB does not save the nervous system, and inflammation processes occur in the brain. However, it is important to answer the question for yourself: do they proceed in the same way as in the rest of the body? Maybe the brain has a special way of immune response, and immune privilege has additional explanations? In vitro, an immune response in tissues can be induced by injecting bacterial lipopolysaccharide (LPS). It is a structural component of the cell wall of gram-negative bacteria that triggers a cascade of immune reactions in our body. When studying the reaction of different body tissues to the introduction of LPS, it turned out that an immune response in the skin and choroid plexuses of the central nervous system occurs to the same dose of LPS [4]. This is logical, because in neither case is there special protection in the form of the BBB. At the same time, to cause an immune reaction in the brain parenchyma similar to that occurring in the skin, a dose 100 times greater than the “skin” dose is required. In this case, compartmentalization of the immune response occurs - predominantly the white matter (the processes of neurons) is affected, and not the gray matter (their bodies). This experience points to another explanation for immune privilege: the weakness of our brain's own, “intrinsic” immune response. The brain parenchyma turns out to be extremely passive in relation to bacterial invasion: the brain does not seem to want to notice foreign components inside itself. Next we will try to figure out what is the reason for this immune “inattention”.
Weak link
If we are talking about the weakness of the local immune response, then we need to figure out what is “broken” in it. This may be impaired recognition with the normal ability of immune cells to attack antigens (weakness of the afferent link). Another option: normal antigen recognition with impaired ability to attack it (weakness of the efferent link). Studies have shown that the efferent part of the brain is preserved and functions normally [2]. Then efforts were focused on searching for disorders in the afferent link. Over time, it became clear that the problem was in recognizing the antigen and further working with it (Fig. 2).
Figure 2. The immune response occurs in several stages. The formation of a reaction to an antigen occurs in two ways: information about the antigen is delivered to local lymph nodes in “liquid” (the antigens themselves) and “solid” form (previously activated cellular elements of the immune system). In an immune reaction outside the brain, both pathways operate. When the brain's immune system reacts to an antigen, cellular elements do not reach the local (cervical) lymph nodes. It is one of the main components of a weak immune response in the brain.
[2]
You can read more about these processes in the article “Immunity: the fight against strangers and... our own” [5].
The brain has difficulty delivering activated immune cells to the cervical lymph nodes. Dendritic cells are responsible for working with antigens in the brain. In other organs, they recognize the antigen and then provide information about it to T and B lymphocytes in the lymph nodes. During inflammation in the brain, this process does not occur: dendritic cells do not migrate to the lymph nodes and do not present antigen. The immune response becomes localized and is regulated by dendritic cells in the brain parenchyma. If in other organs the cellular elements of immunity, after the presentation of the antigen, rush to the site of bacterial penetration [6], then with the development of inflammation in the brain parenchyma this does not happen. The brain has to rely on itself. A similar locality of the immune response is observed in the parenchyma, but not in the choroid plexuses and meninges.
Immigrants in the brain
If we continue to describe the special immune status of the brain in our body, then it is necessary to say a few words about microglia. Microglia are the main cell type responsible for the innate immune response in the brain (Fig. 3) [7]. Microglia have phagocytic activity, are able to recognize microorganisms and contribute to the development of inflammatory reactions in the brain parenchyma, that is, they behave not like a neuron, but a real immune cell [8]. This is explained by the fact that microglia in our brain are of hematopoietic origin [9]. The precursors of microglia in the prenatal period are the “brothers” of all other immune cells that find themselves in the central nervous system. They did not lose their immune functions and began to carry them out locally. It turns out that microglial cells can be called emigrants of the immune system.
6.2. Necrosis of the femoral head associated with smoking
According to statistics, today approximately 4 million people die annually from diseases caused by smoking. More than 30% of patients with ANFH are smokers, and many of them have poor health. By 2021, the number of people killed by smoking will exceed the number of people killed by any other disease, including AIDS. Smoking will become the most important epidemic disease in the 21st century.
When tobacco burns, it releases more than 4,000 toxic substances, of which, as is now known, more than 40 are carcinogenic. Smoking is the main cause of cardiovascular and cerebrovascular diseases. The incidence of lung cancer in smokers is 20 times higher than in non-smokers. One of the research centers in the USA, working on this problem for 35 years, confirmed that there is a clear connection between smoking and cancer: for those who smoke more than 1 cigarette per day, the risk of cancer immediately increases by 2 times , and for those who smoke more than one pack of cigarettes, the risk of getting cancer increases 20 times. Smokers easily get stomach and duodenal ulcers, as well as neurasthenia.
Active and passive smokers - patients with necrosis of the femoral head - poison themselves with nicotine and lead, which accumulate in the body and impair blood circulation, destroy the bone structure and aggravate necrosis of the femoral head. After smoking, nicotine quickly enters the bloodstream and irritates the sympathetic nerve and chromaffin cells, stimulates the production of active factors by the adrenal glands, causing an increase in angiotensin and vasoactive elements in the blood plasma. In different tissues, the quantitative distribution of α- and β-receptors is different, which contributes to the contraction of peripheral blood vessels in tissues and dilation of central vessels, spasm of arterioles, increased vascular resistance, impaired venous outflow, increased blood viscosity, preventing microcirculation in the head of the femur, as a result bone tissue stops receiving nutrition and the destruction of the bone structure of the femoral head accelerates.
Thus, smoking patients aggravate the course of ANFH, slowing down the recovery of health. The harm caused by smokers to society What is even more dangerous is that the smoke exhaled by smokers causes even more harm to others than to the smokers themselves. Research conducted by scientists has confirmed that in Shanghai, 37.8% of school-age children have blood lead levels above the permissible level. For every 100 mg increase in the level of lead in the blood of children, the mental development index decreases by 6-8 points, and the main cause of lead poisoning in children is second-hand smoke created by parents at home. In this regard, to preserve the health of children and other people, it is necessary to create a smoke-free environment in society.
Actively and passively smoking women, in addition to harming themselves, they also destroy their offspring, since smoking has a bad effect on the psychosomatic development of the fetus and causes serious damage to the intellectual abilities of children. If a nursing mother has nicotine in her milk, this has a negative effect on the baby's health. The authors hope that every patient with ANFH will show high social consciousness: will stay away from cigarettes and value the health of their loved ones and other people.
Autoimmune encephalitis
After talking about the special immune status of the brain, we will move on to the topic of autoimmune encephalitis - a group of diseases that are associated with damage to the membrane and intracellular structures of neurons by the body’s own immunity. In modern practice, autoimmune encephalitis is rarely diagnosed. This is explained by the fact that the first cases were described in detail only in 2005 [10]. It can be assumed that there are actually more cases of this disease than are recorded by specialists. Some patients with autoimmune encephalitis may be diagnosed with other disorders, such as schizophrenia or infectious encephalitis. This is due to the fact that doctors have little knowledge about this disease. Doctors diagnose only those diseases that they know. The more arsenal of diagnoses a doctor has in stock, the more accurate the diagnosis and the more correct the treatment.
Autoimmune encephalitis can be divided into two groups:
- diseases caused by activated T cells (something similar occurs in multiple sclerosis [11]);
- diseases that occur when antibodies act on intra- and extracellular components of a neuron, such as ion channels.
The first group of autoimmune encephalitis is characterized by cell damage by antibodies and activated T lymphocytes [12]. These encephalitis are more severe and require intensive therapeutic interventions, unlike representatives of the second group.
In the second group of encephalitis, neuronal damage is only “superficial” in nature. The effect of specific antibodies on surface-located structures leads to the “contraction” of receptors (in English this is called capping) and their subsequent internalization (capture) into the cytoplasm (Fig. 3) [13]. In addition, autoantibodies themselves can bind to receptors, blocking their work [14].
Figure 3. The changes that occur in receptors in autoimmune encephalitis are similar to the changes in synapses in myasthenia gravis. Normally (left side of the figure), the receptors are free and easily interact with the neurotransmitter acetylcholine. In case of illness, antibodies begin to affect the receptors, and their ability to bind to the neurotransmitter is impaired. The “clumped” acetylcholine receptors are gradually drawn into the cytoplasm, where they are destroyed.
www.memorangapp.com
Antibodies penetrate from the outside, from outside the BBB, or are produced by brain-infiltrated and activated B-lymphocytes [15]. In cases where antibodies are directed against intracellular structures, the attack on neurons is led by cytotoxic T lymphocytes. With the help of perforin and granzyme B, they damage the membrane of neurons, which leads to their death [16], [17]. The GEB, which we talked about above, in this light appears to be a reliable fortress wall protecting a quiet city that is no longer used to fighting. If a gap appears in the wall, the city will quickly fall: the nerve cells will be too sensitive to the effects of immune factors.
Looking for flags
Signs of autoimmune encephalitis are very varied, but three types of symptoms can be distinguished.
- Psychiatric symptoms: psychosis, aggressive actions, sexual disinhibition, panic attacks, obsessive actions, feelings of euphoria or fear.
- Motor symptoms: increased muscle tone and unevenness, muscle twitching and repetitive movements of the limbs.
- Seizures: generalized epileptic seizures, status epilepticus.
The initial manifestations of autoimmune encephalitis may be symptoms of a mental disorder: memory impairment, hallucinations or the appearance of delusional ideas. For example, with autoimmune damage to glutamate NMDA receptors, 80% of patients showed symptoms of mental illness, and more than 60% were initially hospitalized in psychiatric departments [18], [19]. Psychiatrists must be able to identify patients with autoimmune encephalitis or at least suspect this disease in order to promptly send the patient for appropriate examinations and consultations with other doctors.
Among the variety of symptoms that can be caused by different reasons, it is easy to get lost. The doctor needs at least rough guidelines to suspect the diagnosis of autoimmune encephalitis. As a result of the analysis of many cases of the disease, signs were identified that most likely indicate this diagnosis - the so-called “red flags” of autoimmune encephalitis [20]. These include:
- Lymphocytic pleocytosis or the appearance of oligoclonal bands on CSF electrophoresis.
- Epileptic seizures.
- Faciobrachial dystonic seizures.
- Suspicion of neuroleptic malignant syndrome.
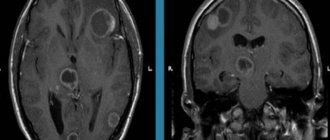
- Abnormalities on MRI.
- EEG abnormalities.
In addition, the researchers also identified “yellow flags” - signs that should alert the doctor and make him think about a possible diagnosis of autoimmune encephalitis [20]. Yellow flags for autoimmune encephalitis are:
- Reduced level of consciousness.
- Violation of posture and movements.
- Instability of the autonomic nervous system.
- Focal neurological symptoms.
- Speech disorders (aphasia and dysarthria).
- Rapid progression of psychosis, despite treatment.
- Hyponatremia.
- Catatonia.
- Headache.
- The presence of other autoimmune diseases, including thyroiditis.
If a doctor sees symptoms from the group of “red flags” in a patient, the study authors recommend testing for specific autoantibodies for the timely diagnosis of autoimmune encephalitis. If a patient has symptoms from the list of “yellow flags,” the doctor should suspect the possibility of such a diagnosis and examine the patient more carefully to look for more reliable signs of autoimmune encephalitis.
Additional Arguments
In addition to the combination of previously described symptoms, the diagnosis of autoimmune encephalitis must be confirmed by laboratory tests and other diagnostic procedures [21].
For example, you can test for antibodies to specific receptors. In autoimmune encephalitis that affects glutamate NMDA receptors, an increase in the titer of antibodies to them can be detected. Interestingly, in encephalitis the amount of immunoglobulins of class G increases, and in schizophrenia - classes A and M [22]. Currently, a correspondence has been established between antibodies that affect specific neuron structures and the symptoms of encephalitis (Table 1). Magnetic resonance imaging (MRI) may show changes in brain structure, and electroencephalography (EEG) may show abnormal brain function in the case of autoimmune encephalitis. Table 1. Correspondence of symptoms and autoantibodies in autoimmune encephalitis [20]
| Structure to which an antibody is produced | Psychiatric symptoms | Other symptoms | Typical patient |
| NMDA receptor | Psychosis, schizophrenia-like disorders, catatonia, aggression | Epileptic seizures, dyskinesia, autonomic instability, speech and consciousness disorders | Young women, common association with ovarian teratoma |
| Caspr2 | Insomnia, panic attacks, depression, schizophrenia-like disorders | Morvan's syndrome, neuromyotonia, muscle spasms, fasciculations | Middle-aged and older patients, possible connection with thymoma |
| LGI1 | Amnesia and other memory impairments, confusion, depression | Limbic encephalitis, faciobrachial dystonic seizures, hyponatremia | Middle-aged and older patients, male to female ratio 2:1, possible association with thymoma |
| Glycine receptor | Behavioral changes, schizophrenia-like syndrome | Tight muscle syndrome, progressive encephalomyelitis with rigidity, myoclonus, hyperekplexia | Middle-aged and older patients, possible association with thymoma and lymphoma |
| Synaptic antigens (GAD) | Schizophrenia-like syndrome, autism, attention deficit hyperactivity disorder | Limbic encephalitis, stiff muscle syndrome, seizures, brainstem dysfunction, ataxia | Middle-aged and older patients, possible association with small cell lung cancer |
| Onconeural antigens (Yo, Hu, CV2, Ri, Ma2) | Behavioral disorders | Limbic encephalitis, cerebellar degeneration, sensory neuropathy | Elderly patients, often with malignant tumors |
In some cases, autoimmune damage to the central nervous system is caused by the development of paraneoplastic syndrome, which may accompany the appearance of a malignant tumor in the body. In paraneoplastic syndrome, the tumor can begin to independently produce hormones and hormone-like substances, disrupting the regulation of various processes in the body. In addition, paraneoplastic syndrome can manifest itself in the form of an autoimmune disease, for example, autoimmune encephalitis.
The pathogenesis of autoimmune encephalitis within the paraneoplastic syndrome is as follows. In a malignant tumor of a certain tissue, genes that are typical for it are expressed, as well as genes that are usually “silent” in it. Among the “silent” genes there may be those that are normally expressed only in the brain, under the protection of the BBB. Therefore, the resulting proteins are called cancer-neuronal antigens. During the maturation of the immune system, it becomes familiar with almost all the proteins of the body, but these proteins are hidden from it and, accordingly, are perceived as foreign. From the point of view of our immunity, there is no difference between them and bacterial antigens. The tumor begins to produce cancer-neuronal antigens, and the immune system recognizes them and produces autoantibodies specific to them. Through minimal gaps in the BBB, autoantibodies penetrate the central nervous system and begin to attack neurons [14].
For this reason, when diagnosing autoimmune encephalitis, special attention is paid to searching for a tumor in the patient’s body. Removal of the tumor in cases of paraneoplastic origin of autoimmune encephalitis will lead to a significant improvement in the patient's condition. While the tumor is in the human body, antibodies continue to be produced, and the patient’s condition worsens.
A blow to the immune system
Steroids and immunoglobulins administered intravenously are used as first-line drugs for the treatment of autoimmune encephalitis. Steroids have a powerful anti-inflammatory effect. They are capable of suppressing immune responses at a variety of levels. The use of steroids leads to a decrease in the synthesis of inflammatory mediators and stabilization of lysosome membranes that secrete inflammatory factors. In addition, under the influence of steroid hormones, the migration of monocytes decreases. Plasmapheresis, which cleanses the blood of “extra” antibodies, can also help.
If first-line therapy does not work, then switch to the use of rituximab and cyclophosphamide. Rituximab is a monoclonal antibody against the CD20 receptor, which is found on the surface of B lymphocytes [23]. B lymphocytes produce a variety of antibodies, including autoantibodies against nerve cells, and their destruction can lead to improvement. The CD20 receptor appears on the surface of normal B-lymphocytes and B-lymphocytes that have undergone the process of malignancy (malignancy). Due to this property, rituximab is effective in autoimmune diseases and B-cell lymphomas. The drug binds to the CD20 receptor on the surface of the lymphocyte and enables other components of the immune system to destroy the cell.
Cyclophosphamide has an immunosuppressive effect and is able to suppress the body's excessive immune response. After passing through the liver, cyclophosphamide is converted into several active metabolites that penetrate the cell and tightly connect the two strands of DNA. This prevents tumor cells or other rapidly dividing cells (such as B and T lymphocytes) from dividing. For this reason, cyclophosphamide is included in the treatment regimen for some autoimmune diseases. The subtlety of using steroids, cyclophosphamide and rituximab for autoimmune encephalitis is that these drugs can complicate the diagnosis of those tumors that are associated with the appearance of autoantibodies. In case of lymphoma, the use of these drugs can temporarily improve the condition, but when discontinued, the tumor will again “take up the old ways” and produce autoantibodies. Although lymphoma is not so often complicated by autoimmune encephalitis, this feature must be taken into account during therapy.
Using autoimmune encephalitis as an example, we can consider two of the most important trends in modern medicine. The first trend is the study of the influence of immune processes on the functioning of the human nervous system and attempts to intervene in this process in the treatment of neurological and mental diseases. We are now close to understanding that the brain is not just an electrochemical laboratory under the skull, but also a special immune world with its own rules. It is in our interests to learn these rules and begin to play by them to our advantage. The second trend is the biologization of psychiatry, the search for specific biological changes in the body that lead to mental health problems. Psychiatry is a part of medicine, a large branch where theoretical knowledge and its practical application are combined. Without a biological basis, medicine will cease to be scientific. If you ignore biological laws and knowledge within one of the medical specialties, then the same thing will happen to it. Psychiatry must become biological in order to remain scientific and fulfill its medical goals.
New Horizons
Recently, researchers and doctors have been paying more and more attention to innate immune responses during the development of neurodegenerative diseases (Alzheimer’s disease [24], Parkinson’s disease [25], Huntington’s chorea [26]) and mental disorders [27]. The accumulation of beta-amyloid, which itself is most likely involved in the immune responses of the central nervous system [28], is associated with an imbalance between its accumulation and elimination (removal). The latter process depends in part on how toll-like receptor 2 (TLR2) is expressed [29]. Mouse models have shown that the lower the level of TLR2 expression, the worse the removal of beta-amyloid [30]. Decreased elimination of beta-amyloid leads to its accumulation in nerve cells and subsequent disruption of their function and death. Studying the internal immune processes of the brain can become the basis for the search for new drugs for neurodegenerative diseases. Pharmaceutical companies are now testing monoclonal antibodies to treat Alzheimer's disease, but success remains modest.
Treatment of necrosis
The disease in question can be successfully treated, but only if it is carried out in a medical institution and under constant monitoring by doctors. General principles of therapy:
- Necrosis of the teeth, jaw or gums is diagnosed quite quickly, because it is accompanied by severe pain and an extremely unpleasant odor from the oral cavity. Patients, as a rule, immediately seek medical help and therefore treatment consists of prescribing medications - antibacterial drugs, disinfectants. In some cases, dentists have to surgically remove already necrotic areas of soft tissue.
- Necrosis of tissues of internal organs is often diagnosed already in the extreme stages. For example, the symptoms of pancreatic necrosis are often blurred. Even when visiting a doctor, the patient is often given an incorrect diagnosis, which can lead to the death of a large number of cells in the internal organ. Typically, pancreatic necrosis is treated surgically, but the prognosis in this case can be very different - from favorable (full recovery) to imminent death.
- Bone death almost always requires surgery. Surgery for necrosis of the hip joint, for example, involves removing the problem area and using an endoprosthesis. With timely diagnosis, such treatment always has a favorable prognosis.
- The stages of liver necrosis are the main factor in choosing the method of its treatment. If at the initial stage drug therapy is quite acceptable, then at the moderate and severe stages only surgery is considered.
Consultation on how intestinal necrosis is treated and what the first symptoms of the pathology are can only be obtained from a qualified doctor. You can make an appointment on our website Dobrobut.com.
6.8. Neurotrophic diseases of bones and joints
Neurotrophic diseases of bones and joints are also called Charcot's joint (neurogenic arthropathy). Neutrophic Charcot arthropathy is a kind of degenerative-dystrophic damage to joints caused by a violation of their innervation. This disease can be caused by the following reasons: • spinal cord lesions due to syringomyelia, tertiary syphilis (neurolues), B12 deficiency anemia (funicular myelosis), myelomeningocele, cauda equina tumors; • pathology of peripheral nerves in decompensated insulin-dependent diabetes mellitus, chronic alcoholism, vitamin B1 deficiency (beriberi), leprosy, familial amyloid neuropathy.
Charcot arthropathy is based on disturbances in the trophism and sensitivity of denervated articular tissues. Weakening of the trophically altered tendon-ligamentous apparatus leads to joint instability, which, in conditions of decreased deep (proprioceptive) and pain sensitivity, contributes to their increased trauma. Moreover, due to trophic disorders in bone tissue, even the usual load on the joints becomes excessive. Under the influence of these factors, pronounced destructive changes occur in the joints, in particular the development of osteolytic processes in the epiphyses with their fragmentation and the formation of intra-articular osteochondral sequestration. X-rays of the hip joint in this disease indicate the presence of osteoporosis and destruction of the bone structure, resorption of the femoral head, and in severe cases, resorption and disappearance of the head and neck of the femur. There is only a small amount of osteochondral formations (bone remains) in the joint, the damaged end of the femoral neck is dislocated upward, the acetabulum and the remains of the femoral neck look unclear, and bone density is reduced. In some images, the head of the femur is flat and the neck is shortened, bone density is increased, there are scattered sac-like light-transmitting zones and peripheral sclerosis between the head of the femur and the trochanter. The edges of the acetabulum are thickened and ossified, the distance between the head of the femur and the bottom of the acetabulum is widened, the head of the femur is shifted outward, the articular space is noticeably narrowed, under the greater trochanter there is a wide proliferation of periosteum in the form of onion peel, in the cartilage tissues at the upper end of the tibia there is a long band of calcification (fascia lata calcification), and in the lower part of the ischial tuberosity there is calcification in the form of a strip or circle.
Differential characteristics of Charcot's joint.
Charcot's joint differs from osteoarthropathy mainly in that it is manifested by the presence of osteoporosis, joint destruction, the presence of bone debris within the joint and its deformation. At the same time, the main thing is not so much osteoporosis, but the presence simultaneously with it of serious destruction of the joint, which is completely inconsistent with the patient’s subjective symptoms in the form of mild pain.
The severity of osteoporosis in osteoarthropathy is less than in Charcot's joint, and its main symptoms are joint pain and impaired movement.
6.5. Congenital varus position of the femoral neck
Congenital varus position of the femoral neck is also called varus position of the femoral neck due to developmental delay. In this case, the gait resembles the walking of a person with a congenital dislocation of the hip. The x-ray shows that the characteristic signs of this disease are: a decrease in the neck-shaft angle, a lack of calcium in the lower part of the femoral neck and the formation of a triangular bone.
The mechanism and causes of this disease are unclear. They are thought to be associated with congenital abnormal development of the epiphyseal plate and interference with the calcification process within the femoral neck.
Varieties
Given the changes that occur in the tissue, there are some forms of necrosis. Namely:
- The cause of coagulation or dry necrosis is the folding, compaction, drying of tissue protein, which then becomes a curdled mass. This is the result of the fact that blood has stopped flowing and moisture has evaporated. Areas of tissue become dry, brittle, and also acquire a dark brown or yellowish gray tint with clear demarcation lines. In the place where the dead tissue was rejected, ulcers will appear, a purulent process will develop, and an abscess will form. The localization of dry necrosis is the spleen, kidneys, and umbilical cord stump in a newborn child.
- With colliculative or wet necrosis, swelling, softening and liquefaction of dead tissue occurs, and a mass with a gray tint is formed and a putrid odor appears.
There are some types of necrosis
1. If the blood supply to a tissue or organ suddenly stops, a heart attack occurs. The term ischemic necrosis refers to the death of any part of a vital organ (brain, heart, intestines, lungs, kidneys, spleen). If the infarction is small, autolytic melting or resorption is observed, followed by tissue restoration. A heart attack can result in impaired tissue functioning, various complications, and even death.
2. If necrosis of a section of bone tissue occurs, the localization of which is the sequestral cavity, this is called sequestration. In such a situation, this area will separate from healthy tissue. The reason for this is a purulent process.
3. Death of the skin, mucous surface, and muscle tissue is called gangrene. The cause of gangrene is tissue necrosis.
4. The presence of bedsores is observed in a person who is completely immobilized. This is explained by prolonged compression of the tissue and damage to the skin. As a result, deep purulent ulcers form.