Polyneuropathy, or peripheral neuropathy, occurs as a result of damage to the peripheral nerves and often results in symptoms such as weakness, numbness and pain, usually in the arms and legs. But polyneuropathy can also affect other areas of the body. Peripheral neuropathy may develop in one nerve (mononeuropathy), two or more nerves in different areas, or may involve many nerves (polyneuropathy).
The peripheral nervous system transmits information from the brain and spinal cord (central nervous system) to the rest of the body. Peripheral neuropathy can result from traumatic injuries, infections, metabolic disorders, hereditary causes, and exposure to toxins. One of the most common causes of polyneuropathy is diabetes mellitus.
Patients with peripheral neuropathy typically describe pain as a tingling or burning sensation. In many cases, symptoms decrease if compensation occurs for the underlying disease.
Each nerve in the peripheral nervous system has a specific function, so symptoms depend on the type of nerve that is damaged. Nerves are divided into:
- Sensory nerves that receive sensations from the skin, such as temperature, pain, vibration, or pressure
- Motor (motor) nerves that control muscle movement
- Autonomic nerves that control functions such as blood pressure, heart rate, digestion, and bladder function
Information about polyneuropathy
The word "polyneuropathy" is translated from Greek as "damage to many nerves." This term very accurately describes the essence of the pathology. All structures of the body are entangled in a network of thin nerve fibers, which are divided into three groups:
- motor: responsible for motor functions;
- sensory: provide tissue sensitivity;
- Autonomous (vegetative): necessary for the unconscious regulation of the activity of certain structures, for example, blood vessels or internal organs.
Damage to certain fibers inevitably leads to disruption of their functions. The most common is mixed polyneuropathy of the lower extremities, in which symptoms of dysfunction of the sensory and motor nerves appear.
Make an appointment
Causes
Damage to peripheral nerves can occur due to the following conditions:
- diabetes mellitus: the most common cause of polyneuropathy, resulting from metabolic disorders in the myelin sheath of nerve fibers; mainly the lower extremities are affected;
- severe and prolonged deficiency of B vitamins necessary for the full functioning of the nervous system;
- infectious diseases: HIV, tick-borne borelliosis, leprosy;
- renal failure;
- alcohol abuse;
- acute and chronic intoxication, including drugs;
- autoimmune diseases: damage occurs against the background of a malfunction of the immune system; the most common are chronic and acute inflammatory polyneuropathy (Guillain-Barré syndrome);
- long stay in intensive care, for example, with extensive injuries or serious illness;
- exposure to ionizing radiation;
- pregnancy: carrying a child can cause vitamin deficiency and autoimmune lesions.
In addition, there are hereditary forms of the disease, transmitted from relatives, as well as idiopathic polyneuropathy, the cause of which cannot be determined.
Polyneuropathy in oncology
Side effects of drugs spoil the patient’s life, requiring dose reduction and increasing intervals between doses, but with chemotherapy, toxic reactions are commonplace, due to the genetic relationship of malignant and normal cells. Damage to the nervous system is typical for a small number of cytostatics, some targeted and immuno-oncological drugs.
Brain damage caused by drugs is observed very rarely - less than 3%; as a rule, this non-persistent complication completely regresses and does not remind itself in later life, as shown by an examination of testicular cancers cured from malignant tumors.
Damage to peripheral nerves - peripheral polyneuropathy is experienced by more than 60% of patients from one to three months after completion of chemotherapy; after six months, symptoms remain in every third person; chemotherapy leaves neurological consequences for every tenth person for life.
Features of damage to the nervous system during antitumor therapy:
- in the initiation of pathology by certain drugs, and not by all cytostatics;
- in the appearance of pathology at a certain total dose administered;
- the impossibility of predicting its course;
- in the predominant violation of peripheral sensitivity;
- in the duration of symptoms;
- in frequent intensification of manifestations after completion of chemotherapy;
- in the impossibility of preventing complications.
Each drug creates a specific clinical picture of neuropathy, different from the symptoms after other cytostatics.
Book a consultation 24 hours a day
+7+7+78
Kinds
Polyneuropathy is divided into several types depending on the type of fibers affected:
- sensory: the nerves that provide sensitivity are affected;
- motor: disturbances in the functioning of motor nerves are detected;
- motor-sensory: mixed form, in which motor disorders predominate;
- sensory-motor: mixed neuropathy, in which sensitivity disturbances are more pronounced;
- vegetative: first place comes to disturbances in the functioning of internal organs, changes in vascular tone and associated trophic disorders.
Significant differences in symptoms are noticeable only in the initial stages of the disease. Subsequently, all nerve fibers are involved in the pathological process, and the manifestations become mixed.
There are other types of classification of the disease:
- depending on the cause: alcoholic, diabetic, idiopathic, etc.;
- depending on the location of the lesion: polyneuropathy of the upper or lower extremities;
- depending on the type of course: acute, subacute, chronic;
- depending on the mechanism of occurrence: demyelinating (the sheath covering the nerve fibers is destroyed), axonal (formed by the death of nerve processes - axons), axonal-demyelinating.
Mechanism of occurrence
The exact mechanism of damage to nerve cells is unknown; it is assumed that the drug penetrates from the blood into the intercellular fluid, from there it diffuses into the cell, where it damages the protein tubulin and other proteins.
Each drug has its own “point of application” to tubulin: taxanes break up its microtubules, platinum derivatives denature it, vinca alkaloids are disassembled into components.
The process of protein damage by cytostatics in all cells is the same, its consequences are varied:
- degeneration of nerve processes - axonopathy;
- degenerative changes in neuron cell bodies—neuronopathy;
- destruction of the myelin sheath of the nerves - myelinopathy throughout or partially.
Symptoms
Symptoms of polyneuropathy depend on its cause and the characteristics of the damage to the fibers. The most common signs of pathology include:
- decreased sensitivity of the feet and palms, leading to the subjective sensation of wearing socks or gloves;
- pain in the affected limbs (sharp or dull, short-term or nagging, usually worse at rest and at night);
- spasms and twitching of muscle fibers;
- pain when touching the skin or pressing on the affected limb;
- decreased reflexes;
- increased sweating of the extremities;
- trophic disorders: swelling, changes in skin color and dryness, trophic ulcers;
- weakness of the muscles of the arms and legs, slight tremors;
- paresthesia: pathological sensations of crawling, burning, coldness;
- muscle atrophy;
- restless legs syndrome.
Alcoholic polyneuropathy
This form of the disease most often affects the lower extremities. It develops with prolonged uncontrolled consumption of alcoholic beverages and manifests itself primarily as a burning sensation and tingling sensation in the legs. With the further development of the pathology, the patient begins to feel numbness and muscle cramps, which develop due to the concomitant lack of B vitamins.
Diabetic polyneuropathy
Elevated sugar levels cause damage to the nerves of the feet (distal version) and the upper legs (proximal version). In the first case, a person experiences a characteristic set of symptoms:
- numbness and decreased pain sensitivity;
- periodic burning pain;
- muscle weakness;
- decreased reflexes;
- impaired coordination of movements, manifested by unsteadiness of gait.
The combination of polyneuropathy with damage to small vessels leads to the appearance of trophic ulcers in the lower part of the leg. The proximal version of the lesion is characterized by sharp pain in the buttock and upper thigh, as well as gradual muscle atrophy in this area.
Clinical phenomenology of chronic renal failure
Symptoms of damage to the nerve process - axonopathy - manifest several weeks and even months later than damage to the neuron - neuronopathy.
Platinum derivatives predominantly cause sensory disturbances in the legs, which destabilizes the gait, does not give the foot a feeling of the floor, which is why the patient has to use his eyes to choose a place to place the foot. It is possible that a motor component may be associated with muscle spasms. After completion of chemotherapy, the manifestations of polyneuropathy decrease very slowly, perhaps even increasing over 3 months - a symptom of inertia.
Pactitaxel initiates sensory disturbances, usually “pins and needles” and numbness, more often in the legs than in the arms. The feeling of “burning” soles is typical, especially after high-dose chemotherapy. Motor disorders are as atypical as autonomic ones. Normalization may take up to a year.
Docetaxel affects sensory fibers, the frequency of symptoms increases with a total of 500 mg, but severe polyneuropathy is practically impossible. Every 5-6 patients develop asthenia - weakness.
Vinorelbine does not begin to ruin your life right away - after a month of weekly injections, the sensitivity of the fingers is often impaired, gastrointestinal motility decreases, which is manifested by constipation, but the most common complication is asthenia in six out of ten patients, when they complain of severe fatigue precisely from the treatment.
Oxaliplatin changes the sensitivity of the hands with tingling of the fingertips, and the disturbances appear very early - literally after the first dose, reaching a maximum on the 3rd day. Between administrations everything seems to return to normal, but in the next course it is repeated and more intensively. The peculiarity is that 3 months after chemotherapy, the symptoms of polyneuropathy are the brightest, then improvement begins, six months after chemotherapy, symptoms of impaired sensitivity in the legs come to the fore, and the hands are less bothersome.
Fluorouracil “hits” the brain, causing gait instability - cerebellar ataxia and spasmodic eye movements - nystagmus, and changes speech due to sluggishness of the tongue. High doses and multi-day infusions may be complicated by encephalopathy. The frequency and intensity of manifestations increases many times in the absence of an enzyme in the cells that destroys fluorouracil metabolites.
During administration, irinotecan
With all the variety of clinical manifestations of polyneuropathy after chemotherapy and the absence of a clear diagnostic algorithm, the neurological complication can be recognized in time, but it is absolutely impossible to predict its duration.
Diagnostics
Diagnosis of polyneuropathy requires a comprehensive examination, which includes:
- survey: identifying patient complaints, clarifying the time and circumstances of the occurrence of each symptom;
- taking an anamnesis: recording all past diseases, injuries, intoxications, chronic pathologies, hereditary risk factors, etc.;
- neurological examination: assessment of skin and proprioceptive (spatial) sensitivity, motor function, muscle strength, quality of reflexes;
- consultations with specialized specialists: endocrinologist, narcologist, toxicologist, nephrologist, etc.;
- general urine test, general blood test, blood biochemistry (determination of glucose levels, lipid spectrum, vitamins and microelements, kidney function indicators and other parameters);
- blood test for HIV and other infections;
- genetic and immunological studies according to indications;
- Electroneuromyography allows you to identify lesions of nerve fibers and exclude other diseases with similar symptoms;
- biopsy of nerve and muscle tissue;
- lumbar puncture (examination of cerebrospinal fluid) to exclude neuroinfections;
- Doppler ultrasound of the vessels of the lower extremities.
The list of examinations can be adjusted depending on the form of polyneuropathy and concomitant pathology.
Pathogenesis
The onset of the development of the disease is two factors that are related to each other: mechanical irritation of the root and/or spinal ganglion and inflammatory changes in the perineural tissue that occur as a result of penetration of the disc into the epidural space.
In this case, factors of root compression can be both disc herniations and bone growths (uncovertebral, spondyloarthritic). Compression can also be caused by hypertrophied ligaments and periarticular tissues, vascular structures (epi- and subdural hematomas, arteriovenous malformations, epidural hemangiomas).
Until now, “blank spots” remain in the pathophysiological concept of radicular pain. It is assumed that the basis of radicular pain is axonal dysfunction caused by various etiological factors, including neural compression, ischemia, damage by inflammatory and other biologically active substances. Spinal roots (unlike peripheral nerves) have a weak blood-neural barrier, making the axon more susceptible to compression injury.
Increased vascular permeability due to mechanical compression of the root leads to endoneurial edema. As a result, a precedent arises that prevents full capillary blood supply and the formation of interneural fibrosis. The spinal root receives up to 58% of its nutrition from the surrounding cerebrospinal fluid (CSF). Perineural fibrosis prevents the complete supply of axonal tissue with nutrients due to diffusion from the CSF, which also contributes to increased sensitivity of the fiber to pressure.
Studies using experimental root compression have shown that even at minimal pressure (5–10 mm Hg) venous blood flow ceases.
The occlusion pressure of the radicular arterioles is significantly higher (approximately corresponds to mean blood pressure), but depends on the potential for venous stasis. Ischemia of nerve fibers or venous congestion leads to biochemical changes that can maintain pain sensations.
Work with experimental root compression demonstrates that compensatory diffusion of nutrients from the CSF is impaired in the setting of epidural inflammation or in the presence of fibrosis.
Recent studies have shown that degenerative changes in the nucleus pulposus and annulus fibrosus can lead to local neural changes and the synthesis of algogenic agents such as metalloproteinases, tumor necrosis factor (TNF), interleukin (IL)-6 and prostaglandin E2. Pathogenetically, the pain syndrome in radiculopathy is of a mixed nature, including nociceptive and neuropathic components.
Treatment of polyneuropathy of the extremities
Treatment is aimed at eliminating the main cause of damage to nerve fibers, restoring their normal functioning, as well as eliminating symptoms that are unpleasant for the patient.
Depending on the cause of the disease, the following may be prescribed:
- drugs to correct blood sugar levels;
- antihistamines;
- immunoglobulins and glucocorticosteroids to eliminate inflammation and autoimmune damage;
- plasmapheresis and detoxification drugs;
- antibiotics for infections.
To restore nerve fibers, the following are used:
- B vitamins (milgamma, neuromultivit);
- drugs that improve blood circulation, metabolism and tissue regeneration: actovigin, cerebrolysin, berlition (especially effective for diabetes mellitus);
- angioprotectors: trental, pentoxifylline;
- means to enhance the conduction of nerve impulses to muscles: neuromidin.
Symptomatic therapy includes:
- non-steroidal anti-inflammatory drugs (ibuprofen, diclofenac, ketorolac), glucocorticosteroids (hydrocortisone, dexamethasone), analgesics (analgin, lidocaine) in the form of tablets, injections or local forms to relieve pain;
- anticonvulsants: tebantin, catena;
- antidepressants for chronic pain;
- sleeping pills according to indications.
Non-drug therapy is of great importance in the treatment of polyneuropathy. It includes:
- restorative and therapeutic massage to stimulate blood circulation in tissues, their nutrition and regeneration, as well as strengthen muscles;
- electrophoresis and phonophoresis with analgesics, B vitamins and other drugs (the use of electric current or ultrasonic waves facilitates the delivery of drugs to the affected area);
- electrical stimulation of muscles;
- magnetic therapy, UHF therapy, ultraviolet irradiation;
- darsonvalization: exposure to high frequency alternating current to improve metabolism and tissue regeneration;
- mud therapy: mud applications on the affected area;
- therapeutic baths with mineral waters or sea salt;
- physical therapy: dosed physical activity strengthens muscles and improves blood circulation in them; at an advanced stage of the disease, it is necessary to start with the easiest complex and gradually complicate it.
- classical acupuncture and electroacupuncture: stimulate the work of muscle tissue and nerve fibers;
- classes with an occupational therapist: necessary when it is not possible to fully restore the function of the limb; exercises are aimed at developing new movements adapted to the capabilities of the arm or leg.
For full treatment, a long-term complex effect on the affected area is required. Only if the patient thoroughly fulfills all the doctor’s instructions can success be achieved, but even in this case, full restoration of the functions of the nerve fibers is not guaranteed.
Definition
Radiculopathy is a symptom, not an independent disease, a symptom of a disease of the peripheral nervous system, the cause of which in most cases is protrusion or herniation of the intervertebral disc and arthrosis of the vertebral joints. And before continuing, I would like to start with the anatomy of the spine and the structure of the nervous system.
According to the classification of vertebrae, free vertebrae are distinguished:
- cervical vertebrae – 7 pcs.
- thoracic vertebrae – 12 pcs.
- lumbar vertebrae – 5 pcs.
and fused:
- sacral vertebrae – 5 pcs.
- coccygeal vertebrae – 3-5 pcs.
A distinctive feature of the cervical vertebrae is the presence of an opening in the transverse process - the vertebral arteries pass through it. Another distinctive feature is the atlas and axial vertebrae (1st and 2nd vertebrae), they are atypical, they lack a body, spinous and articular processes. 3 - 7 cervical vertebrae - typical.
In any typical vertebra, the body, arch and process are distinguished, and their connections are distinguished according to the parts of the vertebra.
The vertebral bodies are connected to each other through intervertebral discs, anterior and posterior longitudinal ligaments.
The arches are connected by the ligamentum flavum.
Among the processes, spinous, transverse and articular (upper and lower) are distinguished. The spinous processes are connected by the interspinous ligament, the transverse ones by the intertransverse ligament, and the articular processes by the intervertebral joints.
All vertebrae form the spinal column among themselves, and when the vertebrae connect, intervertebral foramina are formed (right and left), through which spinal nerves and vessels pass.
The spinal column does not occupy a strictly vertical position; it has physiological curves. The curve facing backward is called kyphosis, and the curve facing forward is called lordosis.
The spinal cord located inside the spinal canal begins from the foramen magnum and ends to the first lumbar vertebra (LI) in men, 2 lumbar vertebra (LII) in women.
There are 124 roots extending along the spinal cord. 62 posterior and 62 anterior, from which 31 pairs of spinal nerves are formed.
Having understood the anatomy of the spine and the formation of nerve roots, you can move on to the disease.
All back pain can be divided into specific, nonspecific and radicular.
So, radiculopathy is a disease caused by compression (damage) of a nerve root, causing radicular pain in the back. Compression occurs due to the fact that the intervertebral disc, which performs a shock-absorbing function in the spine, begins to protrude under external loads and a non-functioning muscle corset. Thus forming a protrusion, and subsequently a herniation of the intervertebral disc.
For understanding, here are statistics on the prevalence of back pain:
- specific – 85% (due to muscles, ligaments, tendons, small joints),
- nonspecific – 10% (vertebral fracture, tuberculosis, osteomyelitis, abscess, spinal stenosis, neoplasm, ankylosing spondylitis, etc.)
- radicular up to 4%.
In other words, the prevalence of radiculopathy is 4% of all back pain syndromes.
Complications
If you do not consult a doctor in time and do not eliminate the cause that caused the damage to the nerve fibers, neuropathy will steadily progress. Complications of the disease include:
- a significant decrease in muscle tone with subsequent muscle atrophy;
- loss of limb performance;
- development of extensive trophic ulcers requiring surgical intervention;
- loss of ability to move and self-care;
- chronic insomnia due to pain and the development of restless legs syndrome;
- depression and neuroses.
You can avoid complications if you consult a doctor for help in a timely manner and also follow preventive measures.
Make an appointment
Prevention
Polyneuropathy is a condition that can be effectively prevented long before the first symptoms appear. To do this you need:
- visit a doctor in a timely manner and undergo comprehensive diagnostics in order to promptly identify and eliminate diseases that can cause damage to peripheral nerve fibers;
- eliminate bad habits: smoking and drinking alcohol, prevent toxins from entering the body;
- eat well, include a sufficient amount of macro- and microelements, vitamins in the diet; For the proper functioning of nervous tissue, polyunsaturated fatty acids, which are found in vegetable oils, olives, nuts, and fatty sea fish, are especially important;
- control blood sugar and cholesterol levels;
- provide the body with regular physical activity without striving for records (walking, swimming, cycling, etc.).
Diseases of the peripheral nervous system
Diseases of the peripheral nervous system (neuritis, polyneuritis, neuropathy).
Among the most frequently diagnosed diseases of the human peripheral nervous system, there are several forms of neuritis, cries, neuralgia, as well as all sorts of these pathologies, which have different topography and most often manifest as sharp and sometimes mild pain of a permanent nature. By the way, such a common radiculitis is also a peripheral lesion.
Diseases of the peripheral nervous system are the most common in neurological clinics and account for up to 50% of outpatients. Not presenting, as a rule, a threat to the lives of patients, they are the main cause of disability.
The causes of damage to the peripheral nervous system can be acute and chronic infections, trauma, intoxication, hypovitaminosis, ischemia, hypothermia, compression, and degenerative changes in the spine.
Pathomorphologically, when a peripheral nerve is damaged, swelling and disintegration of the myelin sheath, proliferation of Schwann cells are observed first, and then structural changes occur in the nerve fibers themselves. In this case, vasodilation, exudation, perivascular edema, and hemorrhages are noted in the connective tissue sheaths of the nerve.
If inflammatory phenomena predominate in etiopathogenesis, then peripheral pathology is designated with the ending “it”, if metabolic - then “ia”. If the cause of the disease is degenerative changes in the spine, then the diagnosis is supplemented with the words “vertebrogenic”, “spondylogenic”.
Pathologies of the peripheral nervous system by location
Depending on the location and pathogenesis, the following diseases of the peripheral nervous system are distinguished.
Neuritis (neuropathy)
- a disease in which pathomorphological changes in the nerve are accompanied by disturbances in motor, sensory and autonomic functions. Neuralgia is characterized by attacks of pain along the nerve without signs of organic damage.
This pathology of the peripheral nervous system is caused mainly by metabolic, degenerative processes in the nerve fiber, with minor inflammatory changes in it.
- Polyneuritis
(polyneuropathy) is damage to many nerves. - Plexitis
is a lesion of the nerve plexus. - Ganglionitis
is a lesion of the intervertebral nodes. - Radiculitis
is a lesion of the spinal cord roots. - Radiculoneuritis
is a simultaneous lesion of the spinal cord roots and nerve trunks. - Myeloradiculoneuritis
- damage to the spinal cord, roots and nerve trunks.
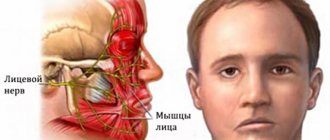
The most common forms of disorders of the peripheral nervous system are vertebrogenic pathology (osteochondrosis), neuritis (neuropathy) and neuralgia. Moreover, the most often affected are those nerves whose trunks pass through narrow bone canals - facial, trigeminal, sciatic.
Peripheral nervous system disorders: facial neuritis
Neuritis of the oculomotor nerve.
The disease is predominantly of vascular, inflammatory, diabetic origin. Observed in intracranial tumors.
Such peripheral neuritis is manifested by drooping of the upper eyelid (ptosis), dilation of the pupil (mydriasis), divergent strabismus and double vision (diplopia).
Treatment
according to the etiology of the disease, vitamin therapy, biostimulants.
Neuropathy (neuritis) of the facial nerve.
Lesions of other cranial nerves are more common.
The cause of the disease can be hypothermia, infection, trauma, inflammation of the ear or meninges, tumors of the base of the skull. Since the trunk of the facial nerve passes through a narrow bone canal and its terminal branches are located superficially, the nerve is easily injured, and during inflammatory processes tissue swelling develops, which leads to compression of the nerve and the vessels that supply it.
This peripheral nerve neuritis develops acutely or subacutely. There are peripheral and central facial palsy.
Peripheral paralysis is characterized by facial asymmetry - the face is skewed towards the healthy side. On the affected side, the skin folds are smoothed, the eye does not close (lagophthalmos), when trying to close the eye, the eyeball turns up (Bell's sign), food gets stuck behind the cheek, teeth are grinned more in the healthy direction. Dry eyes or watery eyes, disturbances in hearing, taste and salivation may occur.
With central paralysis, only smoothness of the nasolabial fold and drooping of the corner of the mouth are observed.
A complication of this disease of the peripheral nerves can be persistent contracture of the affected muscles and tonic muscle spasm - facial hemispasm.
Diagnostics
is based on clinical data and to clarify the diagnosis, an LOP examination, skull radiography, and computed tomography are sometimes performed.
Treatment
This disease of the peripheral nervous system must begin early and correspond to the cause of the lesion. For infectious-inflammatory origin, salicylates, methenamine, indomethacin, acyclovir, and prednisolone are prescribed.
In parallel with the etiological treatment, vasodilators are prescribed: dibazol, aminophylline, trental, nicotinic acid, decongestants (Lasix, furosemide, hypothiazide), vitamins
From 5-7 days of illness, thermal procedures (UHF, paraffin, ozokerite) are prescribed.
In the recovery period, prozerin, aloe, FiBS, ultrasound with hydrocortisone are used on the mastoid process and the affected half of the face, electrical stimulation of the facial muscles, exercise therapy, acupuncture massage, and acupuncture.
If there is no effect within 12 months, they resort to neurosurgical intervention.
Care consists of instilling moisturizing eye drops and wearing glasses during the day. At night, apply eye ointment and cover your eyes with a bandage.
Prevention:
avoid hypothermia, anti-epidemic measures.
Neuritis of the peripheral nerves of the extremities: symptoms and treatment of neuropathies
Neuropathies of the peripheral nerves of the extremities are most often caused by external trauma or compression of the nerve trunk. It is possible that the nerve in the bone canal may be pinched, compressed in deep sleep, when throwing back the arm, during prolonged anesthesia, or when applying a tourniquet. Also, the cause of neuritis can be infections, ischemia, and intoxication.
Radial nerve neuropathy.
It manifests itself as a symptom of a “dangling hand,” while the patient cannot straighten the arm at the wrist and elbow joints, cannot abduct the thumb and supinate the palm, the carporadial reflex decreases, and sensitivity on the dorsal surface of the 1st, 2nd, and 3rd fingers is impaired.
Ulnar nerve neuropathy is characterized by a “bird’s foot” deformity of the hand as a result of paralysis and atrophy of the small muscles of the hand; violation of adduction and abduction of fingers; pain and decreased sensitivity on the 5th and 4th fingers.
Median nerve neuropathy.
It manifests itself as a violation of flexion of the hand and fingers in the interphalangeal joints, opposition of the thumb; impaired sensitivity on the lateral surface of the palm and 1-4 fingers. Also symptoms of such peripheral neuropathy are atrophy of the muscles of the forearm and flattening of the palm like a “monkey’s paw”. The patient cannot clench his fingers into a fist. Characterized by severe pain with a causal tinge and pronounced vegetative-vascular and trophic disorders (hyperhidrosis, hyperkeratosis, brittle nails, atrophy and cyanosis of the skin).
Neuropathy of the external cutaneous nerve of the thigh (Roth disease)
. Occurs as a result of infection, intoxication (alcohol, nicotine, diabetes), atherosclerosis, and long-term nerve injury. This peripheral nerve neuropathy manifests as paresthesia and pain along the outer thigh. The pain is worse at night and especially in an upright position and when walking. Hyper- or hypoesthesia is determined along the outer surface of the thigh.
Neuropathy (neuritis) of the peroneal nerve.
It is characterized by drooping of the foot and the inability to straighten it and the toes. The patient cannot stand on his heel. The muscles of the anterior surface of the lower leg atrophy. Sensitivity on the outer surface of the lower leg and the dorsum of the foot is impaired. The gait becomes step-like, “cock-like.”
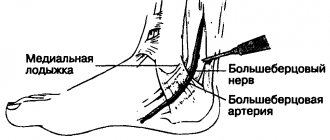
Neuropathy (neuritis) of the tibial nerve.
Leads to impaired flexion of the foot and fingers. The patient cannot stand on his toes. The muscles of the back of the lower leg atrophy, and the Achilles reflex fades. Sensitivity disturbances are noted along the back surface of the lower leg and sole; severe pain and vegetative-trophic disorders.
Treatment
peripheral neuropathy of the extremities includes the use of vitamins B, C, nicotinic acid, aloe extract, proserin, and, if necessary, analgesics.
Physiotherapy is widely used:
- UHF
- Ural Federal District
- Electrophoresis
- Ultrasound
- Laser and magnetic therapy
- Massage
- Exercise therapy
Care consists of preventing persistent paresis and contractures (suspension, bandages, splints for fixing the limb, orthopedic shoes), teaching the patient the elements of therapeutic exercises. If there is no recovery within two months, surgery is indicated.
Lesions of peripheral nerves: neuralgia
Trigeminal neuralgia.
A disease of peripheral nerves with severe pain and a relapsing course.
The cause may be infections, intoxications, atherosclerosis, hypothermia, pathological processes at the base of the skull, in the paranasal sinuses, teeth, orbits, and narrowing of the bone openings.
The main symptom of this disease of the peripheral system
- attacks of sharp shooting pain in the zone of innervation of one or more branches of the nerve. The pain lasts a few seconds, less often - minutes. Pain is provoked by excitement, chewing, talking, touching the tongue to sensitive points (triggers) of the mucous membrane of the mouth and gums. Therefore, patients may develop obsessive fear, and in order not to provoke an attack, they freeze, hold their breath, and are afraid to make the slightest movement. Attacks may be accompanied by redness of half the face, cramps of facial muscles, lacrimation, and copious nasal discharge. During the interictal period, one can detect hyperesthesia in the area of the affected branch and pain at the point of its exit.
When the trigeminal nerve ganglion is damaged, constant burning pain and herpetic rashes are observed. Herpetic keratitis is especially dangerous when the first branch of the nerve is affected.
Treatment
primarily aimed at eliminating the cause of the disease.
Next, analgesic and anti-inflammatory drugs are prescribed (analgin, sedalgin, reopirin, indomethacin, pentalgin):
To suppress neuralgic paroxysms, carbamazepine (finlepsin), trimethin, convulex clonazepam, neurontin, lamictal are used:
They also stimulate metabolic processes (retabolil, solcoseryl, actovegin, B vitamins): Baclofen is also used: For herpetic rashes, acyclovir, herpesin are prescribed:
Physiotherapy includes UHF, ultraviolet irradiation, diadynamic currents, SMT, novocaine electrophoresis, laser therapy..
Care
consists in creating a protective regime, preventing the patient from hypothermia and feeding him non-hot, well-purified food.
Neuralgia of the pterygopalatine ganglion (Slader syndrome).
The disease is caused by the same reasons as trigeminal neuralgia. Symptoms of this disease of the peripheral nervous system are attacks of pain in the eye, root of the nose, jaw, teeth spreading to the tongue, soft palate, ear, and cervicohumeral area. Sometimes the pain covers half of the head, noise, dizziness, and ringing in the ear appear. At the same time, half of the face turns red, tearing and salivation intensify. The attack lasts up to one hour.
Treatment and care
are carried out according to the same scheme as for trigeminal neuralgia. As a local therapy, the middle nasal passage is lubricated with novocaine.
Neuralgia of the glossopharyngeal nerve.
Occurs more often in older people. Causes: atherosclerosis, tumors, scars, osteophytes. This disorder of the peripheral system is characterized by attacks of severe pain in the root of the tongue, tonsils, radiating to the ear, eye, and neck. In this case, the patient experiences dry mouth, cough, and excessive salivation.
Treatment
carried out as with trigeminal neuralgia; locally - lubricating the root of the tongue with cocaine.
Neuralgia of the occipital nerve.
Caused by hypothermia, infections, degenerative processes in the spine, arachnoiditis and tumors of the posterior cranial fossa. The disease is characterized by attacks of pain in one half of the back of the head, radiating to the ear, neck, shoulder girdle, and shoulder blade. The pain intensifies with movement, coughing, sneezing. Possible forced head position. With this disorder of a peripheral nature, pain in the nerve exit points and sensitivity disorders in the occipital area are noted.
Treatment
underlying disease, pain medications, vasodilators, vitamins, locally - UV irradiation, UHF.
Intercostal neuralgia.
It can be primary and secondary, i.e. arising against the background of other diseases, especially with pathology of the spine (osteochondrosis, tumors, tuberculosis) and internal organs (lungs, pleura, liver).
The disease is characterized by girdling, shooting pains spreading from the spine along the intercostal spaces around the chest. The pain intensifies with movements and deep breaths. There are sensitivity disorders in the area of innervation of the intercostal nerves, pain in the paravertebral and intercostal points. Loss of abdominal reflexes and paresis of the abdominal muscles are possible. When the intervertebral ganglion is involved in the process, symptoms of herpes zoster appear. To clarify the diagnosis, a thorough examination of the patient is necessary in order to exclude the secondary nature of neuralgia.
Treatment includes eliminating the cause of the disease, painkillers (analgin, baralgin, diclofenac, indomethacin):
Anticonvulsants (finlepsin, 0.2 g 1-2 times a day):
Vitamins, physiotherapy (UHF, DDT),
Care
provides for the creation of a gentle regime, the choice of a comfortable position, and the prevention of hypothermia.
Shingles (ganglionitis, herpetic intercostal neuralgia).
The disease is caused by the neurotropic herpes zoster virus and is provoked by hypothermia. In the spinal nodes and their cranial analogues, an inflammatory process develops, spreading to the nerves and roots.
The disease begins with general malaise, fever and pain in the area of innervation of the affected ganglion (most often in the thoracic region). After 2-3 days, redness and rashes of very painful blisters filled with serous fluid appear at the site of pain. The vesicles often fester, forming pustules that become covered with a crust that falls off after a few days.
When the gasserian node is damaged, rashes appear on the skin of the forehead, upper eyelid, bridge of the nose and on the membranes of the eye, which can result in keratitis and blindness.
Some patients who have had herpes zoster experience pain for a long time (postherpetic neuralgia) and relapses are possible.
Treatment includes antiviral drugs (acyclovir 0.8 x 3, retrovir 0.25 x 5, valacyclovir), detoxification (hemodez), dehydration (furosemide), chimes, analgesics (azafen 0.025 x 6, pyrazidol 0.05 x 3, mexiletine , finlepsin, amitriptyline, herpesin):
Tebrofen ointment, gassipol, and ultraviolet radiation are used topically.
Polyneuritis and polyneuropathy of peripheral nerves
Polyneuritis
- multiple lesions of peripheral nerves of infectious origin.
Polyneuropathy
- toxic damage to the nerves as a result of intoxication of the body, metabolic disorders, allergic reactions, circulatory disorders. If, along with the nerves, their radicular part is affected, then polyradiculoneuritis is determined.
Anatomically, with polyradiculoneuritis, inflammatory changes (edema, hyperemia, infiltration) of the roots are determined, and signs of myelin decay and degeneration of the axial cylinders are visible in the peripheral nerves. Moreover, if the pathological process is limited to mesenchial formations of the membranes and vessels, then this is interstitial neuritis. If it is accompanied by damage to nerve fibers (demyelination, disintegration of axial cylinders), then it is interstitial-parenchymal neuritis. With polyneuropathies, degenerative changes in nerves occur with a predominance of decay of their myelin sheaths or nerve fibers.
Polyneuritis and polyneuropathy are manifested by pain and paresthesia in the distal parts of the extremities, peripheral paralysis, sensitivity disorders of the “glove” and “sock” type and vegetative-trophic disorders (dryness, thinning of the skin or its hyperkeratosis, cyanosis, trophic ulcers).
Infectious polyneuritis of viral etiology is characterized by an acute onset with general malaise, fever, pain and paresthesia in the extremities.
Subsequently, weakness, atrophy, paralysis of the muscles of the arms and legs, and sensory disturbances develop. The nerve trunks are sharply painful on palpation. Reversal of symptoms is slow.
Treatment includes antiviral drugs, antibiotics, analgesics, corticosteroids, vitamins, and biostimulants.
Acute infectious polyradiculoneuritis usually occurs in the cold season and begins acutely with a rise in temperature, catarrhal symptoms, pain and paresthesia in the distal extremities. Sensitivity disorders of the peripheral type, pain in the nerve trunks, tension symptoms, distal paralysis and vegetative-vascular disorders are determined.
One of the most common forms of multiple lesions of the nervous system is acute infectious Guillain-Barré polyradiculoneuritis. The disease begins acutely with a rise in temperature and catarrhal symptoms, usually in the cold season. Patients develop rapidly increasing weakness in the legs, difficulty walking, and pain along the nerve trunks.
Characterized by symmetrical flaccid paralysis, starting from the lower extremities and covering the muscles of the trunk, upper extremities, neck, lesions of the cranial nerves, sensitivity disorders and sharp protein cell dissociation in the cerebrospinal fluid. The course of this form of the disease is benign.
Another type of polyradiculoneuritis is ascending Landry's palsy.
, in which the anterior roots are predominantly affected. Characterized by an acute onset and rapid course of the disease. The disease begins with paresthesia, pain, weakness, and paralysis of the legs, which quickly, within 2-3 days, spread to the upper limbs and cranial nerves, primarily the bulbar ones. In this case, speech and swallowing are impaired, breathing and cardiac problems occur. Death is common.
Treatment consists of suppressing the autoimmune inflammatory reaction (prednisolone, or its analogues, intravenous bolus up to 1.5-2.1 g per day for the first 3 days, followed by a dose reduction and switching to tablet drugs), administration of antibiotics (benzylpenicillin up to 20 million units per day, gentamicin, rifampicin) and hexamethylenetetramine: Reducing pain (analgin, voltaren): Detoxification (hemodez, glucose): Improving neuromuscular transmission (prozerin intramuscularly 1-2 ml twice a day, galantamine, ATP, B vitamins) :Immunoglobulin and plasmapheresis are also used:
If swallowing is impaired, glucose, albumin, and hydrolysine are administered intravenously; If breathing is impaired, resuscitation measures are carried out. After the acute phenomena subside, ultraviolet irradiation, UHF sessions, light massage, passive movements are carried out, biostimulants and vitamins are administered. 2-3 months after the process has subsided, hydrogen sulfide and radon baths, mud applications, and exercise therapy can be prescribed. Diphtheria polyneuritis occurs two to three weeks after diphtheria. It mainly affects the cranial nerves - the vagus, facial and abducens. The appearance of bulbar disorders is especially dangerous. After recovery, the voice may remain deaf for many years. Treatment is carried out by urgent administration of anti-diphtheria serum (5-10 thousand units). To prevent an anaphylactic reaction, 0.5-1.0 ml of serum is first injected under the skin, and after 12-24 hours the entire dose is injected.
Allergic (anti-rabies) polyneuritis
is a consequence of an allergic reaction to the vaccine. After the start of vaccinations, the patient develops dizziness, weakness, dyspepsia, and diffuse pain. Then the temperature rises; vomiting, uncontrollable, severe headache appear, flaccid paralysis of the limbs and pelvic disorders develop. Reversal of symptoms is rapid.
Diabetic polyneuropathy develops against the background of hyperglycemia.
It is characterized by paresthesia, itching and pain in the legs, sensitivity disorders in the distal extremities, and extinction of the Achilles and knee reflexes. Possible damage to the oculomotor nerves and autonomic ganglia.
Treatment includes correction of hyperglycemia (diabetes, insulin), vitamins, trental, coplamine, nootropics, analgesics, biostimulants, anabolic steroids, lipostabils, thioctacid:
Alcoholic polyneuropathy
develops subacutely with chronic alcohol intoxication. The disease begins with paresthesia, burning pain in the feet against the background of pronounced autonomic disorders (cyanosis, coldness, sweating) of the extremities.
In the distal sections, paresis develops, superficial and deep sensitivity is impaired (sensitive ataxia), and muscle atrophy appears. Korsakov's syndrome is very characteristic - loss of memory for recent and current events, confabulation, temporal and spatial disorganization.
Treatment consists of eliminating alcohol, prescribing large doses of B vitamins, benfogamma, mil-gamma, vasodilators (spasvin) and other drugs used for polyneuropathies.
Polyneuropathy in pregnant women is associated with impaired vitamin metabolism and liver failure. Characterized by paresis, peripheral sensitivity disorders, extinction of reflexes, disorders of autonomic innervation in the form of hyperhidrosis, coldness of the extremities. Possible Landry syndrome.
Lesions of the peripheral nervous system: plexitis
Cervical plexitis
Caused by infections, tumors, tuberculosis and injuries to the cervical spine. It manifests itself as pain and sensory disturbances in the back of the head, ear, neck, upper scapula and shoulder. Disturbances in the function of the phrenic nerve are characteristic (breathing problems, hiccups, complete or partial immobility of the diaphragm).
Brachial plexitis
occurs after shoulder injuries, collarbone fractures, infections, pathologies of the spine and lungs. Depending on the location of the lesion, upper, lower and total brachial plexitis are distinguished.
Upper (Duchenne-Erb palsy)
manifested by pain in the upper third of the shoulder, decreased reflex with the biceps, difficulty in shoulder abduction, supination, flexion of the arm at the elbow joint, as well as impaired sensitivity on the outer surface of the shoulder and forearm.
Lower (Dejerine-Klumpke palsy)
characterized by pain and sensitivity disorders on the inner surface of the shoulder and forearm, paresis and atrophy of the muscles of the hand and forearm, and a decrease in the carporadial reflex. Possible Horner-Bernard syndrome.
Total plexitis
is rare, characterized by pain in the supra- and subclavian region, radiating to the arm, loss of reflex
c, paresis and sensory impairment in the entire arm, severe vegetative-vascular disorders.
Lumbosacral plexitis
occurs as a result of infections, intoxications, diseases of the pelvic and abdominal organs, during pregnancy, during pathological childbirth and injuries to the spine and pelvic bones. Clinically, plexitis is manifested by pain and loss of sensitivity in the buttock, thigh and lower leg, loss of the knee and Achilles reflexes, paresis of the foot and atrophy of the muscles of the buttocks and thighs.
Treatment is similar to that of polyneuropathy.
« Back to previous page
Treatment at the Energy of Health clinic
Neurologists at the Energy of Health clinic will provide assistance with any form of polyneuropathy. Specialists will conduct a full diagnosis to accurately identify the extent and location of the lesion, and then prescribe treatment and rehabilitation in accordance with the individual characteristics of the body. We use comprehensive methods that include:
- drug therapy in accordance with indications and modern recommendations for the treatment of polyneuropathy, including courses of infusions;
- various types of physiotherapy: magnetic therapy, laser and ultrasound exposure, phonophoresis and electrophoresis;
- physical therapy under the supervision of an experienced instructor, training in exercises to restore limb function at home;
- massotherapy;
- sessions with a psychotherapist if you have depression, insomnia, or increased anxiety;
- organization of sanatorium-resort treatment for complete rehabilitation.
Advantages of our clinic
The multidisciplinary clinic “Energy of Health” has experienced staff and the most modern equipment for diagnosing and treating various diseases. We provide each client with high quality medical services, which include:
- detailed examination to accurately determine the cause of complaints;
- consultations with narrow specialists directly in the clinic, as well as communication with foreign doctors if necessary;
- comprehensive treatment, selected in accordance with the indications and individual characteristics of the body;
- minor surgical operations directly in the clinic;
- own day hospital for maximum convenience;
- drawing up rehabilitation programs;
- affordable prices and services within the framework of voluntary health insurance.
Polyneuropathy is a dangerous complication of many conditions and diseases. You should not hope that the symptoms are limited to a simple tingling sensation; over time, the condition will worsen. Don’t delay seeing a doctor; sign up for a consultation with neurologists at the Energy of Health clinic.
Symptomatic treatment of polyneuropathy
Pain syndrome is an integral sign of polyneuropathy. Nonsteroidal anti-inflammatory drugs and analgesics do not significantly reduce pain. More effective pain relievers are the opioid analgesics tramadol and oxycodone. For local anesthesia, local anesthetics (Versatis, lidocaine) and irritating drugs (capsaicin) are used.
Comprehensive treatment of pain in polyneuropathy includes the use of anticonvulsants (tebantine, pregabalin) and antidepressants (amitriptyline, Cymbalta). If these drugs do not relieve pain, neurologists use a combination of several drugs.
In addition to drug treatment methods, rehabilitation therapists use innovative methods of restorative therapy. The staff of the neurology clinic professionally performs all manipulations and is attentive to the wishes of the patients. In order to undergo treatment for polyneuropathy with modern medications at affordable prices, make an appointment with a neurologist by calling the Yusupov Hospital.