Main symptoms of the disease:
- headache,
- insomnia,
- mental disorders,
- noise in ears,
- loss of consciousness,
- lack of coordination
- convulsions,
- loss of skin sensitivity,
- nausea,
- vomit.
The causes of cysts include bruises and hematomas, congenital disorders, parasitic infections, meningitis, dystrophic transformations, problems with blood circulation in the brain. It is impossible to perform an operation to remove a brain cyst without finding out the true cause of the disease. Even the slightest mistake in making a diagnosis will lead to further inflammation of the meninges and the emergence of new lesions.
Small cysts that are not accompanied by any symptoms are most often discovered during the diagnosis of other diseases. In some cases, they do not require surgical intervention, especially if they do not increase in size over a long period of time. It is enough to monitor your blood pressure, avoid hypothermia, avoid viral infections, and do not abuse smoking and alcoholic beverages.
Drug treatment
There is no need for therapy if the tumor is small in size and does not cause discomfort to the patient.
It is enough to simply undergo periodic preventive examinations. But if the cyst begins to grow, then at first it is necessary to carry out drug treatment. According to ICD-10, the disease is coded G93. The patient is prescribed drugs that promote the resorption of adhesions. Tablets or injections are used to lower cholesterol levels.
Natalya Schneider, neurologist, Doctor of Medical Sciences, talks about the use of nootropic drugs:
In order for the functionality of brain cells to be maintained at the required level, they need to be supplied with glucose and oxygen. To do this, the patient uses nootropic substances: Nistenon, Picamilon. Naturally, it is also desirable to protect cells from the negative effects of changes in intracranial pressure. In this case, the patient is prescribed antioxidants.
During treatment, immunomodulators, anti-inflammatory, and antibacterial agents will be needed. Typically, patients are treated with tablets for 10-12 weeks. The treatment course is repeated after about six months. Therapy is prescribed only by a doctor. He also decides on the advisability of its extension. You can also use folk remedies, but it is also necessary to coordinate their use.
Treatment of spinal cyst
Treatment of spinal cysts has certain difficulties and is aimed at alleviating the condition and preventing the risk of developing serious complications. Treatment of spinal cysts can be either conservative or surgical. Conservative treatment is possible for small cysts, in the absence of severe pain and without disruption of the function of internal organs.
Conservative treatment of spinal cysts includes:
- Bed rest.
- A balanced diet with sufficient amounts of vitamins, proteins, micro- and macroelements.
Drug treatment
- Prescription of analgesics and anti-inflammatory drugs.
- Prescription of B vitamins (improves metabolic processes in the cell) and vitamin C (strengthens blood vessels and improves immunity).
- The use of drugs to improve microcirculation
- The use of drugs that reduce degenerative-dystrophic processes in osteochondral tissue (chondroprotectors).
Blockades
. Perhaps the purpose of a therapeutic blockade is the introduction of anesthetics (novocaine, lidocaine) to the place where the pain is most pronounced, the so-called trigger points, or the introduction of an anesthetic into the epidural space (epidural blockade). A blockade with the combined use of an anesthetic and a corticosteroid drug (Cortizone, Diprospan) is possible.
Mysterious pineal gland with a cyst in it
A special type of cystic formation in the brain is considered to be a pineal gland cyst, which is better known to us as the pineal gland. What mission is assigned to the pineal gland in the human body is still not exactly clear. Scientists say that she:
- Produces melatonin, which is involved in the regulation of circadian (daily) biorhythms, so that a person does not get confused with sleep and wakefulness;
- Contributes to the process of puberty;
- Affects the growth of tumors (in some places it accelerates, in others it slows down).
Diagnosing a cyst of this small gland has become possible thanks to the advent of modern neuroimaging methods (for example, MRI). Previously, it was considered a rather rare pathology and accounted for only 1.5% of all brain diseases. Now many authors note that it was simply not found due to its asymptomatic course. Even now, not everyone does MRI every day, so in many cases, a pineal gland cyst is registered as an accidental finding, and in those who do not complain and are not specifically examined, it is considered that it does not exist at all.
A benign cystic formation of the pineal gland, located in one of the lobes of this mysterious organ, as a rule, does not cause much harm to it, does not affect functional abilities and is usually not prone to rapid growth. An epiphysis cyst, like other formations of a similar kind, as a rule, does not give specific signs, and if symptoms appear, they can easily be attributed to other brain diseases:
- A headache that occurs without a reason and has no system; the patient never knows when he will have a headache;
- An attack of cephalgia can be so strong that it causes nausea and then vomiting;
- There may be a lack of coordination of movements, which noticeably affects the patient’s gait;
- The reaction of the organs of vision to attacks is especially significant: it hurts to roll your eyes up, blurred pictures, double vision and fog make it difficult to see surrounding objects.
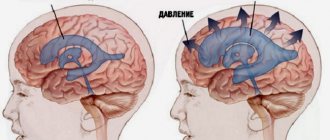
In rare cases, a cyst can also “show its character.” This happens when it grows rapidly and, reaching a critical size, begins to put pressure on neighboring areas of the brain, blocking the movement of cerebrospinal fluid and manifesting symptoms of hydrocephalus with the ensuing consequences.
Why did the cystic formation begin its journey in the pineal gland? Today there are two main reasons for its appearance there:
- For various reasons, the excretory canal closes and blocks the movement of the secretion of the gland, which remains and forms a place for itself;
- With the blood flow, a parasite, echinococcus, enters the pineal gland, which “settles in and settles in” in a new place, forming a capsule that protects itself from attacks by the immune system. The parasite releases the products of its vital activity within its “home,” thereby expanding its domain.
“House” for parasite larvae
Life cycle of Echinococcus. The parasite infects the brain, liver, lungs and other human organs
Echinococcus is a representative of helminths, the larvae of which, having entered the human body, which is the intermediate host, settle in it, forming cysts in various organs. The latter are more often localized somewhere in the liver or lungs, causing discomfort primarily to these areas, but sometimes they reach the brain through the bloodstream and settle in it. Often an attractive place for the parasite is the pineal gland, where it waits out the larval stage and forms cysts for this. True, once in the human body, which is a dead-end branch for the parasite, the helminth stops its development due to the impossibility of relocating to a permanent host.
A pineal cyst formed by echinococcus gives more vivid symptoms; mental disorders (depression, delirium, dementia) and convulsive seizures are added to the clinical manifestations that make one suspect a cyst.
Echinococcal cystic formations are diagnosed using the same methods as other brain cysts (CT, MRI, biopsy, if questions remain), however, a complete blood count can be useful here, which shows a noticeable increase in eosinophils (eosinophilia) and ESR.
Removal of a cyst, whether echinococcal or another nature, is carried out surgically, if the need arises:
- Hydrocephalus develops;
- Other brain structures and vascular beds suffer.
If the cyst behaves calmly, does not show a tendency to grow, does not give symptoms, the patient is monitored, which consists of an annual MRI and a visit to a neurologist.
Course of the disease
A benign cavity filled with cerebrospinal fluid does not manifest itself in any way if it is in a latent, dormant state. As soon as provoking causes arise that trigger the process of division and growth, the tumor begins to put pressure on areas of the brain and the person experiences discomfort. The clinical course of the disease is increasing. The stages of development are given below:
- Clinical compensation is the stage of a “dormant” cyst: the tumor is localized in the skull, but does not manifest itself.
- Subclinical compensation – the first disturbances of neural functions appear.
- Partial clinical decompensation – neurological disorders become permanent.
- Severe clinical decompensation - the cyst changes location, gradually blocking the large hole at the back of the brain. The patient experiences a disruption in the functioning of organs and systems.
- Impaired cardiovascular activity leading to death.
Types of brain cysts
K»Ã°ÃÂÃÂøÃÂøúðÃÂøàðÃÂðÃÂýþøôðûÃÂýààúøÃÂà÷ðòøÃÂøÃÂ:
- Ã] ²²Pa · ãâtely · ãâte ¸.
- ÃÂàÃÂÃÂúÃÂÃÂÂÃÂ: ÿÃÂþÃÂÃÂþù (ø÷ úûõÃÂà¾Ãº ðÃÂðÃÂýþøôðûÃÂýþù þñþûþÃÂÃºà ¸) øûø ÃÂûþöýþù (ÃÂüõÃÂø ð ÃÂðÃÂýþøôðûÃÂýÃÂàúûõþú ø ôÃÂÃÂà ³Ã¸Ã ÃÂúðýõù).
- ÃÂàÃÂÃÂõÿõýø ÃÂð÷òøÃÂøÃÂ: ÿþûþÃÂÃÂà ¸, ÃÂòõûøÃÂøòðÃÂÃÂøõÃÂàò ÃÂð÷üõÃÂð àøûø ÿÃÂõúÃÂà°ÃÂøòÃÂøõ ÃÂþÃÂÃÂ.
From the editor: Treatment of stroke and rehabilitation after it
ÃÂÃÂòðõàø ÿþ üõÃÂÃÂàþñÃÂð÷þòðý øÃÂ: ðÃÂðÃÂýþøôðûÃÂýðà(ýð ÿþòõàÃÂýþÃÂÃÂø üþ÷óð), ÃÂõÃÂÃÂþÃÂõà»ÃµÃ±ÃµÃ»Ã»ÃÂÃÂýðà(ò óûÃÂñøýõ ÃÂõÃÂþà³Ã¾ üþ÷óþòþóþ òõÃÂõÃÂÃÂòð).
ÃÂõÃÂÃÂþÿþûþöõýøõ úøÃÂàò óþû þòýþü üþ÷óõ:
- ÷ðôýÃÂàÃÂõÃÂõÿýðàÃÂüúð;
- ÿÃÂðòðàòøÃÂþÃÂýðàôþûÃÂ;
- ûõòðàòøÃÂþÃÂýðàôþûÃÂ;
- ÃÂõûàüõöôàÿþûÃÂÃÂðÃÂøÃÂüø;
- ûþñýðàÃÂðÃÂÃÂÃÂ;
- ÃÂõüõýýðàÃÂðÃÂÃÂÃÂ;
- üþ÷öõÃÂþú;
- ÃÂøÃÂúþòøôýðàöõûõ÷ð.
ÃÂÃÂðÃÂýþøôðûÃÂýðàúøÃÂÃÂð üþöõà A ÷óþòþü úðýðûõ, ýð úþýÃÂõ ýõà VALUE The úÃÂõÃÂÃÂÃÂð.
How can traditional medicine help?
The task of folk remedies is the same as traditional ones - to improve blood circulation, metabolism, and eliminate symptoms. Properly selected recipes will help cope with annoying headaches and can even slow down the growth of the cavity.
In folk medicine it is common to use:
- Hemlock. The crushed seeds of the plant can be infused in half a liter of olive oil. You need to mix and leave the product for three weeks in a cool place. It is recommended to instill this oil solution 2 drops into the nose 2-3 times a day.
- Dioscoreim Caucasian (root). 4 parts of the root need to be crushed and poured with vodka (1400 ml). The infusion is poured in stages. First, take half the roots and pour 700 ml of vodka in a glass container. You need to leave it for 5 days. Then you need to drain all the liquid and pour a fresh portion of vodka (700 ml) over the roots. Leave again for 5 days. The infusion should be taken one teaspoon three times a day.
- Decoctions of raspberries, licorice, wormwood, elecampane, chamomile, and calendula will help reduce intracranial pressure.
For some reason, many people believe that folk remedies are safe. This is wrong. To avoid unpleasant consequences, you should definitely ask your doctor whether you can use them specifically. It is the doctor who must select the folk remedy. Otherwise, it may not only not help, but also seriously harm. In addition, some medications are incompatible with herbs or alcohol.
Pathogenesis
As the colloid cyst grows, its circulation channels close, and it cannot pass from the third to the fourth ventricle. Fluid accumulates and intracranial pressure increases. If the growth of the cystic formation does not go towards the connection of the canals, then the increase in intracranial pressure occurs gradually, and the symptoms of the disease manifest themselves for a long time (up to 10 years). With the rapid growth of a neoplasm in the area of the anatomical openings of the cerebrospinal fluid circulation or with a sudden shift of the cyst, symptoms of acute blockage of the cerebrospinal fluid ducts develop. With an increase in the size of the latter, pressure occurs on the cerebral vault and the nuclei of the hypothalamus, this leads to disruption of the process of remembering recent events (short-term memory), disruption of the regulation of body temperature, sleep and wakefulness, complete loss of the feeling of hunger (anorexia) or, conversely, satiety ( bulimia), changes in the emotional sphere.
When is a consultation with a neurosurgeon necessary?
Newborns today are almost universally examined using neurosonography (ultrasound examination of the brain). During this test, infants often have some type of cyst. If the cyst is large, specialists will likely recommend an MRI. If not, they will watch. A rapidly enlarging cyst, or a cyst causing epileptic seizures or other neurological symptoms, requires consultation with a neurosurgeon.
If, at the age of several months, a previously healthy child shows signs of increased intracranial pressure and a cyst is detected during examination, surgical treatment is necessary.
When an older child is examined for a traumatic brain injury and a cyst is accidentally found, we are NOT talking about surgical treatment.
If an examination is prescribed due to speech delay or developmental delay, then the cyst found is a reason to consult with a surgeon to understand whether this cyst is associated with these symptoms.
When a school-age child is examined due to the appearance of severe headaches, the cyst found should be discussed with a neurosurgeon. Perhaps surgery will help eliminate the cause of these pains.
If a child who practices martial arts or boxing undergoes a mandatory MRI (young athletes are required to undergo examinations before competitions), during which a cyst is accidentally discovered, it is necessary to obtain advice from a neurosurgeon about the possibility of practicing these sports. A cyst without additional symptoms in older children is usually not life-threatening. But it has contraindications for engaging in traumatic contact sports, primarily martial arts and boxing, and to a lesser extent football and hockey. This cyst does not require surgical treatment.
Surgical removal of a spinal cyst
Surgical treatment of spinal cysts is performed to eliminate compression of the roots and spinal cord, improve blood circulation, restore impaired sensitivity and motor activity, as well as dysfunction of internal organs. And, as a result, surgical treatment of spinal cysts allows you to prevent disability and restore maximum performance.
As a rule, large tumors are removed. The extent and type of surgical intervention is determined by the neurosurgeon after diagnosis. Usually the tumor is removed by puncture or completely excised with all its walls.
Surgeries to remove spinal cysts can be performed using endoscopic methods or under X-ray or CT control, which significantly reduces the risk of postoperative complications.
Basic signs
Acquired and congenital vertebral cysts are classified according to the place of their formation. Symptoms of the pathology are largely related to the location of the pseudotumor, its type, size, and stage of growth. Sometimes the neoplasm develops for a long time, without giving obvious signs, and sometimes it causes pain to the patient in the early stages. The severity of pain is determined by the pressure of the cyst on the spinal roots and its proximity to the nerve ganglia.
There are main signs that develop in all types of benign vertebral tumors:
- Sharp and dull pain, concentrated in the area of the cystic capsule, which disturbs the patient even at rest, intensifying with movement. Usually there is a return of pain (irradiation) to the thoracic and pelvic region, buttocks and limbs.
- Radicular syndrome, which develops with the growth of spinal cysts localized near the spinal nerve root and ganglia (nerve plexuses), which are compressed as the tumor grows and moves. It manifests itself:
- pain and shooting in completely different parts of the body - neck, arms, legs, lower back, sacrum, behind the sternum, in the esophagus, stomach, which is determined by which nerve node is irritated;
- muscle weakness and atrophy (shrinkage);
- impaired sensitivity in the legs and arms, as well as in the area of the affected root.
- If a spinal cord cyst has formed, then as it enlarges, neurological manifestations of varying severity occur:
- increasing weakness in the lower extremities, gradual atrophy of muscles controlled by the affected spinal nerves;
- impaired skin sensitivity to pain, cold and heat due to damage to cells that perceive pain and temperature fluctuations;
- burning sensation, cold goosebumps, tingling, numbness in the arms, legs, fingers;
- headaches, sound hearing impairment (noise, ringing), dizziness, feeling of pulsation in the head, increased blood pressure;
- double vision, blurred vision, spots and threads before the eyes;
- sudden loss of consciousness, seizures;
- disruption of the intestines and genitourinary system;
- the appearance of lameness, loss of coordination of movements, balance, changes in gait.
Symptoms
A retrocerebellar arachnoid cyst manifests itself in the symptoms listed below.
General cerebral
The human brain has a limited volume, so as the tumor grows it begins to put pressure on the soft tissue, which causes:
- headache of a bursting nature, worsening at night and in the morning;
- nausea causing vomiting;
- psychomotor disorders: inappropriate behavior, uncontrolled movements, aggression, suicidal tendencies;
- congestion detected during fundus examination.
Focal
By touching the brain structures, the fluid-filled cerebrospinal fluid membrane creates a lesion and causes:
- In the occipital lobe:
- gradual decrease in vision;
- visual hallucinations;
- agnosia – failure to recognize objects;
- blurred vision, disorientation.
- In the temporal lobe:
- convulsions;
- hallucinations;
- impairment of auditory perception.
- In the frontal lobe:
- speech disorder;
- muscle hypertonicity;
- "drunk" gait;
- In the parietal lobe there is a disturbance of perception and sensitivity.
Causes
If the appearance of cysts was preceded by a difficult pregnancy in the expectant mother, experts call such tissue defects primary. Provoking factors are:
- uncontrolled use of medications by a woman;
- alcohol abuse;
- past infectious diseases;
- abdominal injuries.
If the formation of a tumor occurred in the postneonatal period of life, then the reasons may be:
- neuroinfections - for example, meningitis, or encephalitis, tuberculosis or syphilis;
- surgical interventions on brain structures;
- agenesis of the corpus callosum – absence of an anatomical unit or its replacement with a cyst;
- traumatic brain injuries;
- helminthic infestations;
- intracerebral bleeding.
From the editor: Causes of epilepsy in adults
Sometimes an arachnoid vesicle is identified as a result of examinations that were performed for other indications. The reasons for such formations are not reliably known - the person himself does not remember what could have been the impetus for the formation of the intracerebral cavity.
Features of therapy
As a rule, treatment of a cyst is prescribed only after a full diagnostic examination, which is performed using computed tomography or magnetic resonance imaging, which allows you to see the clear contours of the formations, determine their size, as well as the degree of impact on surrounding tissues.
It should be borne in mind that the presence of such cavities is not necessarily associated with cancer and usually responds well to treatment. During a magnetic resonance imaging study, the patient is injected with a special contrast agent, which makes it possible to determine what exactly is in his brain: a cyst or a malignant tumor. MRI is recommended to be performed repeatedly to constantly monitor the dynamics of the disease.
Methods for treating a brain cyst are selected based on the reasons as a result of which it arose. Emergency assistance is usually needed in the following cases:
- constantly recurring seizures;
- hydrocephalus;
- rapid increase in cyst size;
- hemorrhages;
- damage to brain structures located next to the cyst.
As a rule, non-dynamic brain cysts do not require intervention, while dynamic ones are treated using medicinal and surgical methods.
Traditional treatment involves the use of various medications, the main purpose of which is to eliminate the causes of the disease. Doctors may prescribe medications to patients that resolve adhesions, such as caripain or longidase. In order to restore blood circulation, they prescribe medications aimed at reducing cholesterol concentrations, normalizing blood pressure and blood clotting.
You can provide brain cells with the necessary amount of oxygen and glucose with the help of nootropics, for example, picamilon, pantogam, instenon. Antioxidants will help make cells more resistant to intracranial pressure. In addition, immunomodulatory, antibacterial and antiviral agents are sometimes used, which are necessary in case of detection of autoimmune and infectious diseases.
The appearance of arachnoiditis signals, first of all, that the patient’s immunity is greatly weakened, which is why it is necessary to actively restore the defenses. In order to select a consistent and safe course of immunomodulatory and anti-infective treatment, you need to take a blood test. As a rule, all medications are prescribed in courses lasting about three months, repeated twice a year.
Diagnostics
The presence of an intracranial space-occupying lesion can be determined based on a neurological examination and the results of a primary examination, which includes the following methods:
- echoencephalography (Echo-EG);
- rheoencephalography (Rheo-EG);
- electroencephalography (EEG).
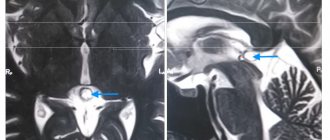
In order to clarify the location and nature of the space-occupying neoplasm, MSCT and MRI of the brain with contrast are indicated. The use of a contrast agent allows for differential diagnosis between a cerebrospinal fluid cyst and another formation, since the contrast can accumulate in the liquid contents of the cystic cavity.
Based on the diagnostic results, a decision is made on the need for surgical treatment of a cystic neoplasm.
Cavity formation in the brain
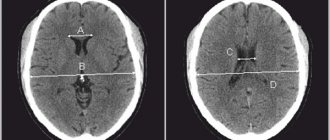
Fig2. General view of an intracerebral brain tumor with volumetric effects
1. In the photographs, the tumor is characterized by a volumetric component in the process of growth with an increase in its own mass, the so-called “plus tissue” sign.
Fig3. General view of a brain tumor in the frontal lobe on CT
2. Brain tumors have a mass effect, due to the volumetric influence of their own stroma, displacing and expanding the normal anatomical structures of the brain.
Fig4. An example of the volumetric effect of a tumor on the corpus callosum, shown on an MRI image
3. For benign brain tumors, it is typical to have clear boundaries on MRI and CT, since they have a capsule that separates them from brain tissue, a so-called expansive growth pattern (as a result of an increase in size, adjacent parts of the brain are displaced, pushed aside), relatively slow growth rates and absence of metastasis.
Fig5. example of a benign tumor (indicated by an asterisk), with a capsule, expansive growth and volumetric effect on MRI
4. For malignant brain tumors, the absence of clear contours and boundaries is typical; on the contrary, their edges are not visible, they are characterized by an infiltrative type of growth (that is, they spread their cells between the cells of healthy tissue - infiltration), necrotic decay (in the center the tumor begins to devour itself due to lack of nutrition, which leads to self-digestion of the central areas of the tumor), high rates of growth and development (short-term dramatic outcome) and metastasis (spread of the tumor to neighboring areas of the brain along the membrane and through the cerebrospinal fluid).
Fig6. Malignant tumor of the left frontal lobe with edema, necrotic decay and without distinct boundaries
5. In MRI and CT images, brain tumors in most cases accumulate contrast agent after intravenous contrast enhancement, which is a sign characteristic of tumors, although some tumors do not accumulate contrast, but this is more typical for the initial stages of formations.
6. The tumor changes the MR signal, becoming brighter or darker in the brain substance, since it consists of a separate type of tissue, although there are tumors that are “not visible” on imaging or not visible without contrast. Almost all brain tumors are visible on MRI, but can be missed on CT.
Fig7. An example of a change in brightness (MR signal) on a tomography in a region of the brain affected by a tumor
7. Perifocal edema is a feature not only of a brain tumor, but is very characteristic of tumor formations affecting the substance of the brain. Edema increases the mass effect of the tumor, leads to increased intracranial pressure and can cause displacement of brain structures or their pinching in anatomically narrow places (herniation).
Fig8. Severe perifocal edema of the brain substance surrounding the tumor on an MRI image
Due to the fact that brain tumors are not always represented by ovoid, round formations, as patients are accustomed to perceive them, and other pathological processes in the body tissues can lead to exactly this kind of shape, diagnosis becomes quite difficult and sometimes requires extraordinary knowledge and experience.
Cysts in the brain are benign neoplasms, which are a bubble with liquid contents inside. Young children and adults face a similar problem. Not everyone knows what a cyst is.
Editor's note: Causes of headaches with nausea
They are localized both in the left hemisphere and in the right. The clinical picture of the disease largely depends on this. Congenital cysts most often appear between the ages of 30 and 50 years. The growth of these tumors can be fast or slow.
In the latter case, wait-and-see tactics are often used. A cyst in the brain can be arachnoid (located in the area of the arachnoid membrane) and intracerebral. Depending on the location, the following types of neoplasm are distinguished:
- pineal gland;
- dermoid;
- choroid plexus;
- colloidal.
Types of cerebrospinal fluid cysts and reasons for their development
Depending on the origin, cerebrospinal fluid cysts can be:
- primary;
- secondary.
They will be called primary, or true, if they were formed during intrauterine development and already existed by the time the child was born.
Secondary arachnoid cystic cavities are not congenital and arise due to acquired pathology. The size of cerebrospinal fluid cysts varies from a few millimeters to 3-5 or more centimeters, which undoubtedly affects symptoms and prognosis.
The causes of a cerebrospinal fluid cyst are:
- Inflammatory processes in the membranes of the brain - meningitis, viral or bacterial arachnoiditis;
- Scarring after neurosurgical surgery;
- Suffered traumatic brain injuries;
- Hemorrhages under the arachnoid membrane, leaving collagen adhesions after resorption;
- Some malformations of the brain are underdevelopment of the corpus callosum;
- Systemic collagenoses, when the formation of connective tissue in both the meninges and other organs is disrupted;
- Genetically determined focal splitting of the arachnoid membrane during intrauterine development;
- Infections, alcohol abuse, smoking during pregnancy.
Secondary cerebrospinal fluid cysts are the result of scarring in the arachnoid membrane , therefore the walls of the cyst will have scar growths.
In true cysts, the walls of the cavity are formed by the arachnoid medulla and microglia.
an example of the development of a cerebrospinal fluid cyst due to inflammation
Other types of brain cysts
The following types of cysts are also common:
- Cyst of the epiphysis of the brain, the symptoms of which are severe headaches, drowsiness, disorientation, double vision. It also makes walking difficult. At the initial stage of the disease, drug treatment is used. A neglected cyst that increases in size is removed surgically.
- Vascular plexus cyst is a benign neoplasm that manifests itself at certain stages of fetal development in the womb. Such a brain cyst in a child most often resolves on its own. In some cases, a brain cyst in a newborn occurs as a result of complications during pregnancy and childbirth. Infectious infection of the fetus can also lead to it. In rare cases, this formation leads to pathological changes in other body systems. A congenital brain cyst is determined using a procedure called neurography. It is absolutely harmless to the child's health. Diagnosis of such a cyst in adults is made using ultrasound examination.
- Pseudocyst of the brain in newborns occurs in 1% of premature infants. It is detected by ultrasound in the first 24 hours of a child’s life. This fetal brain cyst occurs as a result of hemorrhage of the germinal matrix. It can be unilateral or bilateral. Pseudocysts are the safest health consequence of childbirth. They do not require special treatment. As a rule, by the first year of a child’s life they completely resolve.
- A cerebrospinal fluid cyst is a neoplasm that arises between the meninges. Its formation is promoted by inflammatory processes (meningitis, stroke), trauma and surgery. It is diagnosed in adulthood, since in the early stages its symptoms are practically not expressed. Symptoms of a liquor cyst: nausea, vomiting, mental disorders, loss of coordination, convulsions, paralysis of the limbs.
- A subependymal cyst occurs in newborns after a cerebral circulatory disorder or during hypoxia (insufficient oxygen supply to the brain). This disease requires medical supervision.
- Porencephalic cyst of the brain is a formation that occurs in its tissues due to melting of the affected area. It leads to very serious consequences such as hydrocephalus and schizencephaly.
- A lacunar cyst forms in the area of the pons, in the cerebellum, subcortical ganglia, and optic thalamus. Most often it occurs as a result of age-related changes and atherosclerosis.
- Colloidal cyst is of congenital origin. It appears as a result of embiogenesis. A person can have it all his life, but it does not cause him any problems. It is believed that it is hereditary. This cyst blocks the flow of fluid. It is often accompanied by headache, epileptic seizures, weakness in the legs and high intracranial pressure. The symptoms of this disease manifest themselves most clearly in adulthood. Sometimes this disease causes hydrocephalus and cerebral hernia. In rare cases, it is fatal.
Colloidal cyst
Cysts of different parts of the brain
In some cases, doctors diagnose the following diseases:
- A pituitary cyst of the brain is a benign formation. It appears mainly in people aged 30-40 years. There are practically no pituitary cysts in children and adolescents. This disease is dangerous because the tumor affects the central nervous system. Most often, such a cyst is removed surgically.
- A cerebellar cyst can occur for a number of reasons. Most often, its treatment is aimed at resolving adhesions. If the cyst is formed as a result of autoimmune processes or infection, anti-inflammatory therapy will be needed. Surgical intervention is performed if there are signs of hemorrhage, convulsions, or loss of coordination of movement. In most cases, this disease is completely curable.
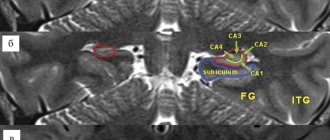
Localization
A cerebrospinal fluid cyst is a neoplasm located between the dura mater and the arachnoid membrane of the brain. Arachnoid cystic formations are most often localized above the sella turcica, in the area of the Sylvian fissure or cerebellopontine angle. They are located in both hemispheres of the brain, sometimes only in the left hemisphere, sometimes in the right part of the crown or middle cranial fossa.
Basically, these cavities are single in nature (80%), and multiple locations occur (12%). The diagnosis is confirmed 4 times more often in men than in women.
All ages are submissive: cysts in infants
In newborns, cystic formations formed either during intrauterine development or appeared as a result of birth trauma. The same reasons precede the appearance of cysts in infants, and, in addition, new prerequisites are added, for example, infectious and inflammatory processes or hematomas resulting from injuries, which result in cerebral circulatory failure, leading to hypoxia and ischemia, and, consequently, to the death of neurons in some part of the brain (the place where the cyst forms).
Subsequent degeneration of the nervous tissue, its necrosis, will serve as a good place for the formation of a cavity, which will begin to accumulate fluid, enlarge and compress neighboring areas and liquor-conducting pathways. This will most likely result in hydrocephalus and give certain neurological symptoms, delayed growth and development of the child.
A cyst in a child’s head can form anywhere; therefore, the main types of cystic formations localized in the brain are distinguished:
- Arachnoid cyst resulting from trauma and inflammatory processes. The habitat can be any part of the brain, characterized by rapid growth, manifested by hydrocephalus with its characteristic symptoms.
- The most severe forms of the cystic process include the subependymal cyst. Its cause is circulatory failure in the brain followed by ischemia. Such a cyst requires increased attention to itself and constant monitoring of the child (MRI annually to avoid excessive growth)
- A choroid plexus cyst, which develops in the fetus and by the time the baby is born, usually disappears safely.
Choroid plexus cysts (pictured) - in most cases, a phenomenon that does not require concern
The cystic process is diagnosed in early infancy using neurosonography (ultrasound), and the cyst is removed surgically.
Treatment
Even knowing about the presence of a simple, congenital, frozen cyst, the patient should not worry. The following drugs are prescribed against liquor cysts to improve metabolism:
- vitamins;
- to reduce cholesterol levels;
- for resorption of adhesions;
- to normalize blood pressure;
- anti-inflammatory drugs.
Further observation and supportive therapy will be required. It is important to be systematic in treatment and follow doctors’ recommendations.
Indication for surgery
If the tumor tends to increase, creates pressure on the functional areas of the brain, and neurological disorders have appeared, there are grounds for the use of surgical treatment methods.
Surgical intervention is indicated:
- when convulsions occur;
- if the tumor grows quickly;
- if cerebrospinal fluid accumulates, dropsy occurs;
- when the cavity is located in nearby parts of the brain.
Types of surgical procedures
When treating arachnoid cysts, the following operations are performed:
- Shunting. The procedure is performed under general anesthesia and lasts about an hour. The shunt is installed through small incisions in the head, neck, and abdomen. It removes excess fluid into the abdominal cavity, where it is organically processed by the excretory system. The patient will feel relief of some symptoms immediately after surgery, but it may take weeks for other functions to return.
- Endoscopy. The modern method of neurosurgery makes it possible to remove a pathological formation through a small hole in the skull.
- Trepanation of the skull. Rupture of the cyst shell, spillage of fluid, hemorrhage into the cavity are indications for complete excision. Requires long healing.
- Proton therapy. The modern treatment method has a great advantage over traditional radiation therapy. Gamma rays, along with the source of the disease, also affect nearby healthy tissues of the body. Proton beams, releasing maximum energy, thanks to precise dose programming, stop at a given depth, specifically heal the sore spot, and return back. The harmful effects on healthy tissue are significantly reduced.
- Radiosurgery. It is distinguished by a single dose of radiation, which kills cells in 1 session. Separate beams of radiation, each carrying a small dose, along a certain trajectory reach the desired cavity (intersection point) and collectively release energy without affecting other structures of the body.