The full functioning of human reflex activity is largely determined by the functioning of the nervous system.
If the nervous system is affected, then the human body malfunctions - all its basic functions are disrupted: the frequency and rhythm of the heart, breathing, coordination of movements and walking skills, as well as nutrition.
If the disorder occurs in the brain, the person may lose all basic life skills such as speaking, writing, and reading.
Despite the fact that medullary gliosis is not a disease, this abnormal process contributes to the occurrence of serious disturbances in a person’s normal life.
White matter gliosis - what is it?
This process is a fairly severe morphophysical disorder of a pathological nature, which occurs in the tissues of the brain under the influence of certain environmental factors that are traumatic in nature.
This process is accompanied by a significant growth of the scar formed in the injured area where neurons have died.
This scar is medically called neuroglia.
This term refers to the additional tissue substance of the brain, which makes up about 30% of the total mass of brain tissue. The main function of neuroglia is to protect the brain matter from the effects of pathogenic microorganisms and various damages. Neuroglia also produce useful substances and take part in metabolic processes.
When brain cells are injured or infected, the volume of neuroglia increases. Scar tissue usually forms in the damaged area of dead neurons.
However, neuroglia excludes its formation, since it itself becomes a kind of bioconductor.
The main problem is that neuroglia are not able to function like natural nervous tissue. This in turn causes serious health problems.
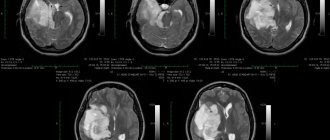
Foci of gliosis are very clearly visible on MRI of the brain.
When brain tissue is damaged, the following symptoms are observed:
- Fatigue that is chronic. A person experiences causeless bouts of fatigue, even while at rest.
- Prolonged and unremitting headaches, which may be accompanied by dizziness, nausea, fear of light, and vomiting.
- Sudden jumps in blood pressure, including conditions of arterial hypertension of varying degrees of complexity.
- Epileptic seizures and convulsions. If a large lesion is present, neurological symptoms may also be observed.
- Impaired motor coordination associated with cerebellar disorders, which leads to injuries of varying severity.
- Problems with short-term and long-term memory.
- The occurrence of sound and olfactory hallucinations.
- Lack of ability to clearly express one's thoughts out loud and in writing, which is caused by the formation of a lesion in the brain in the area responsible for the formation of oral and written language.
- Sudden mood swings, which can be accompanied by increased aggression, depressive states, and absolute apathy towards everything.
Cerebral gliosis: to worry about or not to worry about?
If the skin is injured, scars form on it. Similar scars can form in the brain.
We talk about such a common pathology as gliosis with Oksana Egorovna Volkova, a radiologist, chief physician and executive director of MRI Expert Lipetsk.
“An MRI revealed gliosis of the brain,” sounds scary. Oksana Egorovna, tell us what cerebral gliosis is?
This is the replacement of dead neurons with neuroglial cells. There are different types of cells in the brain. The main cells are neurons, thanks to which neuropsychic processes occur. These are the very cells that are said to “not recover.”
Another type is glial cells (neuroglia). Their function is auxiliary; they participate, in particular, in metabolic processes in the brain.
Nature, as we know, abhors a vacuum. Therefore, if neurons die for one reason or another, then their place is taken by neuroglial cells. Here we can draw an analogy with skin trauma. If the damage is significant enough, a scar will form in its place. An area of gliosis is also a “scar”, but in nervous tissue.
— Is cerebral gliosis an independent disease or a consequence of other diseases?
This is a consequence of other diseases.
Read the material on the topic: Vegetative-vascular dystonia: diagnosis or fiction?
— For what reasons do glial foci of the brain develop?
The causes of cerebral gliosis are different. It can be congenital, and also develops against the background of a large number of brain pathologies. The most common foci of gliosis appear in response to a vascular disorder. For example, there was a blockage of a small vessel. The neurons in the area of its blood supply died, and their place was filled with glial cells. Gliosis occurs during strokes, cerebral infarctions, and after hemorrhages.
IF THE SKIN DAMAGE IS SIGNIFICANT, THEN A SCAR WILL BE FORMED IN ITS PLACE. AN AREA OF GLIOSIS IS ALSO A “SCAR,” BUT IN NERVOUS TISSUE.
It can also form after injuries, with hereditary diseases (for example, a fairly rare disease - tuberous sclerosis), neuroinfections, after brain surgery, poisoning (carbon monoxide, heavy metals, drugs); around tumors.
— Before preparing the interview, we specifically studied people’s requests and found out that along with the phrase “gliosis of the brain,” Russians are trying to find out from search engines whether it is dangerous, fatal, and are even interested in the prognosis of life. How dangerous is cerebral gliosis for our health?
This depends on the cause of gliosis and what consequences the gliosis lesion itself can cause.
For example, a small blood vessel becomes blocked in a person and a patch of gliosis forms at the site of death. If everything is limited to this, and the site of gliosis itself is in a “neutral” place, then there may be no consequences “here and now”. On the other hand, if we see such a hearth, even a “silent” one, we need to understand that it appeared there for a reason.
Sometimes even a small focus of gliosis, but located in the temporal lobe, can “make itself known”, causing the appearance of epileptic seizures. Or an area of gliosis may disrupt the transmission of impulses from the brain to the spinal cord, causing paralysis of one limb.
Read the material on the topic: Is a brain cyst always a dangerous diagnosis?
Thus, it is always necessary to try to get to the bottom of the cause, since in some cases gliosis is a kind of “beacon”, a warning signal that something is wrong - even if now it does not bother the person at all.
— Cerebral gliosis and cerebral glioma are not the same thing?
Definitely not. Glioma is one of the most common brain tumors. Gliosis has nothing to do with tumors.
— Gliosis cannot develop into oncology?
No. It can occur with brain tumors, but as a parallel phenomenon - for example, against the background of concomitant vascular pathology.
Read the material on the topic: Why is MRI of cerebral vessels prescribed for headaches?
— What are the symptoms of cerebral gliosis?
The most diverse - based on the variety of pathologies that cause areas of gliosis to form. There is no specific symptom(s) of gliosis.
GLIOSIS HAS NO RELATION TO TUMORS. IT CANNOT GROW INTO ONCOLOGY.
Headaches, dizziness, unsteadiness of gait, variability in blood pressure, memory impairment, attention problems, sleep disorders, decreased performance, impaired vision, hearing, epileptic seizures and many others may occur.
— Oksana Egorovna, is gliosis visible on MRI?
Undoubtedly. Moreover, we can say with a certain probability what its origin is: vascular, post-traumatic, postoperative, after inflammation, with multiple sclerosis, etc.
Read the material on the topic: If an MRI of the brain showed...
— How can cerebral gliosis affect the patient’s quality and life expectancy?
It depends on the underlying disease. Asymptomatic gliosis after a minor traumatic brain injury is one thing, but a lesion in the temporal lobe that causes frequent epileptic seizures is another. Of course, the amount of damage to the nervous system and the resulting disorders (for example, during a stroke) also matter.
— Do glial lesions in the brain require special treatment?
And here everything depends on the underlying pathology. This issue is resolved individually by the treating doctor.
Read the material on the topic: What is hidden behind the diagnosis of dyscirculatory encephalopathy?
— What type of doctor should a patient see if gliosis is detected during an MRI scan of the brain?
To a neurologist, if indicated - to a neurosurgeon.
— If magnetic resonance imaging reveals foci of gliosis in the brain, does such a patient need dynamic observation?
Yes. Its frequency depends on the cause that caused the appearance of gliosis, the number and size of foci, their “behavior” during dynamic observation, etc. These issues are resolved by the attending physician and the radiologist.
You may also find it useful:
Does osteochondrosis exist?
Which tomograph is better: open or closed?
Why is electroencephalography needed? Complete patient guide
For reference:
Volkova Oksana Egorovna
In 1998 she graduated from Kursk State Medical University.
In 1999 she completed her internship in the specialty “Therapy”, in 2012 - in the specialty “Radiology”.
She worked as a radiologist in.
Since 2014, he has held the position of chief physician and executive director.
Types of disease
Because, due to the pressure of developing neuroglia, necrotic cells gradually die and die.
Against this background, small areas of gliosis of different sizes and shapes appear, which can be located in any area of the brain.
The pathological process is classified into 7 forms:
- Intraventricular - lesions form inside the ventricles of the brain, which contributes to a significant reduction in their volume, as well as the volume of cerebrospinal fluid.
- The formation of lesion islands that form around atherosclerotic vessels, which are severely compressed under pressure.
- Regional - involves the formation of single lesions that are concentrated outside the brain tissue (this type of neuroglia is the simplest, since it does not affect the central region).
- Fibrous - gliotic foci can be filled with fibers, which can have different lengths and sizes.
- Massive neuroglia - multiple foci are formed in different areas of the brain tissue (when scanning, the image is displayed as a large spotted field).
- Intrathecal – altered areas are located under the inner membranes of the brain, which significantly complicates the diagnosis of the disease.
- Anisomorphic - altered lesions are located chaotically.
Foci of gliosis
Depending on how focal changes are displayed on film during MRI of the brain, gliosis is divided into the following groups:
- Hypodense - are quite rare, do not have a specific structure and are extremely difficult to paint;
- Hyperintense – characterized by a pronounced structure, easily stained during examination.
Depending on the number of pathological zones, neuroglial foci are also divided into:
- single – when performing an MRI of the brain, single foci of gliosis are very clearly visible;
- multiple – are also clearly displayed during the examination.
Unit formations
Such formations are more common in different age groups.
MRI of the brain can detect foci of gliosis in both infants and elderly patients.
In the first case, the formation of altered lesions may be associated with the consequences of postpartum trauma; in the second, it may be the result of degeneration of brain tissue due to age-related changes.
This process is a natural age-related change that is visible in 60% of cases when scanning white matter in people over 85 years of age.
As a rule, such lesions are detected by chance, since they do not cause discomfort. However, when lesions form in the left frontal lobe, they often provoke the appearance of hallucinations.
This phenomenon is due to the fact that in this part there are the most important centers responsible for deep feelings and sensations.
The main feature of such a lesion is that it is not predisposed to proliferation and carries a significant risk in the development and exacerbation of chronic diseases.
Causes
There are two groups of causes of gliosis of vascular origin:
The first group is direct, affecting the organic structure of the brain matter:
- Ischemic stroke. This pathology is characterized by an acute circulatory disorder due to an embolus or thrombus entering the bloodstream. The consequence of an ischemic stroke is cerebral infarction and softening of the white and gray matter. As a result of the lesion, a protective mechanism is activated, and the lost neurons are replaced by glial cells.
- Hemorrhagic stroke. The condition is characterized by hemorrhage into the thickness of the brain substance due to a violation of the integrity of the vessel. It is not the tissue into which the hemorrhage occurred that suffers more, but the area that, due to lack of blood, suffers from oxygen and nutritional starvation.
- Atherosclerosis of cerebral vessels. The pathology is characterized by a violation of fat metabolism and, as a consequence, the deposition of adipose tissue on the inner wall of the arteries. This leads to impaired blood flow: the brain substance receives less oxygen and nutrients. Particularly needy areas suffer, where replacement occurs.
The second group is indirect causes that indirectly affect brain tissue:
- Heart diseases: heart failure, arrhythmia, coronary heart disease. Not enough blood reaches the brain.
- Arterial hypertension and hypertension. The blood vessels narrow, the brain matter receives less oxygen.
- Diabetes. Small blood vessels are affected, causing small lesions of gliosis.
- Smoking, alcohol. The toxic effect of poisons “washes out” nutrients from neurons and kills them.
- Sedentary lifestyle.
- Stress, anxiety, psycho-emotional stress, hard physical work, intellectual exhaustion.
Multiple lesions
Such lesions are much less common compared to single gliosis of the brain. This pathology can develop against the background of various diseases of the blood vessels, the central nervous system (in particular, white matter), as well as connective tissues.
Typically, the cause of such lesions is atherosclerosis, as well as previous strokes and heart attacks. Also, multiple lesions can occur due to traumatic brain injury.
It is important to note that with brain trauma, a process of necrosis occurs, and in different areas and in different areas. As a result, it is the subcortical foci of tissue death that are much more susceptible to gliotic degeneration.
When receiving minor head injuries, the size of the lesions is no more than a few millimeters. Thanks to this, the functions of human thinking remain practically unchanged.
If a patient has even the smallest structural changes, they can easily be detected using an MRI examination.
MRI of the central nervous system is the method of choice for patients with clinical manifestations of multiple sclerosis, approved by an international group of experts in 2001. The diagnosis of multiple sclerosis is based on confirmation of dissemination of the disease in space and time, as well as the exclusion of other diseases that can mimic the clinical and laboratory manifestations of multiple sclerosis.
MR criteria for assessing multiple sclerosis are based on the detection of local lesions in the central nervous system, which have a typical morphology, type of distribution, and evolution on T2-WI, FLAIR, pre- and post-contrast T1-WI for this disease. The first criteria developed by the MAGNIMS group in 2010 are known as the McDonald criteria. Since the beginning of 2011, as new information has emerged from studies, including using MR scanners with high (3.0 T and 7.0 T) magnetic field strength, there has been a need to revise some points of the 2010 McDonald criteria. The result of this work was the creation of a new edition of the MAGNIMS criteria for 2021.
MAIN PART
According to the 2010 McDonald criteria for multiple sclerosis, spatial dissemination can be defined as the presence of at least one lesion on T2-weighted imaging in at least 2 of 4 locations:
- juxtacortical;
- periventricular;
- infratentorial;
- spinal cord.
According to MAGNIMS 2021, it is necessary to increase the number of required lesions in the periventricular space from 1 to 3, as well as to identify an additional localization - the optic nerve.
Periventricular lesions
The presence of a single lesion in the periventricular space does not always reflect a high probability of the presence of a demyelinating process, which is confirmed by the incidental detection of periventricular lesions in 30% of patients examined for migraine. The presence of 3 or more periventricular lesions is the most accurate threshold value. However, it should be remembered that the presence of a single periventricular lesion in children (as well as one or more hypointense lesions on T1-WI) allows one to reliably differentiate multiple sclerosis from demyelinating diseases with a monophasic course.
Lesions in the optic nerve
20-31% of patients with clinically isolated syndrome debut in the form of optic neuritis. Compared with other clinical manifestations, adult patients with optic neuritis are more likely to have a monophasic course of the demyelinating process. At the same time, the presence of at least one T2-weighted hyperintense lesion of the brain in children with optic neuritis is highly likely to correspond to manifestations of multiple sclerosis. The absence of foci in the brain is characteristic of a monophasic demyelinating process.
Cortical lesions
Data from pathological studies have shown widespread involvement of gray matter in the demyelinating process in multiple sclerosis. At the same time, many cortical lesions remain invisible in MR studies of at least 1.5 Tesla and 3.0 Tesla scanners.
Since intra-, leuko-, and juxtacortical lesions cannot be reliably distinguished in studies performed on most MR scanners, the group of experts adopted the term “cortico-juxtacortical lesions” to designate them. According to the 2010 McDonald criteria, dissemination over time can be established based on one of the following:
- the presence of at least one new lesion on T2-weighted images or a contrast-enhancing lesion on the control MRI (if a control study is available);
- simultaneous presence of contrast and non-contrast lesions on one study.
Nonenhancing hypointense lesions on T1-weighted images (“black holes”) represent chronic lesions of severe axonal damage. Criteria for dissemination over time have not changed since 2010, and the presence of nonenhancing black holes is not an additional criterion for dissemination over time in adult patients with multiple sclerosis. The presence of “black holes” is a sign that allows differentiating multiple sclerosis and monophasic demyelinating process in children.
SYMPTOMIC AREAS
The decision as to whether an identified lesion is symptomatic is often very difficult to make. The division of lesions into symptomatic/asymptomatic is quite simple in the brain stem, spinal cord, but not in other localizations. Based on this information, the panel recommends that no distinction be made between symptomatic/nonsymptomatic lesions.
IMAGING THE SPINAL CORD
According to the 2010 McDonald criteria, asymptomatic lesions in the spinal cord may also contribute to the assessment of disease dissemination in time and space. Based on these data, it is recommended to perform MRI of the spinal cord in the absence of spinal neurological symptoms to supplement data on the dissemination of the disease.
When the distribution of lesions in the brain does not meet the criteria for spatial dissemination, MRI of the entire spinal cord is recommended to identify additional lesions. In the presence of spinal symptoms, MRI of the spinal cord is indicated to exclude other causes (compression, tumor, vasculitis). The value of MRI of the spinal cord in assessing dissemination over time in the absence of neurological symptoms is low.
In 2021, the European expert group of the MAGNIMS society published new recommendations for the diagnostic criteria for multiple sclerosis according to McDonald. The work is the result of a consensus adopted on the basis of expert opinions and evidence-based medicine. Key changes to the previously used criteria primarily concern the “dissemination in space” section:
- The optic nerve is added to the existing four sites characteristic of multiple sclerosis (periventricular, juxtacortical, infratentorial and spinal cord)
Rationale: ~25% of patients with clinically isolated disease will present with optic neuritis
- The presence of at least 3 (three) foci of periventricular localization
Rationale: Single periventricular lesions are often incidental findings in some conditions (eg, migraine); the presence of at least 3 (three) lesions increases diagnostic accuracy in clinical studies
- Cortical localization of lesions added to the previously existing juxtacortical localization
Rationale: Postmortem studies have shown large amounts of gray matter damage in the brain in multiple sclerosis. Newer MRI techniques have high sensitivity for localizing lesions. However, most cortical lesions remain invisible on images obtained with conventional 1.5 and 3.0 Tesla MR scanners.
Comment: since it is difficult to differentiate cortical and juxtacortical lesions using traditional MR scanners, such localizations are usually combined under the general term “cortico-juxtacortical”.
- No more distinction is made between symptomatic and asymptomatic lesions when assessing dissemination in space/time; all detectable lesions are taken into account
Rationale: Previously, the McDonald 2010 criteria did not include symptomatic lesions (eg, a lesion in the spinal cord in a patient with corresponding focal neurological symptoms) in the diagnostic criteria; however, deciding whether a lesion is symptomatic is often difficult to decide. Spatial dissemination The new MAGNIMS 2021 criteria define spatial dissemination as involving at least two (2) of the following five (5) locations in the central nervous system:
- periventricular: ≥3 lesions;
- cortico-juxtacortical: ≥1 lesion;
- infratentorial: ≥1 lesion;
- spinal cord: ≥1 lesion;
- optic nerve: ≥1 lesion.
Dissemination over time can be defined in two ways:
- the appearance of a new lesion compared to the previous study (regardless of time);
- lesion hyperintense on T2-weighted images and/or demonstrating contrast enhancement on T1-weighted images;
- presence on the same study of lesions demonstrating and not demonstrating contrast enhancement.