It is a neurological disease in which the activity of many peripheral nerves is disrupted at the same time.
Occurs in people who abuse alcohol. It appears during the second and third stages of alcoholism, when a person abuses heavily and can no longer hide his illness from others. The cause of the onset and development of the disease may be the toxic effect of ethanol on the nervous system and a disruption of the metabolic process in it.
What is this
Alcoholic polyneuropathy is a neurological disease caused by alcohol damage to nerve fibers and manifested by impaired sensitivity, movement and pain in the extremities (arms and legs). If left untreated, it leads to irreversible changes in the limbs and disability.
Seen by EVERYONE! alcohol abusers. But only no more than 30% of all sick patients turn to doctors with complaints of impaired sensitivity and gait.
Classification
Alcoholic polyneuropathy has several clinical variants.
The following forms are distinguished along the flow:
- spicy;
- subacute;
- chronic.
Acute is provoked by binge drinking or hypothermia. Against this background, symptoms manifest quickly and, without treatment, become latent, or a protracted version with erased manifestations.
The chronic form develops in 4 stages:
- Zero. It is possible to identify changes indicating the onset of a disease process only through studies using a special diagnostic device - an electromyograph. Positive data from quantitative and sensory testing also support the development of pathology. The patient does not make any complaints.
- The first (initial manifestations). The patient experiences periodic, mild symptoms of polyneuritis.
- The second (with classic, clinically significant signs). For diagnosis, existing complaints and medical examination data are quite sufficient. There are no functional defects.
- Third (with severe symptoms). Patients who are sick partially or completely lose their ability to work and become disabled.
Symptoms
The very first signs of this disease are decreased sensitivity in the feet and legs. But patients usually do not pay attention to this. Later, the first unpleasant sensations appear - paresthesia in the legs or arms. In some cases, pain occurs in the legs, which intensifies with pressure on the muscles. When gross and irreversible destructive processes already occur in the nerve fibers, weakness in the legs, gait disturbances, and paralysis of the lower and upper extremities appear. The muscles begin to atrophy (decrease in size). In addition, changes in the skin are added: increased sweating, swelling, changes in color and skin turgor. In severe and long-term cases, decreased and loss of vision, cardiovascular, respiratory and gastrointestinal disorders are observed.
Diagnostic methods
It will be quite difficult to initially make a correct diagnosis, because the symptoms of polyneuropathy are similar to other diseases. And making a diagnosis by listening to the patient’s complaints is almost impossible, because it is necessary to undergo a whole series of laboratory tests.
First of all, you need to thoroughly consult with a neurologist so that the specialist examines the limbs that are affected, and he also needs to check the patient’s reflexes.
When there is already an approximate suspicion of polyneuropathy, then it will be necessary to conduct a general blood test, do an electroneuromyography, and in very rare cases a nerve biopsy will be needed.
ENMG will make it possible to find out about nerve damage, a differential diagnosis of other diseases will be made, and it will be possible to determine the prognosis of this disease. And then ENMG will allow you to track the dynamics of changes in the nerves against the background of the rest of the treatment.
The next stage is the laboratory methods of the entire study, namely screening laboratory tests. In other cases, there is a need to consult an endocrinologist, as well as do other research.
Treatment
A prerequisite for treatment is to stop drinking alcohol. As a rule, this becomes possible only when the patient begins treatment for alcohol dependence. In most cases, such treatment begins in a specialized 24-hour hospital.
Treatment methods for alcoholic polyneuropathy:
- Treatment of alcohol addiction.
- Vitamin therapy. B vitamins, ascorbic and nicotinic acid allow you to restore nerve cells and nerve fibers that have not yet died.
- Metabolic, neurometabolic therapy restores metabolism inside cells, improves the absorption of glucose and oxygen.
- Vascular therapy helps improve blood supply to all tissues of the body.
- Physiotherapy.
- Biofeedback therapy.
- Diet therapy.
- Exercise therapy, massage, occupational therapy.
Treatment of alcoholic neuropathy consists of two stages: active therapy in a hospital, lasting from 10 to 45 days; and rehabilitation (at home or in a specialized rehabilitation center) lasts from 1 to 12 months.
Causes of alcoholic polyneuropathy
The disease is provoked by alcohol intoxication and the associated toxic effect on peripheral nerves, their damage, and metabolic disorders. There are several additional factors that cause alcoholic polyneuropathy:
- "dietary". Unbalanced, poor nutrition often accompanies alcohol addiction. The diet contains an excess of carbohydrates and a lack of vitamins. Deficiency of folic acid, thiamine, and other B vitamins slows down the utilization of ethyl alcohol and its breakdown products, which increases the toxic effect of alcohol;
- oxidative stress. With constant consumption of alcohol, excessive formation of free oxygen radicals occurs, and the activity of antioxidants decreases. The balance of pro-oxidant and antioxidant systems shifts, which causes disturbances in the activity of cellular structures, and, in particular, in the work of endothelial cells (“responsible” for the metabolic support of the brain, regeneration, tissue growth, and perform barrier functions). A decrease in endothelial activity provokes endoneurial hypoxia, against which neuropathy appears;
- direct damage to the peripheral nervous system. Occurs under the influence of alcohol and ethyl alcohol metabolites. Acetaldehyde destroys the barrier protection of the nervous system and damages the nerve fiber.
Clinical and anatomical conference
Alcoholic polyvisceropathy
Authors of the article: Doctor of Medical Sciences, Prof. Vertkin A. L., Ph.D., Associate Professor Nosova A.V., ass. Sycheva A.S., Ursta E.M.
Clinical example:
Patient Zh., 70 years old, was hospitalized at the City Clinical Hospital named after. Spasokukotsky on August 29, 2019 through the emergency medical service with a referral diagnosis: “Atrial fibrillation (more than 48 hours)”
.
Length of hospital stay: 23 hours
.
Upon admission, the patient complained of rapidly progressing shortness of breath
with minimal physical exertion and in a horizontal position until suffocation during the last two days.
From the medical history: long history of alcohol
(vodka), last episode of alcohol consumption during the week preceding hospitalization, denies alcohol consumption for the last 2 days.
At the same time, the above-described shortness of breath appeared and began to increase, and therefore
an ambulance team was called (ECG: paroxysm of atrial fibrillation). Hospitalized in the cardiac intensive care unit.
From the life history: long history of hypertension
with maximum figures of blood pressure = 200/100 mm Hg.
Art., adapted to the figures of blood pressure = 140/80 mm Hg. Art. For this disease he takes Cordaflex
.
Several years of paroxysmal atrial fibrillation, the date of the last paroxysm is unknown. They talked about a myocardial infarction
. ONMK, SD denies. Extirpation of the uterus for fibroids in 1991.
Objectively: the condition is serious
.
The skin and mucous membranes are pale
.
Breathing is spontaneous, regular, dullness
of percussion sound in the lower parts,
moist
fine
rales
.
Heart sounds are muffled, the rhythm is correct. Blood pressure
= 215/100 mm Hg.
Art. Heart rate
= 120/min.
ECG tachycardia
, no focal changes. The abdomen is soft, painless in all parts. Urination is not changed.
According to ECG data (Figure 1, 2) from the ambulance team: the rhythm of atrial fibrillation
with heart rate = 120, EOS is located normally, McGean-White sign (
S 1 Q 3 T 3
)
S 1 Q 3 T 3
may also characterize not only
acute cor pulmonale
, BUT also be observed in individuals
with a bradymorphic body type (obese individuals)
due to the “lying” position of the heart on the diaphragm -
differentiated
by taking
an ECG on a deep breath
(with a “lying” position of the heart, the changes will disappear ).
According to Rg OGK data (Figure 3) dated 08/29/2019: Phenomena of venous stagnation in the ICC
.
Incipient pulmonary edema
?
According to ECHO-KG data dated August 20, 2019: LVEF
= 51.7%.
Concentric hypertrophy of the LV myocardium. Paradoxical
movement of the IVS.
Slight effusion in the pericardial cavity. Significant pulmonary hypertension
.
According to laboratory data upon admission:
Clinical blood test: WBC = 11.4*109/l ( leukocytosis
), lymphocytes = 6.7% (relative lymphopenia),
ESR
= 23 mm/hour.
Biochemical blood test: total bilirubin
= 42.1 µmol/l.
Diagnosed by the ICU doctor:
BASIC:
IHD: post-infarction cardiosclerosis (n/a)
BACKGROUND.:
Hypertension stage III, hypertension stage 3, very high risk of cardiovascular complications. Obesity 2 tbsp.
O.S.:
Hypertensive crisis from 08/29/2019. Paroxysmal form of atrial fibrillation with restoration of sinus rhythm at the prehospital stage. NK 2B art. Acute decompensation of CHF. Recurrent cardiac asthma.
SOP:
Chronic cerebral ischemia. Extirpation of the uterus for fibroids in 1991.
Therapy prescribed:
- "Bisoprolol" 5 mg 1 time/day;
- “Losartan” 50 mg 1 time/day;
- "Moxonidine" 0.4 mg;
- "Fraxiparin" 0.4 ml;
- Furosemide 60 mg;
- "Omeprazole" 20 mg.
08/30/2019: the patient experienced cardiac arrest. There is an isoline on the ECG monitor, blood pressure is not determined, there is no pulsation in the great vessels. Resuscitation measures are ineffective, biological death is diagnosed.
Post-mortem diagnosis:
BASIC:
IHD: post-infarction cardiosclerosis (n/a)
BACKGROUND.:
Hypertension stage III, hypertension stage 3, very high risk of cardiovascular complications. Obesity 2 tbsp.
O.S.:
Paroxysmal form of atrial fibrillation. NK 2B art. TELA. Brain swelling. Pulmonary edema.
SOP:
Chronic cerebral ischemia. Extirpation of the uterus for fibroids in 1991.
Key clinical positions:
- Elderly woman;
- Alcohol history;
- Atrial fibrillation;
- CHF;
- Hypertonic disease;
- Hypertensive crisis.
Key laboratory and instrumental positions:
- ECG: LVT; paroxysm of atrial fibrillation;
- Echocardiography: concentric LV hypertrophy; LA volume index more than 41 ml/m2;
- D-dimer;
- Billirubin.
Differential diagnosis:
- With AMI: chest pain, changes in ECG data (elevation); increased levels of Troponin I (other forms of AMI due to anemia, for example, this is rare);
- Gastrointestinal tract: no anemia according to the blood test; no liver cirrhosis with signs of portal hypertension;
- Alcoholic cardiomyopathy (no key sign: dilatation of the heart cavities);
Autopsy data:
Pathological diagnosis:
BASIC:
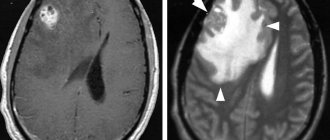
Hematoma-type hemorrhage in the temporoparietal region of the right hemisphere of the brain (fibrous plaques that stenose the lumen up to 50%)
BACKGROUND.:
Arterial hypertension: concentric myocardial hypertrophy (wall thickness of the left ventricle - 1.8 cm; right - 0.3 cm; heart weight - 510 g), arteriolosclerotic nephrosclerosis. Obesity 2 tbsp. (BMI = 36.39)
O.S.:
Edema of the brain with herniation of the cerebellar tonsils into the foramen magnum. Acute and chronic venous congestion of internal organs: brown induration of the kidneys and spleen, “nutmeg” liver
SOP:
Diffuse small-focal cardiosclerosis. Atherosclerosis of the coronary arteries of the heart (plaques in the stage of calcification, narrowing the lumen of the arteries to 50%), aorta (fibrous plaques with ulcerations, calcification). COPD: peribronchial pneumosclerosis. Fatty hepatosis. Condition after long-term hysterectomy.
Divergence of diagnoses:
In this clinical case, there is a discrepancy in diagnoses in category I.
The reasons for the discrepancy in diagnoses in this clinical case:
- Short stay;
- Lack of consultation with a neurologist if indicated (episode of psychomotor agitation in the patient, clinical signs of focal brain damage);
- Lack of head CT as the main diagnostic method for diagnosing stroke.
Stroke:
This patient has:
- Obesity 2 degrees;
- Hypertension stage III;
- Post-infarction cardiosclerosis, atrial fibrillation;
- Physical inactivity;
- Alcohol abuse.
Factors that provoke the development of hemorrhagic stroke:
- Arterial hypertension (especially hypertensive crisis: upon admission, the patient’s blood pressure = 215/100 mm Hg);
- Alcohol abuse (the patient had binges for 4 days).
The outcome of ischemic stroke can also be hemorrhage
according to the type of diapedesis due to ischemia of the vascular wall and an increase in its permeability.
The patient had an episode of psychomotor agitation and an increase in cerebral hypoxia: indications for consultation with a neurologist.
Instrumental confirmation of stroke: CT scan of the brain
.
Recommendations from the RPO “Outpatient Doctor”:
- Systematization of complaints;
- According to the set of complaints by system, determine the diseases that occur in this patient;
- Compare the identified diseases with a table of the main causes of death according to gender and age;
Chronic form of IHD:
- Post-infarction cardiosclerosis;
- Ischemic cardiomyopathy;
- Chronic cardiac aneurysm.
Mechanisms of death:
- Death due to ventricular fibrillation (typical of AMI);
- Death through asystole.
alcoholic polyvisceropathy occurs in 84% of cases
, 75% of cases had hypertension, 48% had benign prostatic hyperplasia, 33% had COPD, 29% of cases had diabetes, 24% had gastric and duodenal ulcers, 21% had obesity, 9% had malignant neoplasms.
Alcohol intoxication – there is no such concept in modern medicine!!!
A patient who abuses alcohol smells of alcohol = ACUTE POISONING WITH ETHANOL AND ITS SURROGATES (this diagnosis is in the ICD)
.
WHO criteria for harmful use of alcohol and drunkenness:
Drinking alcoholic beverages at a rate of more than 40 g of pure alcohol per day for a man and 30 g for a woman is considered harmful.
Harmful use pattern: consumption of at least 60 grams of pure alcohol per episode at least once a month over the past 12 months.
Alcohol abuse – 60 grams or more of pure alcohol at least once every week.
Withdrawal syndrome = no smell from alcohol abuse
.
Bibliography:
- Materials of the Regional Public Organization “Outpatient Doctor”: Clinical and anatomical conference. Broadcast from July 10, 2021 https://www.youtube.com/watch?v=2_CIFMqCWfY&feature=youtu.be
- Autopsy materials from the State Budgetary Healthcare Institution “GKB IM. S.I. SPASOKUKOTSKY DZM";
- European Action Plan to reduce the harmful use of alcohol 2012–2020. World Health Organization, Geneva, 2013. https://www.euro.who.int/__data/assets/pdf_file/0008/187154/e96726R.pdf
- ESC CLINICAL GUIDELINES FOR THE TREATMENT OF PATIENTS WITH Atrial Fibrillation, developed jointly with EACTS, 2021 https://scardio.ru/content/Guidelines/2516-6313-1-SM.pdf
Physiotherapy
It helps restore muscle tone, improve nerve tissue conductivity and normalize sensitivity. To achieve this result, physiotherapeutic procedures are prescribed. They can be selected by the doctor strictly individually . Their choice is influenced by the duration of the disease and the severity of damage to the nervous tissue. Treatments include exercise therapy, acupuncture and massage.
After the course of treatment, the patient requires a comprehensive rehabilitation program. It includes:
- corrective rehabilitation procedures,
- moderate physical activity,
- taking medications,
- exercises aimed at training intellectual abilities,
- a balanced diet.
But the most important requirement for a recovering person is a complete abstinence from alcohol after the end of treatment.
Literature:
- Alcoholic polyneuropathy (polyneuritis) and its reversibility during detoxification treatment: Abstract of thesis. for the degree of Candidate of Medical Sciences. (14.0013) / Orenburg. state honey. int. - Orenburg, 1974. - 18 p.
- Diagnosis and treatment of early manifestations of damage to the nervous system in alcohol abusers: dissertation ... candidate of medical sciences: 01/14/11 / Kurashevich Ksenia Georgievna; [Place of protection: First St. Petersburg. state honey. University named after I.P. Pavlova]. — St. Petersburg, 2021.
- Alcoholic polyneuropathy / A. A. Yarosh, T. I. Ilyash. - Kyiv: Zdorov, I, 1986. - 37 p.
The text was checked by expert doctors: Head of the socio-psychological service of the Alkoklinik MC, psychologist Yu.P. Baranova, L.A. Serova, a psychiatrist-narcologist.
CAN'T FIND THE ANSWER?
Consult a specialist
Or call: +7 (495) 798-30-80
Call! We work around the clock!