general information
According to statistics, at least every tenth person on the planet suffers from migraine.
Women get sick approximately twice as often as men. This is associated with cyclical hormonal changes during the menstrual cycle. Typically, the disease makes itself felt before the age of 30-35; cases of the pathology occurring in childhood have also been described.
The biomechanism of the development of the disease is not precisely known. There are several theories about the occurrence of pain and accompanying symptoms, the most popular of which is neurovascular. According to this point of view, migraine begins against the background of activation of the trigeminal nucleus, which first causes spasm and then dilation of cerebral vessels. As a result, the tissue around the arteries becomes swollen, which leads to pain. In addition, the pathological process is associated with impaired serotonin metabolism.
Some scientists believe that pain occurs solely against the background of a sharp spasm and subsequent relaxation of blood vessels, resulting in tissue swelling (vascular theory). It has been clearly proven that the risk of developing the disease is significantly higher in women, as well as in people whose parents or close relatives also suffered from migraine.
Make an appointment
What are the characteristics of migraine with aura?
About 20% of patients experience an aura. But only a few say that it occurs with every attack. The most common symptom of an aura is visual disturbances. Less commonly – sensory organ disorders (tingling, numbness, goosebumps). Aura symptoms are divided into positive and negative. In the first case, something is felt, and in the second, the fields of vision disappear or the hands go numb. Another property of the aura is dynamism. That is, a gradual increase in symptoms, and then their gradual decline. Usually the aura is replaced by a headache, but sometimes the aura appears on its own.
Migraine with aura is characterized by the following symptoms:
- Two episodes of migraine without aura.
- The presence of an aura for 1 hour or more before pain occurs. In this case, the following neurological symptoms appear - one or more:
- visual disturbances – photophobia, blinking, black spots in the field of vision, flickering arches, lines, zigzags, incorrect perception of objects in the field of vision;
- sound disorders, mainly intolerance to any sounds;
- speech problems;
- sensory disturbances – tingling, burning, numbness, etc.;
- impairment of motor abilities, such as sudden weakening of muscles on one side of the body.
Causes
Migraine occurs against the background of various external and internal causes (triggers), each of which can cause another attack:
- mental and psycho-emotional stress;
- constant severe stress;
- sleep disturbances, insufficient rest at night;
- chronic fatigue (mental and physical);
- smoking;
- previous head injuries (even many years ago);
- excessive physical activity for a particular person;
- hormonal surges: puberty, menstruation (“menstrual migraine”), pregnancy;
- consumption of foods containing tyramine (chocolate, coffee, citrus fruits, nuts, cheese, smoked meats);
- drinking alcohol, especially low-alcohol drinks;
- sharp fluctuations in atmospheric pressure, changes in air temperature;
- overstrain of the senses: sharp sound, bright light, strong unpleasant odor, etc.;
- staying in a hot or stuffy room, etc.
Each person has his own “dangerous” factors. Most of them can be calculated and, if possible, avoided in the future.
Sadness and fear are common causes of migraines
One day one of the patients said that migraine is suppressed sadness and fear. She came to therapy for completely different reasons, and for a long time I didn’t even know she had migraines.
Some time ago we talked about this disease, studying under what circumstances it appears. This observation helps to obtain information about what feelings pain may be a response to.
But that was about six months ago. And now here's a discovery. Increasingly aware of her feelings and the benefits of being able to experience them, this woman tried to observe them and not lose sight of them.
She noticed that the last time she got a migraine right after she felt sad . And the final proof for her was the fact that when she didn't run away from the feeling and allowed herself to feel it, the pain subsided.
For some time we worked on her ability to process grief, which she “always” ran away from and tried not to feel. She was very afraid of him, that she would not be able to withstand despair if she allowed him, and she avoided him in every possible way, to such an extent that sometimes it was difficult for her to understand that she felt him at all. And migraine was one of the symptoms that masked and at the same time reminded that not all was well.
Symptoms
A migraine attack follows a standard scenario, consisting of several successive stages.
- Prodromal (initial) stage. A person’s mood begins to change, yawning and drowsiness appear, or, conversely, insomnia. Some report sensitivity to noise and bright light. Sometimes there is a slight numbness in one of the hands. For most patients, these symptoms are enough to know that a full-blown migraine attack is on the way. The duration of the prodromal stage ranges from several hours to several days; it is not present in all patients.
- Aura. Occurs against the background of cerebral vascular spasms. Most often it manifests itself in the form of visual disturbances (flashes in the form of spots, zigzags or lightning in front of the eyes, distortion of the contours of objects, loss of individual fields of vision). Less common are taste or hearing disorders, problems with coordination of movements, etc. Aura is not observed in all patients.
- Actually a migraine attack. In most cases, it manifests itself as a unilateral headache that is pulsating in nature. It starts with slight discomfort and gradually gains strength, becoming simply unbearable. Movements, changes in body position, bright lights and loud sounds intensify the sensations, which is why patients try to spend this time lying in a darkened room. Against the background of a headache, many patients report nausea, vomiting, soreness in the muscles of the neck and shoulders, nasal congestion, lacrimation, chills and even fever. The duration of the attack is individual and ranges from 2-3 hours to several days.
- Resolution stage. At this time, the headache goes away on its own or after taking medications. Many patients fall asleep at first, but within 24 hours after the attack they may feel weak, lethargic, dizzy, and depressed. Increased sensitivity to light, sounds and smells also does not go away immediately. Less common is the opposite type of resolution stage, in which patients note increased activity.
What does migraine with aura mean?
Migraine with aura is a disorder characterized by recurrent episodes of reversible local neurological symptoms (aura), usually increasing over 5-20 minutes and lasting no more than 60 minutes.
“Aura” is a term by which doctors mean the following:
- Visual impairment
. These can be lines, lights, spots, flickering. In severe cases, loss of vision. All manifestations are reversible. - Sensory perception disorders
. It seems that goosebumps are crawling all over the body, the person feels tingling, and there may be areas of numbness. All this is also reversible. - Speech disorders
, which also go away along with the attack.
In 73% of migraine attacks with aura, the headache begins not after the end of the aura, but during the aura itself and can be accompanied by other migraine symptoms - nausea (51%), photophobia (88%) and phonophobia (73%) i Morozova O.G. Migraine: new international criteria for diagnosis and principles of therapy based on evidence-based medicine and our own clinical experience / O.G. Morozova // International Neurological Journal. — 2021. — No. 3 (81). — pp. 131-138. . It happens that a panic migraine develops. Its complications are fear, anxiety, etc.
Migraines with and without aura are the same. A person usually feels a throbbing pain in one side of the head. Often it is concentrated in the eyeball. The pain intensifies with movement, sound and light stimuli. It can last from 4 hours to 3 days. At this time, it is impossible to lead a normal lifestyle. A person wants to be left alone in a dark and cool room, freeze, hide under the blanket. Typically, patients describe the pain as “bursting,” “splitting,” “about to burst,” “every sound like a hammer on the head.” And even after an attack, the consequences persist. The person is apathetic, tired and overwhelmed. It takes more than one day to recover.
Types of pathology
Migraines are most often classified according to the presence of an aura and its type. The following types of disease are distinguished:
- classic migraine: before an attack of pain, a typical aura occurs with visual, auditory, olfactory and other disturbances;
- migraine without aura: symptoms appear suddenly against a background of relative well-being; the rest of the clinical picture is characteristic of the disease.
Depending on the predominant symptoms, the following types of migraine are distinguished:
- ocular (ophthalmic): accompanied by classic visual impairments: glare, flickering, flare in certain areas of the visual field;
- retinal: the disease manifests itself as complete or partial loss of vision in one eye due to impaired blood circulation in the vessels of the retina;
- ophthalmoplegic: manifested by double vision, visual distortions, drooping of the eyelid;
- basilar: accompanied by dizziness, ringing in the ears, unsteadiness when walking, blurred speech;
- hemiplegic: characterized by loss of sensation and impairment of motor function of one arm or arm and leg on one side;
- cervical: occurs against the background of impaired blood flow in the vertebral arteries and is accompanied by a very severe headache;
- aphasic: pain is accompanied by speech disorders, as with a stroke;
- abdominal: additionally manifests itself as severe pain throughout the abdomen, diarrhea, nausea and vomiting; this form is very common in children;
- “decapitated”: the patient does not feel a headache, as a rule, only visual disturbances are noted, while the prodromal period and aura occur typically.
Migraine status stands apart. This is a severe condition in which two or more attacks occur in a row with less than 4 hours between them. This type also includes pain that lasts for more than 3 days. Against the background of migraine status, the patient experiences repeated vomiting, which does not allow him to eat, drink, or take medications normally.
How to cope with psychosomatics faster
Watch the video from our psychologist with more than 20 years of experience, Olga Kopylova. In it she talks about how psychosomatics is formed:
Two points are important: getting to the exact cause and choosing the right psychological techniques. If you break down all the work into stages, then it would be more advisable to go this way:
- determine the initial situation,
- specify the root emotion (anger, guilt, shame, grief - each has its own),
- select appropriate psychological techniques,
- check the correctness of their implementation,
- adjust the emotion (develop new reactions to provocations).
Moreover, you can take the first step to find the cause today. To do this, take our test:
Take the test
Example : you can read for a long time about constipation - that these are mental blocks, dislike for yourself. But in 95% of cases it appears in a state of choice, in limbo. If you have basic mistrust and anxiety, constipation becomes chronic and worsens during the period of choice.
Consequently, situations with choice will never end, but the attitude towards them can be changed using psychotherapeutic methods.
What do the majority do?
They study the theory, but do not achieve improvement.
The fact is that working independently with your unconscious requires a lot of preparation.
Do you need a specialist?
It will just be faster with him. It’s possible to cope on your own, but only a few can do it and it takes a long time.
In our practice, the terms varied from 1 consultation to a year. The most common cases are:
- headache,
- Gastrointestinal tract (for example, irritable bowel syndrome),
- gynecological and genitourinary problems (for example, cystitis and urethritis),
- lungs (for example, bronchitis),
- various allergies,
- childhood illnesses through parents and others.
As you can see, the psychosomatics of migraine in women is quite amenable to work and adjustment. If you need an experienced specialist along this path, you can find out about working with us here. I wish you health and psychological comfort!
Diagnostics
The patient's headache has characteristic features that immediately suggest a migraine. For diagnosis, the doctor uses the following methods:
- collecting complaints and medical history to determine the nature of the pain; special attention is paid to: the time of onset and end of the attack;
- provoking factors;
- nature of pain;
- the absence or presence of an aura, its symptoms;
- well-being after an attack;
If necessary, additional examinations and consultations with specialists are prescribed. The diagnosis of migraine is made by exclusion when no other causes of headache have been identified.
Make an appointment
Treatment
Migraine treatment is divided into two areas:
- relief of the patient’s condition during an attack;
- preventing the occurrence of new attacks.
Help during a seizure
At the first signs of an impending migraine attack, it is necessary to eliminate as quickly as possible all factors that can increase the pain:
- turn off the lights and TV, close the curtains;
- eliminate sources of extraneous sounds as much as possible;
- provide access to fresh, cool air;
- go to bed.
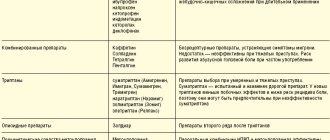
To prevent and relieve immediate pain attacks, painkillers of various groups are used:
- analgesics and non-steroidal anti-inflammatory drugs (analgin, ibuprofen, indomethacin and their analogs): used for mild attacks that do not affect a person’s daily life;
- combination drugs (codeine, tempalgin, solpadeine): prescribed for moderate attacks that have little effect on life activity;
- triptan drugs (amigrenin, sumamigren, zomig and others) are used if attacks interfere with normal life;
- hormonal drugs (dexamethasone): used for severe and prolonged migraines in combination with other medications.
Additionally, antiemetics (metoclopramide, cerucal) can be used.
Home remedies to prevent a migraine attack are used as an addition to the main therapy. Many patients benefit from:
- cold compress on forehead;
- rubbing essential oils into the temple area;
- infusion of chamomile, mint, lemon balm, lavender and other herbs that promote relaxation;
- acupressure on acupuncture points: at the base of the skull, between the eyebrows in the hollow above the bridge of the nose, on the back of the foot (the hollow between the first and second toes).
It is important to remember that these remedies do not replace primary therapy.
Treatment between attacks
Preventing the occurrence of attacks is no less important than relieving pain and nausea. Currently, various groups of drugs are used:
- beta-blockers (propranolol and drugs based on it);
- antidepressants (venlafaxine, milnacipran, etc.): have a good effect in the treatment of chronic pain, and also reduce the manifestations of depression characteristic of patients with frequent attacks;
- anticonvulsants (Depakine, topiramate): well tolerated and significantly reduce the frequency of exacerbations.
Medicines are used:
- if exacerbations occur more than 2 times a month;
- if attacks last more than 48 hours;
- with severe headache or complications.
In other cases, general preventive measures are sufficient.
Female migraine
The dynamics of the prevalence of migraine in men and women in different age groups is presented in Figure 1. A clear understanding of hormonal influences on the course of migraine is important for its treatment in women.
Migraine in childhood
The prevalence of migraine, as well as the characteristics of its clinical picture and course in childhood and adolescence differ from those in adults. In boys aged 4–7 years, the prevalence of migraine is higher than in girls, in whom it usually debuts at menarche. By the time they reach adolescence, the prevalence of migraine in girls is 3 times higher than in boys. In general, the majority of women experience migraine onset before the age of 19 years.
Compared to adults, migraine attacks in children are usually shorter (1–48 hours), headaches (TH) reach their peak intensity more quickly (usually within 1 hour) and can be bilateral. Young children often experience migraine equivalents, such as benign paroxysmal vertigo, paroxysmal torticollis, and cyclic vomiting. In addition, girls often experience migraine attacks on weekdays during or after school.
In general, more conservative approaches are used in the treatment of migraine in children than in adults. Prevention should be aimed, first of all, at changing lifestyle and controlling provocateurs. Stress and overwork are among the most common triggers of migraines in children and adolescents. Biofeedback and stress management techniques are highly effective in this age group. At the same time, about a third of girls with migraines require medication to control the frequency of attacks. In childhood, for the preventive treatment of migraines, it is possible to use topiramate (especially in overweight girls), magnesium supplements, amitriptyline and propranolol.
Menstrual migraine
The menstrual cycle is one of the important provocateurs of migraine attacks. The relationship between migraine and menstruation is observed in 60% of women of reproductive age. Typically, this relationship develops gradually in the second decade of life; in most women, the presence of a migraine attack during menstruation becomes obvious by the age of 35.
A migraine attack can occur before or during menstruation. However, menstrual migraine attacks are usually more severe, they last longer and may be resistant to analgesics. In addition, menstrual attacks are often resistant to preventive treatment.
Menstrual migraine is represented by 2 forms: true menstrual and menstrual-associated migraine (Table 1).
True menstrual migraine is a relatively rare condition, occurring in only 10–14% of women. Menstrually associated migraine occurs in approximately 50% of women. Moreover, in addition to a migraine attack in the perimenstrual period, migraine attacks are also observed on other days of the month. The menstrual attack is often the most severe, with nausea, vomiting and significant disability, but for some women other attacks are a particular problem, and the number of them can be very large. When stopping attacks not associated with menstruation, a stratified approach is relevant, when the choice of drug is determined by the severity of the attack. If the patient experiences severe attacks in which her ability to work is significantly impaired, triptans should be taken.
By definition, menstrual migraine is always migraine without aura. However, such patients may also experience migraine attacks with aura on other days of the cycle. This fact must be taken into account when selecting preventive therapy.
The pathogenesis of menstrual migraine is based on increased sensitivity to normal fluctuations in estrogen levels throughout the menstrual cycle. Figure 2 shows the inverse correlation between the likelihood of a migraine attack and the concentration of estrogen degradation products in the urine.
Treatment of menstrual migraine presents significant challenges. In many patients, such an attack is not well controlled by analgesics, even triptans, the pain intensity quickly increases, vomiting occurs, and the attack itself can last longer than usual (up to 3-4 days). During this time, the patient takes a large number of analgesics, which bring, at best, short-term relief. This is why a number of patients with menstrual migraine need preventive treatment, even if the number and severity of other migraine attacks are small. In some situations, preventive treatment is necessary even for patients with true menstrual migraine. This means that the patient is forced to take medications daily for a long time to reduce the severity of a migraine attack, which occurs only once a month.
Keeping a headache diary for at least 3 months is critically important in this situation. This will not only establish the relationship with menstruation, but also assess the effectiveness and quantity of analgesics used, as well as the overall frequency of attacks.
In case of insufficient effectiveness of pain relief, as well as a high frequency of attacks (if it is necessary to take analgesics more than 2 days a week), preventive treatment is indicated using traditional non-drug and pharmacological approaches for migraine. The goal of such therapy is to reduce the frequency of migraine attacks, as well as their duration and intensity, which is especially important for a migraine attack during the menstrual period.
However, even if preventive therapy is effective, the severity of a menstrual headache attack can remain significant. If it is the menstrual migraine attack that poses a particular problem for the patient, there is the possibility of mini-prevention. It makes sense in patients with a regular menstrual cycle and a relationship with menstruation documented in the diary. This will allow you to predict in advance the day the attack will begin.
For mini-prevention, hormonal and non-hormonal agents are currently used. To prevent a menstrual attack, certain analgesic medications are taken throughout the perimenstrual period. For this purpose, naproxen (550 mg 2 times / day), acetylsalicylic acid (500 mg 2 times / day) or mefenamic acid (500 mg 3 times / day) can be used. You should start taking the drug 2-4 days before the menstrual migraine attack and before the 3rd day of menstruation. Since the effectiveness of such prevention is low, you can try different drugs to select the most suitable one. This method can primarily be recommended to patients whose menstruation is accompanied by abdominal pain.
Triptans are significantly more effective as a mini-prophylaxis, however, to prevent a menstrual attack of hypertension, it is necessary to take a significant amount of medication: sumatriptan (25 mg 3 times a day), naratriptan (1 mg 2 times a day), zolmitriptan (2. 5 mg 2 times/day). The drug is taken for 5-6 days, starting 2 days before the expected migraine attack.
Since the provocateur of a menstrual migraine attack is a normal drop in estrogen levels in the second phase of the menstrual cycle, its stabilization throughout the cycle seems to be an effective method of preventing the disease. Hormonal prophylaxis methods are aimed at preventing the decline in estrogen levels during the luteal phase of the menstrual cycle and can be offered to patients with treatment-resistant menstrual migraine attacks and no contraindications to the use of such methods. More detailed information about the use of hormonal drugs for migraine is provided in the next section.
As a result of many years of research in the field of hormonal methods of mini-prevention of menstrual migraine attacks, it was concluded that the use of combined oral contraceptives (COCs) according to a special scheme is preferable. The use of transdermal estrogen preparations during the perimenstrual period has been found to be less effective.
Currently, patients with severe attacks of menstrual migraine can be recommended to take COCs using only active tablets (taking without a break for 7 days or skipping inactive tablets). The drug is usually taken for 4 cycles (84 days), then a break is taken for 7 days. In this way, 3 out of every 4 menstrual attacks can be prevented. For this purpose, monophasic low-dose (preferably micro-dose) COCs are used.
Using oral contraceptives for migraines
Many migraine patients take COCs for contraception and to treat endometriosis, dysmenorrhea, heavy menstrual bleeding, or acne. The most commonly used drugs contain a combination of ethinyl estradiol and a progestin. Such drugs block ovulation and change the natural dynamics of estrogen levels. For this reason, COCs may have different effects on the course of migraine.
In monophasic COCs, all active tablets contain the same amount of estrogens and progestogen. Low-dose COCs (containing less than 35 mcg ethinyl estradiol) can be used in most women with migraine. Contraindications to the prescription of estrogens include the presence of migraine with aura, bleeding disorders, diabetes mellitus, arterial hypertension, and smoking. Thus, COCs can be prescribed to patients with migraine without aura who do not have risk factors for ischemic stroke. This is because in women with migraine without aura, the risk of ischemic stroke and venous thrombosis is no greater than that in women without migraine. The risk of stroke in young women aged 25–29 years is 2.7 per 10 thousand women. Taking COCs increases this risk to 4. At the same time, with migraine with aura, the risk of stroke when using COCs increases 8 times. In patients suffering from migraine with aura, the risk of stroke increases by 34 times when smoking and taking COCs are combined. In this regard, migraine with aura is a contraindication for taking COCs.
After starting to take COCs, the frequency of migraine attacks should be carefully monitored during the first month of use. In cases of increased migraine frequency, increased severity of attacks, or the appearance of aura symptoms, COCs should be discontinued.
The use of COCs for the prevention of migraine cannot be recommended. However, as stated above, COCs can be used for mini-prophylaxis of menstrual migraine attacks. For this purpose, it is preferable to use microdose COCs containing less than 30 mcg ethinyl estradiol.
Migraine during pregnancy and lactation
During pregnancy, 50–70% of women experience improvement in migraine without aura. Migraine attacks become mild, extremely rare, and in many patients stop completely. Improvement occurs after the end of the first trimester, starting from 12–14 weeks. pregnancy (Fig. 3). This is due to the fact that by the beginning of the second trimester, the level of estrogen stabilizes - it increases 6 times, and its fluctuations stop. Migraine with aura stops less often during pregnancy - in approximately 40% of patients.
In patients with migraine, pregnancy planning is important. By the time of pregnancy, it is necessary to ensure maximum control over the number of migraine attacks. For a number of patients, this requires preliminary preventive treatment in order to reduce migraine attacks, as well as the abolition of analgesics. During such treatment, it is necessary to convey to the patient the need to comply with contraceptive measures. If it is impossible to stop preventive therapy after achieving the optimal frequency of attacks, it is necessary to replace all drugs used with drugs approved for use during pregnancy.
During the period of preparation for pregnancy, it is necessary to teach the patient methods of non-drug control of hypertension. This will minimize the need to take painkillers and medications for the preventive treatment of migraines during pregnancy.
Relief of migraine attacks during pregnancy
The selection of drug therapy for patients with migraine during pregnancy poses significant difficulties. In an ideal situation, the use of drugs should be kept to a minimum, especially in early pregnancy, in order to minimize the risk to fetal development.
At the same time, the severity of migraine is especially high during the first trimester of pregnancy. During this period, the course of migraine may become even more severe than before conception. Full-blown unrelieved migraine attacks are often accompanied by nausea, vomiting and lead to suffering and dehydration, especially in patients with early gestosis.
During pregnancy, minimizing the amount of medications you take becomes a priority. A stepwise approach should be recommended, starting with non-drug approaches for mild to moderate attacks. It is recommended to take medications at the very beginning of an attack only in case of a rapid increase in pain intensity and disability.
Nausea is a common symptom during pregnancy, especially in the first trimester. During this period, the most severe course of migraine attacks is observed with the greatest likelihood of developing nausea and vomiting during an attack of headache. Dehydration, which can occur as a result of repeated vomiting in pregnant patients, in turn is a provocateur of migraine attacks.
To reduce the severity of nausea and prevent vomiting during a migraine attack, patients should avoid strong odors and drink more fluids, for example, juices diluted with water in a 1:1 ratio. Feelings of nausea can also be reduced by eating easily digestible foods, such as crackers, applesauce, bananas, rice, pasta, and ginger. An effective remedy is vitamin B6 at a dose of 30 mg/day. In case of severe nausea, medications must be used. Preference is given to drugs with safety category B (metoclopramide, ondansetron).
Drinks containing caffeine (coffee, cola, sweet tea) may help relieve headaches. For mild hypertension, a short walk, swimming, soft music, a warm heating pad, stretching exercises for the neck muscles, relaxation exercises, and breathing exercises are also effective. At the first symptoms of an aura or at the onset of headache, it is recommended to try to fall asleep. In addition, relaxation and biofeedback (BFB) exercises at the very beginning of a migraine attack are effective in 75% of pregnant women.
The frequency of regular use of medications to relieve migraine attacks should not exceed 2 days a week in order to reduce the risk of developing drug-induced headache. The range of drugs that are used to relieve migraine attacks during pregnancy is significantly limited. Despite the fact that, in general, paracetamol is less effective for relieving an acute attack of migraine than acetylsalicylic acid and nonsteroidal anti-inflammatory drugs (NSAIDs), its safety during pregnancy is higher.
Taking NSAIDs in early pregnancy is associated with an increased risk of miscarriage, perinatal mortality, and intrauterine growth retardation. For these reasons, the use of NSAIDs should be limited to the second trimester. Acetylsalicylic acid in analgesic doses is also recommended for use only in the second trimester.
Caffeine is an important addition to analgesics and has the ability to enhance their analgesic effect. Among combined analgesics during pregnancy, preference is given to drugs containing only paracetamol and caffeine. In addition, a caffeinated drink can be added to a simple analgesic (Table 2).
Triptans are the most effective analgesics for the relief of migraine attacks. The safety of their use during pregnancy is assessed using pregnancy registries. The largest amount of data has been collected for sumatriptan. There is no information indicating an increased risk of congenital malformations with its use. At the same time, insufficient data has been accumulated to formulate official recommendations.
Currently, the widespread use of triptans during pregnancy is not recommended, except for use in patients (based on expert advice) who experience severe migraine attacks leading to serious disability and vomiting.
The use of analgesics containing codeine is undesirable due to the possibility of constipation and nausea. Drugs containing phenobarbital are prohibited for use in pregnant women.
A schedule of follow-up visits agreed upon with the patient will allow her to adhere to a clear treatment plan, and will also enable the doctor to prescribe a course of preventive treatment for migraine in a timely manner, if necessary. In order to monitor the frequency of headaches and the effectiveness of the analgesics used, the patient needs to keep a headache diary, recording information about the use of non-drug methods, the frequency, severity and duration of headache attacks, and the presence of attacks of other forms of headache. This will determine the degree of compliance with recommendations and the need for preventive treatment.
Preventive treatment of migraine during pregnancy
The neurologist needs to promptly identify a group of patients who need preventive treatment for migraine. Persistence of frequent migraine attacks by 10–12 weeks. pregnancy indicates a high probability of persistence of headache throughout its entire duration.
Preventive treatment of migraine is necessary for patients in the following cases:
- high frequency of attacks (more than 2 days a week) due to the high risk of drug-induced headache;
- the presence of severe or prolonged attacks;
- significant disability;
- development of dehydration and insufficient absorption of nutrients;
- poor response to approved analgesics.
Pain management techniques (relaxation, biofeedback and stress management methods), lifestyle adaptation to control attack provocateurs, as well as dosed physical activity are highly effective. Patients with musculoskeletal pathologies should be recommended to regularly perform special exercises, as well as a course of massage or manual therapy in the early stages of pregnancy.
β-blockers have the best combination of effectiveness and safety in the treatment of migraine in pregnant women. Due to the widespread use of propranolol in the treatment of hypertension during pregnancy, a significant amount of safety data has accumulated for this drug. Propranolol is considered the drug of first choice for the preventive treatment of migraine during this period. The drug should be used with caution in patients with bronchial asthma, a tendency to arterial hypotension and bradycardia. The dose of β-blockers should be gradually reduced during the last weeks of pregnancy (from 36 weeks).
Tricyclic antidepressants are highly effective in the preventive treatment of migraine. At the same time, there is evidence of the possible teratogenic effects of amitriptyline. Selective serotonin reuptake inhibitors are not recommended for use due to their significantly lower effectiveness compared to the effectiveness of tricyclic antidepressants. While the use of antidepressants during pregnancy is necessary for the treatment of significant mood disorders, their use in nondepressed migraine patients is limited due to the small risk of teratogenicity associated with the use of most antidepressants at different stages of pregnancy. In addition to the above drugs, the use of magnesium is recommended.
Recommendations for preventive treatment of migraine during pregnancy are given in Table 3.
Migraine during lactation
Despite the fact that chronic headache in the second and third trimesters of pregnancy in most women is not intense, it usually recurs after childbirth. Breastfeeding allows you to delay the return of hypertension, so breastfeeding should be encouraged. Such patients should be provided with information about the safe use of medications during this period.
During breastfeeding, it is necessary to use analgesics to relieve attacks of moderate and high intensity no more than 2 days a week.
Some medications, such as paracetamol and ibuprofen, can be used by a nursing mother regardless of feeding time. If unsafe drugs are used, breast milk must be expressed for several hours after taking them, and previously stored milk must be used for feeding.
Information on the use of analgesics during lactation is given in Table 4.
The safety of triptans during lactation is still incompletely studied. However, the data collected to date does not allow us to talk about their possible harm to the child. The American Academy of Pediatricians approves the use of sumatriptan during lactation. For other triptans, as well as generic preparations of sumatriptan, insufficient data have been accumulated on the safety of use during breastfeeding. If you are taking these medications, you must express milk for at least 4 hours after taking them.
If non-drug approaches are insufficiently effective, patients with frequent or severe migraine attacks need to choose a drug therapy regimen.
Propranolol and timolol are more effective in the treatment of migraine; the safety of their use during lactation has been studied quite well. For these reasons, propranolol is the first choice drug for the treatment of migraine during lactation. The use of valproic acid is compatible with breastfeeding. Other antiepileptic drugs are not recommended for the prophylactic treatment of migraine during lactation due to the lack of convincing data on their safety. The use of antidepressants for the preventive treatment of migraine during this period is extremely undesirable.
Recommendations for preventive treatment of migraine during breastfeeding are presented in Table 5.
Medicines for the preventive treatment of migraines should be taken before the longest break in feeding the baby (ideally, before the longest period of sleep for the baby).
Migraine during menopause
Migraines usually improve with age. However, this occurs in only about a third of women, most often in those patients who have had menstrual migraine. However, during perimenopause, when the menstrual cycle becomes irregular, many women experience worsening migraines. This period can last more than 10 years. During this time, there are irregular fluctuations in hormone levels and a gradual decrease, which can lead to symptoms such as fatigue, insomnia, irritability, hot flashes, decreased libido and poor concentration. Worsening migraines may signal the onset of perimenopause and make treatment more difficult.
Some women use hormone replacement therapy to treat menopausal symptoms. For this purpose, estrogen preparations can be used. The effect of this treatment on migraine may vary. If the course of migraine worsens, similar to the use of COCs, the need for therapy should be reconsidered. In general, the worsening of migraine occurs somewhat less frequently with the use of transdermal estrogen preparations due to the creation of a more stable physiological concentration of hormones than with the use of tablet preparations.
Migraine in old age
The appearance of migraine after 60 years is extremely unusual and requires additional examination of the patient to exclude secondary causes of headache, the frequency of which is about 30%.
Migraine in older women may be accompanied by an aura; attacks that occur in the form of an aura without headache (“decapitated migraine”) are also common. Such attacks require a differential diagnosis with transient ischemic attacks.
The presence of comorbid diseases and the use of a large number of drugs for the treatment of somatic diseases often complicate the treatment of migraine in older women. At the same time, the prevention of migraine in patients with coronary heart disease is especially important due to the fact that triptans are contraindicated in these patients. In this case, as well as in arterial hypertension, a β-blocker may be the first choice drug for the preventive treatment of migraine. Despite the high effectiveness of tricyclic antidepressants, in this age group the prescription of these drugs is problematic due to the frequent presence of contraindications. In general, all migraine medications should be prescribed at lower doses than in younger women to reduce the risk of unwanted effects.
Conclusion. Migraine is widespread in the female population. At the same time, there are features of its course in different periods of a woman’s life. In recent years, new treatments for migraine have been developed based on an understanding of its pathophysiology in women of different ages. Taking these features into account will allow us to optimize methods for relieving migraine attacks and select the most successful preventive therapy.
Prevention
Prevention of migraine attacks is not only properly selected drug therapy, but also correction of the patient’s lifestyle. Doctors recommend:
- normalize sleep: for the normal functioning of the body, at least 8 hours of night sleep every day are required;
- minimize the consumption of foods that can cause an attack, especially chocolate, spices, and alcoholic beverages;
- eliminate smoking;
- adhere to a balanced diet with a mandatory breakfast and intervals between meals of no more than 5 hours;
- observe the drinking regime and consume at least 1.5-2 liters of clean water per day; in hot weather this amount can reach 2.5-3 liters;
- establish a work and rest schedule, avoid mental and physical fatigue;
- reduce stress levels as much as possible;
- make a habit of light or moderate physical activity: swimming, walking, cycling, yoga, Pilates;
- promptly identify and treat chronic diseases, especially osteochondrosis of the cervical spine, atherosclerosis and other pathologies that contribute to the deterioration of blood flow in the brain.
Regular health resort treatment of a restorative nature and tourist trips without extreme changes in climate and time zones have a good effect.
Treatment at the Energy of Health clinic
Neurologists at the Health Energy clinic are ready to help with migraines of any severity. We offer each patient:
- individual selection of drugs for the relief and prevention of attacks;
- training in relaxation and self-help techniques;
- sessions of restorative massage and physical therapy in the absence of contraindications.
Treatment is selected according to the individual characteristics of the body. Before prescribing a specific regimen, a complete examination of the patient is carried out to exclude other causes of headache.
Advantages of the clinic
Medical facilities are equipped in accordance with modern standards of diagnosis and treatment of diseases. We try to make every patient feel comfortable within the walls of the clinic and offer:
- consultations with doctors of various specialties;
- informative methods of instrumental, functional and laboratory diagnostics;
- individual selection of treatment regimen;
- complex effect on the body using not only drugs, but also additional methods: physiotherapy, massage, exercise therapy, manual therapy, etc.
Reception is by appointment, without queues or long waits. The location of the centers allows both motorists and those traveling by public transport to reach us comfortably.
If migraine attacks are making your life miserable, do not endure the pain. Contact the neurologists at Health Energy. Together we will find a way to relieve you of this disease.