Early help for hydrocephalus is a chance for a normal life. Professional management of the disease and competent rehabilitation can reduce complications and the degree of disability by 60%.
What it is
The Greek word “hydrocephalus” is used by specialists along with the Russian term “dropsy of the brain.” If translated literally from ancient Greek. ὕδωρ “water” + κεφαλή “head”, so it turns out – “water in the head”.
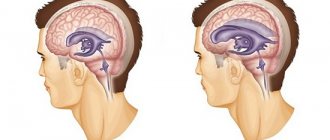
However, we are not talking about water, but about cerebrospinal fluid (CSF), which accumulates in the ventricles of the brain and/or in the space between the membranes of the brain. Liquor is produced in the ventricles, then circulates inside the skull, then moves into the circulatory system through special veins. This is a kind of “safety cushion”. It protects the brain and spinal cord from external mechanical influences, that is, it softens blows and other sharp impacts. It also removes harmful substances from the brain and delivers useful ones, that is, it supports metabolic processes between the blood and the brain.
Usually there is very little cerebrospinal fluid, in infants - only 50 ml. But if suddenly the production of cerebrospinal fluid becomes excessive or the outflow becomes difficult, an excess of it appears and intracranial pressure increases. This syndrome is called hydrocephalus.
Excess cerebrospinal fluid puts pressure on the brain - and this can lead to severe neurological disorders, decreased vision, weakness in the upper and lower extremities, decreased intellectual abilities, and most importantly, death.
Brain shunting: features
Surgeries performed to create additional pathways for the drainage of biological fluids using implants are called bypass surgery. After the operation, the patient quickly returns to a full life and does not experience painful symptoms. The procedure can be carried out after the appointment of a neurosurgeon who will study the examination results in detail.
Brain shunting for hydrocephalus, the consequences of which develop quite often, allows you to restore blood flow in the brain, its functions, and normalize intracranial pressure. Before the procedure, the patient undergoes a thorough examination in order to identify contraindications and create a unified picture of the course of the disease. This operation is performed in the Yusupov Hospital, located in Moscow, where all conditions have been created for a comfortable stay for patients and the provision of high-quality medical care.
Cause
Neurosurgeons count more than 180 reasons that can cause the development of hydrocephalus. It can be congenital (when a child is born with an excess amount of cerebrospinal fluid in the head) or acquired as a result of other problems:
– traumatic (develops after a trauma, for example, birth trauma, cerebral hemorrhage), – inflammatory (develops after neuroinfections), – tumor (the tumor blocks the outflow of cerebrospinal fluid or stimulates increased production), – vascular (due to vascular diseases of the brain), – idiopathic (when the reason is not clear).
At risk are premature babies and children with excised spina bifida (since the spinal cord is connected to the brain, hydrocephalus often manifests itself as a concomitant disease). Most often, hydrocephalus is detected before the age of three months; boys develop it more often than girls.
Alenka. Reset stigmas
Svetlana Lisunova, an activist of the MBOO helping children with neurosurgical diseases “He needs you”, Alenka’s mother with post-hemorrhagic occlusive hydrocephalus, says:
“I stood under the door of the intensive care unit and only heard: “This is already a corpse. Why are you clinging to her”, “Imagine that it’s an abortion”, “It’s better to cry once now than to cry all your life later”
Difficult birth. Brain hemorrhage. They immediately said about their daughter: “she won’t survive.” And that’s probably why they didn’t do much about it. She lay in intensive care for 12 hours without artificial ventilation. She just lay there and gasped.
“Sick leave? If he dies, come and get sick leave.” They weren’t allowed to baptize: “There’s no point in shaking dirty robes here.” They didn’t take expressed milk: “We don’t need your goat urine here.”
At three months, Alenka, without waiting for her death, was nevertheless discharged home. Within a week, Svetlana realized that hydrocephalus was growing. Alenka cried sharply, burped heavily, her eyes literally popped out of her head - she was probably tormented by severe headaches. The accumulating cerebrospinal fluid began to put pressure on the brain.
Svetlana is a doctor by training. She could recognize hydrocephalus. What's next? Of course, she, an orthopedist by specialty, took a course in neurosurgery in a very truncated form. But what exactly? I got out the textbooks. “A condition incompatible with life... die in the first days of life... parents suffering from drug and alcohol addiction...”
Svetlana devoted the next ten years of her life to refute each of these lines of that rotten textbook. Reset stigmas.
Today she is an activist in the public organization “He Needs You.” And her Alenka is a 10-year-old beauty and an excellent student. Her friends, wards, colleagues - hundreds of parents of children with hydrocephalus.
There is not a single person with addictions among them. The vast majority of cases of hydrocephalus she encounters are rooted in birth injuries and cerebral hemorrhages. A small percentage of children received congenital hydrocephalus (usually it is also associated with intrauterine injuries - accidents, etc.). And a small percentage of hydrocephalus is associated with infections suffered by the mother during pregnancy.
Treatment methods
Timely – early – intervention makes hydrocephalus not as fatal as before. Modern treatment methods save 95% of patients with a similar diagnosis. Surgery is virtually the only method of combating the disease. Drug methods in most cases can only slow down the course of the disease, but do not eliminate the root cause.
Modern techniques have many options for surgical treatment of hydrocephalus. In order to remove excess fluid from the cranial cavity, shunting is usually used. It consists of installing a shunt, which can be compared to a pipeline. It pumps out excess cerebrospinal fluid and pumps it into other cavities of the body - into the abdominal cavity, into the atrium.
Silicone valve systems are used as a shunt, which help regulate the pressure of cerebrospinal fluid in the cavities of the brain. The drainage system (shunt) and the level of pressure in it (in the case of programmable shunts) are selected by a neurosurgeon depending on the form of hydrocephalus and the age of the child. Bypass surgery is free and is included in the compulsory medical insurance list.
Endoscopic operations are also used as surgical treatment. The purpose of the endoscopic operation is to create an anastomosis (connection) between the cavity of the third ventricle and the basal cisterns (the second largest cavity of the brain, which is a reservoir for cerebrospinal fluid), located at the base of the skull. This operation is appropriate for outflow disorders in the posterior cranial fossa.
Endoscopic operations are also widely used when it is necessary to remove any obstacle to the movement of cerebrospinal fluid, for example, to remove a cyst. Without exception, all operations are aimed at restoring the balance between the production and absorption (discharge) of cerebrospinal fluid.
Alenka: she can do anything!
For 10 years, Svetlana tirelessly explains to neurologists at appointments that a “ventricle” is not a “small stomach”, it is a part of the brain. And the shunt is not in my daughter’s stomach, but in her head.
But she is not tired, she is ready to continue doing this. Enlighten. Inspire. Inform.
“Why am I writing about my daughter and her successes? Sometimes you really want to climb deeper into the den and not let anyone in there. But I see how these posts inspire those parents who are just faced with this diagnosis. They see Alenka on a horse, at a reading competition, at a meeting with producer Maxim Fadeev - and believe in the best.
One day, Alenka, my eldest daughter Nastya, and I went on a horseback riding trip. I was nervous about my eldest and kept shouting to her: “Nastya, hold on! Nastya, hold on!”
Finally, the instructor couldn’t stand it and said: “Yes, she’s holding up better than anyone else,” and points to Alenka. I laugh: “Yes, I know, I’m shouting to the eldest.”
Alenka is confident both in the saddle and on stage. Not a single performance at school goes on without her. Even when she couldn’t walk yet, she played... Kolobok!
What she hasn’t been able to do yet is seriously take up music (we are often in hospitals, it’s difficult to organize a regular schedule of classes) and dancing (dances for wheelchair users are not suitable for her - she has already left the wheelchair, and the usual ones are not yet possible).”
But, looking at Alenka and her mother, we can confidently say: “This is not working out YET!” Once upon a time, doctors, looking at shunt-dependent Alena, only said: “Sit near the intensive care unit and don’t rock the boat!”
And only Dmitry Yuryevich Zinenko (now the head of the neurosurgical department of the Yu.E. Veltishchev Research Institute of Pediatrics) said: “You can do anything! Either fly into space or go diving.”
“It is no coincidence that all of us, his patients, are jokingly called “Zinen addicts.” He gave us a chance for an ordinary life.
Alenka, for example, does not allow me to stick a disabled sign on my car. And there are children with hydrocephalus who were not registered as disabled at all. They just live like everyone else. Of course, it is impossible to completely relax and not think about the shunt. In any state, I control it with at least the edge of my consciousness.
Didn't you fall? Did you hurt yourself? Doesn't she feel sick? If you feel sick, go straight to the ambulance and the hospital. If a child with a shunt vomits, the first thing we do is rule out problems with the shunt. Everything else is poisoning, infection - later. And yet I try not to get hung up on thoughts about the shunt, but just live. So, I think Alenka should still try to take up music: she has perfect pitch.”
Head shunt surgery for hydrocephalus in Moscow
Yusupov Hospital is a modern medical institution equipped with high-quality and high-precision equipment. At the neurology clinic, which is part of the Yusupov Hospital, you can undergo a comprehensive examination and begin treatment for the disease.
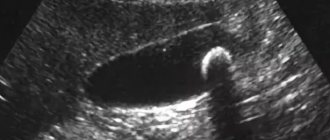
Diagnosis of hydrocephalus in the neurology clinic of the Yusupov Hospital includes magnetic resonance or computed tomography; in complex cases, additional studies are performed to determine the rate of cerebrospinal fluid production.
Brain shunting for hydrocephalus, the consequences of which develop as a result of non-compliance with medical recommendations, requires the patient to stay in the clinic. The Yusupov Hospital has created comfortable conditions for patients: the wards are equipped with modern equipment, wireless Internet, and daily monitoring of the patients’ condition is provided by qualified medical personnel. Customer service at the Yusupov Hospital is provided at the European level.
The high professionalism of doctors and the use of modern equipment for treatment and diagnosis allows us to achieve serious results in the treatment of patients at the Yusupov Hospital with hydrocephalus. You can visit the clinic at a time convenient for you without queues or long waits; to do this, you need to make an appointment by calling the clinic.
Dmitry Zinenko: hydrocephalus is a mysterious disease
– Hydrocephalus is the most mysterious disease of the central nervous system, which still does not have a generally accepted definition. But, despite this, we have learned to cure hydrocephalus,” says Dmitry Yuryevich Zinenko, head of the department of neurosurgery at the Research Institute of Pediatrics. – If you treat it on time and adequately, then it goes away without consequences for the child.
– Can I play sports?
– Children live full lives. True, it must be said that the cause of hydrocephalus can be: hypoxia, hemorrhage, trauma, infection and other diseases that are accompanied by brain damage, which determines the severity of the child’s condition, and not hydrocephalus as such. But it is hydrocephalus that can be recognized in a timely manner and adequately treated.
– Can specialists “overlook” it?
– Hydrocele of the brain is most often diagnosed in children under one year of age. It always occurs with increased intracranial pressure, which has clear manifestations: a rapid increase in head circumference, swollen veins on the head, and a swollen fontanel. A bright picture, impossible not to notice. If we talk about diagnostics, then more often we are dealing with overdiagnosis.
In 90% of cases, the diagnosis of “hydrocephalus” is made where it does not exist.
But when the patient has a shunt installed, then other problems appear. More often we encounter, on the contrary, an underestimation of the severity of the child’s condition. The pressure becomes low, not high. And this further hinders the child’s development.
Sometimes you have to deal with the following opinion: they installed a shunt, the ventricles got smaller – and that’s good. And if the child still cannot stand upright, this is perceived as a natural manifestation of the disease itself.
But in fact, if the ventricles have become smaller, this is a disaster. The head has stopped growing - this is a disaster. A child cannot stay upright for a long time - this is a disaster. These are all signs that the shunt is working too well. It is necessary to change the shunt and reduce the outflow of fluid. To save money, shunts are generally installed, which do not meet all the needs of the body.
- Poor quality?
– How can I tell you... You can buy a Zhiguli. Good car. But she has her limits. Or you can buy a Mercedes. It has more opportunities and higher security. But the price is different. That's how it is with shunts. Unfortunately, fixed pressure shunts are such “Zhiguli”. They are available, but lead to a huge number of complications. It's like a faucet that is always open to the same flow of liquid, which may not be suitable for a particular child.
You need to immediately install a programmable shunt. Then we can regulate the outflow of fluid for each child individually without repeated operations. They are expensive, but in the long run they avoid many complications and would be cheaper overall for the health care system. And most importantly, it’s safer for the child.
– You operated on little Matvey together with the famous Indian surgeon Sandeep Vaishya, when you reduced the volume of his head, a consequence of hydrocephalus. Was this a unique experience for you?
– Of course, any exchange of experience is priceless. We also perform such operations, but it was useful to work with an excellent surgeon, see his technique, and discuss approaches. This operation is exclusive today only because such large heads have become rare these days. Hydrocephalus can be successfully treated in the early stages. You don't have to wait until your head gets that big.
Birthday head: volunteer surgeons treat orphans with hydrocephalus
Hydrocephalus - early help as a chance for a normal life!
Neurosurgery Tags: hydrocephalus
Vladimir Semenov:
The ProVozrast program is on air, I’m with you, Vladimir Semyonov. The topic of our today's program: “Hydrocephalus. Early help as a chance for a normal life." Our guest is Kirill Dmitrievich Shevchenko - Candidate of Medical Sciences, neurosurgeon at the National Medical Research Center for Neurosurgery named after. N.N. Burdenko.
Kirill Dmitrievich, hydrocephalus is a name that probably few people have heard. It is completely medical; many people know it as dropsy of the brain. Today we will pay great attention and understand what hydrocephalus is and the causes of its occurrence.
Kirill Shevchenko:
Yes, indeed, the old name for hydrocephalus is hydrocephalus, it is still used by neurosurgeons and neurologists, especially in Russia. By hydrocephalus, we, doctors, understand an increase in the volume of the ventricles of the brain as a result of impaired cerebrospinal fluid circulation. In simple terms for a wide range of listeners, this is an excessive accumulation of cerebrospinal fluid in a person’s head for various reasons. Cerebrospinal fluid is present in all people, and not only people, in the brain and spinal cord, and it is the increase in its amount, accompanied by characteristic symptoms, that is called hydrocephalus or dropsy of the brain.
Vladimir Semenov:
What are the main causes of the disease?
Kirill Shevchenko:
The reasons for the development of this disease are extremely different. It is probably worth turning to the classification of the disease. There are several main determining factors by which we classify this disease. The first and most basic is the occurrence of hydrocephalus due to the etiology of the disease. This is dropsy associated with hemorrhage, that is, posthemorrhagic dropsy associated with a previous infection of meningitis, encephalitis, meningoencephalitis, and so on, associated with tumors in the cranial cavity and generally within the central nervous system, as well as dropsy associated with developmental defects of the central nervous system systems. The second point is the time of origin factor. There is a distinction between dropsy, which arose at the stage of human development, at birth, it is called congenital, and there is acquired dropsy, when it arose in a person during life.
What stands apart here is the situation when we cannot find out any indications of the congenital nature of the disease, nor any reason that could serve as a reason for its development by an already formed person in childhood, adolescence or adulthood. In this case, the term “idiopathic hydrocephalus” is applicable; it is typical for absolutely all age groups. Previously, it was considered more characteristic of older patients, over 60, and appeared under the term “idiopathic normotensive hydrocephalus,” as most doctors know it and patients often encounter it. Now this is only a component of the general concept of idiopathic hydrocephalus in adults.
Vladimir Semenov:
Are there species and subspecies in the classification?
Kirill Shevchenko:
Yes. The next factor on the basis of which the choice of treatment method is determined, in addition to the actual cause of hydrocephalus, is its nature, namely: there is occlusion, that is, an obstacle to the circulation of cerebrospinal fluid within the ventricles of the brain, or not. That is, communicating dropsy is either non-communicating, or non-occlusive and occlusive in a different way. Based on this, treatment tactics, prognosis, and so on are built.
Vladimir Semenov:
Are there those who are more susceptible to this disease? At-risk groups?
Kirill Shevchenko:
We talked a little about this at the very beginning of the conversation, when we talked about the reasons, when I talked about hemorrhages in the cranial cavity and so on. The risk group includes patients with a history of hemorrhage in the cranial cavity, namely: rupture of an aneurysm, venous malformation, so-called cerebral hemorrhage. When blood leaks into the cranial cavity, about one-third of patients develop hydrops, 25 to 30%. Next are patients with traumatic brain injury, and here the indicators vary, according to some literature data they range from 1 to 90%. But, on average, it is believed that one fourth to one third of patients after a traumatic brain injury develop post-traumatic hydrocephalus. The next point is infection, that is, meningitis in a high percentage of cases also leads to an imbalance between the production of this fluid and its absorption within the nervous system, which may require treatment of this condition. I’m not talking about the pediatric group of patients now, we’re talking more about adults, I deal more with adult patients. The last point, which we have already talked about, is the idiopathic form of hydrocephalus, when the cause is not clear, but recent data indicate that in the pathogenesis, precisely in the mechanism of development of this form of the disease, arterial hypertension and cardiovascular pathology in general are important. That is, in patients suffering from arterial hypertension and various diseases associated with hypertension, with pathological conditions in the brain, the frequency of detection of idiopathic normotensive hydrocephalus is significantly higher than in patients who do not suffer from arterial hypertension.
Vladimir Semenov:
Do we have statistics in our country, for example, do men or women get sick more often, or a certain age group? Or is there no such thing?
Kirill Shevchenko:
To be honest, there are no such statistics. A number of institutions keep their statistics, where the majority of such patients are concentrated, but in our country it is not possible to say that exactly this percentage of the population suffers from this form of the disease. I can say that in Europe, Germany, also in Japan and America, data were presented that about 4-5% of patients over 60 years of age suffer from idiopathic normotensive hydrocephalus without indicating gender. But, men and women suffer from the disease approximately equally.
Vladimir Semenov:
This question is: could frequent headaches indicate that hydrocephalus may be developing?
Kirill Shevchenko:
Yes, indeed, and not even just frequent headaches. Everyone has a headache, every person has had a headache at least once in their life: for some it hurts more often, for others it hurts less often. The following fact applies here: an increase in frequency or change in the nature of headaches is a cause for concern and a reason for examination. That is, if a person had a headache for 5 years, had reactions to the weather, or suffered from migraines every 2 months, and for the last 3 months he has had a headache 3-4 days a week out of seven and the pain is of a different nature - bursting, pain accompanied by nausea, then at a minimum, they are an indication for a study of the brain in order to exclude a problem associated not only with hydrocephalus, but generally associated with any pathological process in the head.
Vladimir Semenov:
Are there diseases that can later lead to the disease we are talking about today?
Kirill Shevchenko:
Yes, of course, there are such people. Again, I repeat: these are mainly pathologies of the central nervous system, ruptured aneurysm, infection of the central nervous system, traumatic brain injuries, various tumors, and general volumetric processes. Now I am not taking an aneurysm or other vascular pathology, I am taking specifically oncological benign and malignant tumors that cause an obstruction to the circulation of cerebrospinal fluid. They can be accompanied by hydrocephalus, of course.
Vladimir Semenov:
If a person is in pain, he comes to the doctor at his place of residence at the clinic. Who can determine which doctor? After all, an ordinary therapist is unlikely to be able to determine; he should probably redirect to another doctor in the clinic. Who can determine whether a person is already developing a disease or not? How does the process of redirecting a person from a regular clinic, for example, to you happen?
Kirill Shevchenko:
There is probably no algorithm for patient referral; Most patients turn or are referred by doctors of other specialties to our neurologist. Headache and dizziness, gait disturbance and other neurological symptoms - as a rule, doctors of various specialties refer the patient to a neurologist. More often it is a neurologist, especially if the situation is not urgent or emergency. A person turns to a neurologist, the neurologist looks at the symptoms and, as a rule, refers the patient to a brain study - MRI, CT scan of the brain, or others. Then, if the radiologist finds changes that frighten him, or he sees that they belong to the neurosurgical spectrum of pathology, then a consultation with a neurosurgeon is recommended in black and white. How does a patient get to this or that doctor: either he goes to the clinic at his place of residence and the institution is recommended there, or he reads on the Internet, or he comes to this or that doctor in various ways.
Vladimir Semenov:
Is it possible to confuse this disease with others? Are there any similarities in symptoms or anything else?
Kirill Shevchenko:
Yes, of course, there are similarities in symptoms. As we said, headaches can have different causes. Everyone has a headache, and it in itself is not always an indication for surgery or surgical treatment. Hydrocephalus may not manifest itself with a very wide range of symptoms. Young people are characterized by headaches, dizziness, nausea, and sometimes vomiting, if the situation is accompanied by increased intracranial pressure and so-called occlusive attacks. There may also be a decrease in memory for current events, a decrease in attention, that is, patients do not remember information that was just received - they met someone and immediately forgot, they were told something, some information, they cannot reproduce it. This is more typical for young people. Older people and those over 60 tend to experience gait disturbances. A change in gait like a shuffling one, as if the legs are pulled to the floor by a magnet, as patients describe, they shuffle, walk in small steps. This also includes urinary disturbances such as incontinence, and less often memory impairment is also associated. That is, the patient can also be disoriented in time, place, even in the personal situation in severe cases.
Diseases such as Parkinson's disease, Alzheimer's disease, and a number of other neurodegenerative diseases, some of which can be treated surgically, some cannot be treated surgically, can exhibit similar symptoms, especially in older people. Often these diseases occur together. For example, in a patient diagnosed with Parkinson's disease who is receiving specific drug therapy, an examination of the brain reveals dilated ventricles. The symptoms are very similar; in some cases, antiparkinsonian medications help, in others they do not. When we see dilated ventricles against the background of an incomplete effect of drugs, we suggest that the patient undergo a certain additional examination, do a manipulation that will show whether the dilated ventricles affect the state of his health, whether hydrocephalus affects his health. It often happens that it really does have an effect, and the subsequent operation, if the patient agrees to it, allows one to either get rid of the diagnosis of Parkinson’s disease, parkinsonism, so-called. The symptoms go away, the person begins to walk smoothly, his urination is restored, it even happens that the tremor goes away, there are such cases. Or the operation allows you to reduce the number of drugs that the patient receives, which, undoubtedly, cannot go unnoticed. Everyone knows that in Parkinson's disease, the effect of specific drugs is gradually suppressed; over time, an increase in dosage is required and ultimately they stop helping. Neurologists and surgeons are always happy that the effect of the operation has come and the symptoms have either disappeared or significantly decreased, and the need for drugs has decreased.
Vladimir Semenov:
Does hydrocephalus always mean surgery? Or is it possible that drug treatment will be possible and surgery will not be necessary in the future?
Kirill Shevchenko:
To be honest, in my practice I have seen very few cases when patients just receive medications and move on with their lives. They can be counted on the fingers of one hand, namely adults with newly diagnosed dropsy. Quite often we have to consult and communicate with patients who have suffered from hydrocephalus since childhood; these are approximately patients born in the late 1990s - early 2000s.
Vladimir Semenov:
Why such statistics?
Kirill Shevchenko:
This is not a statistic, just an observation. I don’t know for what reasons, but the patient, a small child, was diagnosed with hydrocephalus at birth, but no surgical treatment was performed. Previously, they mostly performed a shunt, bypass surgery. There was no treatment; patients were prescribed diuretics, on which they lived for literally years. That is, for 10–15–20 years a person periodically or regularly took diuretics, and this, in general, was the end of the treatment. Over time, they stopped helping, symptoms began to progress, and patients sought surgery. There are such cases of conservative treatment, but in fact, drug therapy in the case of hydrocephalus only helps the patient endure and survive until surgery.
Vladimir Semenov:
It turns out that there is no prevention of this disease? How to protect yourself from the disease?
Kirill Shevchenko:
When we know the cause, hemorrhage from an aneurysm, and so on, then as a preventive measure for the disease, after a certain age it is necessary to undergo a brain examination for aneurysms, monitor blood pressure, and in case of infectious diseases, treat them promptly and adequately so as not to get meningitis or encephalitis. Avoiding traumatic brain injury is understandable; some people can do it, others cannot. Prevention here means trying to prevent the development of these conditions. But, we may not know the reason. Let's say a young guy was living, studying, playing sports, and suddenly his head began to hurt. It hurts for a day, two, a week, a month, also nausea, vomiting, vision began to decline. They take pictures and find that the patient has large ventricles and severe hydrocephalus; the reason is unknown, you can’t influence what you don’t know.
Vladimir Semenov:
A neurologist refers you to the operation, consults with a neurosurgeon and then prescribes the operation. This can be done under compulsory medical insurance, as I understand it?
Kirill Shevchenko:
Yes, in our country the operation is either carried out according to a quota or within the framework of compulsory medical insurance.
Vladimir Semenov:
If possible, tell us what happens during the operation?
Kirill Shevchenko:
Yes, sure. But, before I tell you, I’ll first briefly go ahead and say that with hydrocephalus, it is possible either endoscopic intervention or a shunt, shunt operation, installation of a shunt system, in fact, a foreign body in the body, in order to remove cerebrospinal fluid from the brain beyond its boundaries . Both interventions are carried out under anesthesia, that is, the person sleeps and does not feel anything. In terms of duration, the operation takes from 1 to 2 hours, I mean from bringing the patient into the operating room to leaving it, with all the preparatory measures, the operation itself, and so on.
In endoscopic surgery, its variant is mainly used - endoscopic ventriculostomy, namely, making a hole in the bottom of the third ventricle, one of the cavities of the brain, in order to direct the flow of cerebrospinal fluid bypassing the place where it cannot pass, in a bypass. . In this case, the hair in the frontal area is shaved off, a small incision is made in the skin and soft tissue, about 3 cm long. A small hole is made in the skull, about a centimeter in diameter, no more. An endoscope is inserted through the resulting hole in the cavity of the brain ventricles, then advanced into the third ventricle and using special micro-instruments, a hole is made in the bottom of the third ventricle. Some modifications of these operations are possible, depending on the location of the obstruction. There are different options for the occurrence of obstructions in the brain, and in some cases the operation is complemented by manipulations somewhat deeper than the bottom of the third ventricle, but this is already a feature, in principle, the essence of the operation does not change. For the patient, one incision is also left on the head within the scalp.
Vladimir Semenov:
Kirill Dmitrievich, when is bypass surgery performed, and when is endoscopy?
Kirill Shevchenko:
Yes, a very good question, patients very often say: we want endoscopy. The Internet is accessible to everyone, the information is there, and most patients want to do without a shunt; almost everyone immediately wants an endoscopy. There is a subtle point here, returning to the causes of hydrocephalus. If a person had hemorrhage in the cranial cavity, there was an injury accompanied by hemorrhage, or there was an infection, then endoscopic operations are almost ineffective; there is a very low percentage of effectiveness, and there is no need to give any guarantees to the patient that the operation will work. We do not recommend performing endoscopic operations in these cases.
Vladimir Semenov:
You can do an endoscopy, but in the end... Or do you immediately say that no, endoscopy is not suitable here?
Kirill Shevchenko:
We say that it is theoretically possible, but the likelihood that this operation will help you is extremely low. We try to offer the patient possible treatment options with a prognosis, that is, how likely this or that operation will help. The patient himself chooses how he will be treated. We can say: “This is the forecast, but, frankly, I don’t recommend it. You can choose. Formally, you can choose, at least if one operation does not work, there will be a second operation. If you are ready to try, please do so.”
Returning to the reasons. As I said, for the stated causes of dropsy, as a rule, endoscopic surgery is extremely ineffective. Basically, they install shunts, whatever they are, but a shunt. With idiopathic hydrocephalus, there is an obstruction, there is an obstruction to the outflow of cerebrospinal fluid or there is none within the ventricles of the brain. So, if there is an obstacle, then in most cases, in 95–98%, endoscopic surgery will be effective, at least in the near future. I can’t talk about the delayed perspective, because we don’t have a situation where a patient comes all his life and gives information about himself to a medical institution. I can say that during a 5–7-year follow-up, the so-called follow-up of patients for 5–7 years, with adequately selected indications for surgery, when treatment tactics are correctly determined, in 95–98% of cases endoscopic operations are effective.
When there is no obstruction, that is, communicating hydrocephalus, not obstructive, then in most cases we cannot offer anything other than shunt surgery. Why in most cases, because there is one form of hydrocele that is considered communicating, but there is obstruction outside the ventricles of the brain. Then we can also offer patients endoscopic surgery, which will have an effectiveness of about 80-85%. But, given that young people more often suffer from this form, for them the absence of a shunt in the body and the effectiveness of the operation are quite relevant. But this is a rare situation, I don’t think it’s worth discussing in detail. When hydrocele is communicating, we cannot offer the person anything other than a shunt.
Bypass surgery is also performed under anesthesia: the person sleeps and does not feel anything. There are cosmetic nuances: half the head of hair is shaved, in some cases the entire head is shaved. Since insertion of a foreign body is associated with higher risks of infection, the risks should be minimized. Hair is a part of the body that carries infectious agents; therefore, half a head of hair is removed within the surgical field. For many this is important. Someone puts on a wig, someone changes their hairstyle, but, in general, that’s a different question. Next, several small incisions are made, two of them, usually on the head, one on the anterior abdominal wall, on the abdomen, near the navel, if we are talking about implanting a shunt into the peritoneal cavity. Let me emphasize: here the shunt is not implanted either in the stomach or intestines; the shunt is simply immersed in the abdominal cavity. That is, its end is located between the organs, it does not penetrate into any organ, is not immersed, nothing is opened. There is a fairly widespread opinion that the shunt is placed in the stomach - no, the shunt is simply placed in the abdominal cavity.
The second option - some doctors prefer it, we use it as a backup option - is to immerse the second part of the shunt into the venous bed, namely into the lumen of the jugular vein, facial vein and subsequently into the jugular vein, and then it is installed near the atrium. This type of operation has a right to exist. Why do we use it as a backup, because in some cases a person cannot be implanted into the abdominal cavity if she has had many operations on the abdomen, peritonitis, and so on. In this case, the function of cerebrospinal fluid absorption by the peritoneum is impaired and the operation will simply be ineffective. For such patients, a shunt is placed in the venous bed, and a small incision is made in the neck in the appropriate projection.
Vladimir Semenov:
After the operation is completed, time passes. Is there rehabilitation and is the patient registered somewhere? You said that you don’t come as often, perhaps as the doctor would like, to track and have statistics on how and what is happening with the patient.
Kirill Shevchenko:
In general, patients are recommended to be monitored by a neurologist and neurosurgeon. We cannot tie a patient to a specific institution, to a specific doctor, since people can be from Kamchatka, from the north, from the south of the country, from everywhere, and not everyone can afford, both for time and financial reasons, to come for a consultation in Moscow . If there is a doctor who can adequately answer the patient’s questions at his place of residence, of course, please, we don’t mind, we understand everything. Of course, we are interested in having information about the people we operated on, at least the key points, stored in our database, in our system of medical records, in our archives, so that in the future we can make predictions about our treatment, perhaps find new treatment paths, perhaps new approaches, perhaps changing indications for operations, perhaps setting additional contraindications. This all matters, of course, but it is what it is.
Vladimir Semenov:
Does it happen that after surgery a repeat operation may be necessary? Were there such cases?
Kirill Shevchenko:
Yes, such cases occurred both after endoscopic and bypass operations. There are cases that endoscopic surgery either did not bring any effect, or the positive effect regressed in the future. The reason may be the closure of the hole that we made in the bottom of the third ventricle, although this is a very rare situation, I have only encountered it once in my practice. The second point is when a person’s symptoms return, we take pictures, formally according to MRI there is a hole, cerebrospinal fluid circulates through it, we can see this from specific signs on the images, and the symptoms return. In this case, the question arises: either offer the person a shunt, or he agrees to continue living like this, as long as possible, until the symptoms become so pronounced that he cannot live with them any longer. This is what concerns endoscopic operations.
As for shunt operations, let's start with the fact that a shunt is a foreign body, I repeat. This is a tube with a valve, it can be of different brands - Russian, American, German, and so on.
Vladimir Semenov:
Does the shunt have a lifespan?
Kirill Shevchenko:
There are, of course, but I saw completely different situations. I saw people who walked for 30 years with one shunt, I saw people who went through one year and dysfunction arose. There is an opinion here: a shunt is a foreign body, it can break, in simple terms, it can become clogged with all sorts of different components of the cerebrospinal fluid, protein, or become overgrown with tissue in the brain and stop functioning. It can simply open up, that is, over time the material undergoes changes, especially in a living organism. It happens that its rigidity and elasticity change. A person lived, say, 5-7-10 years, everything was fine, he made some sudden movement and after a few days or weeks symptoms began. We take pictures, an X-ray of the shunt, and see that it has opened in one of the places along its length. Then reoperation is needed, from the banal restoration of integrity through a small incision under local anesthesia to the replacement of the entire shunt, if the reason why it somehow does not function properly is not clear.
Vladimir Semenov:
How does a patient’s life change after bypass surgery? Lifestyle, nutrition, sports - are they possible after bypass surgery, are there any prohibitions, at least briefly.
Kirill Shevchenko:
I will say right away: nutrition does not affect the shunt in any way, people can eat and drink whatever they want, absolutely. Regarding lifestyle in general, I constantly give patients a recommendation: that you should live the way you want to live, the way you lived before, including sports. Yes, after the shunt we recommend limiting strenuous physical activity, including sports, for approximately 2-3 months. The wounds must heal, a scar must form at the site of insertion into the abdominal cavity, because playing sports usually means an increase in intra-abdominal pressure. The abdominal wall defect must close, everything must close tightly, otherwise there may be a hernia, there may be externalization of the shunt, that is, the shunt may jump out of the abdominal cavity. Everything should be overgrown there; according to our considerations, it will take about 2–3 months. After this, patients who were involved in sports continue to exercise; maybe not professionally, as before, but in a supportive manner, for themselves, for their health, most patients engage in and continue to live a normal life.
Vladimir Semenov:
What are your recommendations as a neurosurgeon? What do you recommend to healthy people who are not sick, or who have already suffered from hydrocephalus?
Kirill Shevchenko:
I would recommend not to despair, first of all. There are treatment options. You can live with this, the treatment has been worked out. When you can help, then you can help.
Vladimir Semenov:
The main thing is on time, perhaps?
Kirill Shevchenko:
Yes, you can’t ask for help when you’ve stopped walking and the person is lying in dementia and doesn’t understand anything. There is such a feature: the more pronounced and more symptoms before surgery, the worse the prognosis for a person’s recovery. Therefore, the recommendation may be to seek help in time if such a situation occurs. I repeat that surgical treatment has been worked out. Yes, we cannot always offer it to people, because there are situations when surgery is not indicated or contraindicated, but most patients who apply can undergo surgery. They tolerate it and, with adequately selected indications, it helps them.
Vladimir Semenov:
Thank you very much, Kirill Dmitrievich!
Kirill Shevchenko:
Thank you
Matvey: waiting for his mother
Matvey's head grew so large from hydrocephalus that until he was three years old he could not even lift it. No, not by oversight. Yes, the young 17-year-old mother abandoned him immediately after giving birth. But the caring hands of Elena Evgenievna Shatskaya, the head physician of that institution for orphans in the Ryazan region, who accepted Matvey, and her colleagues did everything possible for him. And even the impossible. Bypass surgery, shunt testing, replacement. Everything was complicated by a congenital brain defect.
When the capabilities of regional neurosurgeons were exhausted, Elena Evgenievna reached the federal ones. And now a unique operation to reduce the head (cranioplasty) of three-year-old Matvey was performed in two stages by the best Russian neurosurgeons together with the invited Indian surgeon Sandeep Vaisha.
After the first operation, the baby turned over on his stomach, and after the second, he began to get up on all fours and raise his head.
Today, 4-year-old Matvey can sit down on his own and remain in a sitting position for quite a long time. This means that now he eats and walks while sitting. His diet has expanded (it turns out he loves bananas and strawberry curds), his visibility has increased, and new emotions have appeared.
– Even such a difficult combination of diagnoses is not a reason to “give up” on a child. We cannot guarantee him the ordinary life of an ordinary baby, but we can improve the quality of his life, give him a chance, and use the rehabilitation potential that he has. I don’t know if he will study in a regular school, but there is hope that he will go!
Our most important worry is that in a year we are obliged to transfer our smiling boy to a boarding school for children with severe mental retardation. But if only he had a family! We would be very happy to provide them with all our rehabilitation opportunities,” Elena Evgenievna dreams. “I’m sure he will make someone’s parental happiness!”
Disability - valid or not?
After we returned home after the operation, the neurologist at our place of residence advised us to apply for disability. It sounded like another sentence, they even thought about refusing, but in the end they decided - let it be. Moreover, quite a lot of money was spent on rehabilitation, massages, and paid doctor’s appointments, and the pension was not superfluous.
We were granted disability for a year, but not because of bypass surgery, but because of postoperative developmental delay. The commission warned that during recertification in a year, if the child begins to walk, it will be removed. What we still really hope for to this day.
Hydrocephalus: symptoms
If you notice the following symptoms in your little child:
– rapid increase in head circumference, – enlarged and swollen fontanel, – pronounced venous pattern on the forehead and face, – oculomotor disorders (strabismus, setting sun symptom, congestion of the optic nerves), – if the child does not hold his head up, throws it back, – eats poorly, sleeps poorly, cries often -
Contact a neurologist immediately! Time in this case can work against you!
Your actions:
STEP 1. Get a referral from a neurologist for an examination (MRI or CT). All examinations are carried out within the framework of compulsory medical insurance! MRI is performed free of charge for young children; the examination is performed under general anesthesia in a day hospital.
STEP 2. Contact a neurosurgeon with the results of the examination. If there is no neurosurgeon in the region (or to get a “second opinion”), send the results of the examination (MRI image) for an online consultation at a specialized clinic (the consultation is free, the contacts of medical organizations are in the memo) or to the post office of the municipal non-profit organization “He Needs You” marked “for consultation”
STEP 3. The hospital conducts an absentee medical consultation based on the medical documents you provided and, if hospitalization is necessary, prepares a voucher for you, which will indicate the date of hospitalization, a list of tests for the child and accompanying person, doctor’s contacts, hospital address and other important information.
STEP 4. When a diagnosis of Hydrocephalus is made based on MRI results, surgical treatment is performed. The method of surgical intervention is determined by the neurosurgeon depending on the type of disease.
Varenka: the suffering was associated with the shunt
– Even as a child, I knew that I would have a son, Stepka, and a daughter, Varenka. But somehow it didn’t work out,” says Elena Kirina from the city of Sortavala (Karelia). My husband and I did not have children for seven years. They were examined and treated. Finally they told me that I was pregnant and had twins, I fell to the floor with joy and began to cry. And then at 14 weeks, on an ultrasound, it became clear that Varyusha has Dandy-Walker syndrome, the cerebellum is not developing and she most likely will not survive, and if she survives, she will become disabled. They offered us an abortion, but Styopka could have been harmed during the abortion. And in general, I have always been against abortion. We decided to give birth. I cried for the rest of the pregnancy. At 33 weeks labor began. They performed a caesarean section. I didn’t see Varya at all - she wasn’t breathing, they immediately took her away.
On the 9th day, Varya began to develop hydrocephalus. At three months she had her first shunt installed. But the girl suffered. In total, she underwent eight surgeries. Her shunt was clogged and her cerebrospinal fluid was infected. In essence, she was doomed. She spent a whole year in hospitals in Petrozavodsk and St. Petersburg. And Lena, who could not leave Stepan for long (he also had health problems), spent more time on the road this year than with her daughter.
“I had a small child at home, and I cried endlessly and wanted to strangle myself. Because my other child was dying alone in the hospital.
The problem was that Varya was kept in the infectious diseases department, believing that her symptoms were a consequence of the virus. And her suffering was associated precisely with the shunt.
Today's day
Now my son is already 1.2 years old. It develops, of course, with a delay. But neurologists say that under our conditions (prematurity and repeated anesthesia) this is normal. At the moment he is crawling, standing at the support, and slowly starting to talk. In general, almost like all children. The shunt does not particularly affect his life - the only thing is that we do neurosonography every 2 months. In the future it will be less and less frequent.
Unfortunately, at 9 months he had to undergo another surgery due to shunt dysfunction. Usually this happens no earlier than after 2-3 years, but we were unlucky - the valve in the head stopped letting fluid through due to the fact that the vessels were tightly intertwined with it. But now everyone in our family knows how to identify dysfunction. The main signs that made you worry:
- vomiting, 2-3 times a day;
- the child became lethargic and slept almost all day;
- He often cried, as if something was beginning to hurt him greatly.
All this lasted two days, on the second day we went to do neurosonography.
She showed that the ventricles were enlarged. Moscow and the second operation awaited us again. Author of the article: Anna Shershova.
Have questions? Write in the comments!
Shunt dependent
When discharging a child from the hospital, you must insist that the brand, model of the drainage system (shunt) and pressure level (in the case of programmable shunt models) be included in the discharge. This is vital in emergency situations (eg shunt dysfunction) and when measuring pressure if overdrainage is suspected. Each programmable shunt has its own pressure setting system!
Not all types of shunt can pass through metal detectors. The drainage system settings may fail.
Avoid overheating (baths, long exposure to the sun), hypothermia, head injuries, electromagnetic treatment. Every time a child has been exposed to intense magnetic fields, check the pressure level setting of the valve.
Do not massage the head, neck and abdomen area.
If the drainage system is not functioning well, signs of shunt dysfunction appear, which are manifested in the following symptoms: increased intracranial pressure, headaches, nausea, vomiting, decreased level of spontaneous activity.
If you have a fever in combination with other suspicious symptoms (vomiting, lethargy), immediately contact a neurologist or neurosurgeon!
Varenka: they weren’t the ones who pulled them out!
When Lena brought her Varya home to Sortavala one year ago, and she was admitted to their local hospital, the doctors threw up their hands in bewilderment:
“We’ll lie down and watch.” - You mean die? - Well, yes.
And then Lena realized that she couldn’t just wait for her daughter to die. She called a paid ambulance and rushed to St. Petersburg. And from there by train, with Varya in her arms, to Moscow. “She will die on your way!” - they told her goodbye at the hospital. But she found a paid doctor who would accompany her and went.
She already knew that in Moscow there was Dmitry Zinenko, for whom hydrocephalus was not a death sentence or a horror story.
“And they weren’t the ones who pulled it out,” said Dmitry Yuryevich, looking at Varya, whose head weighed four kilograms out of six kilograms of total weight.
In Moscow, Vara was fitted with a new shunt, brought into the atrium, and later into the abdominal cavity. And the girl came to life. Lena and Varya completed two courses at the St. Petersburg rehabilitation center. And after the first year, Varya began to raise her head. And a year later she began to roll over, crawl, sit up and walk along the support.
– The main thing is that we are now at home and all together! – Lena couldn’t be happier.
Three-year-old Styopa, developed for his age, dashingly climbed onto a chair and reached for the paints that his mother had hidden. And now she and Varya are already painting something on the floor. They worked well together - twins.
“The relatives in Var dote on their souls,” says Lena. “And the main thing is that since Varya returned home, we never have quarrels, no one yells at anyone. Unless the children fight with each other sometimes. Well, children!
Postoperative period
After 24 hours in the recovery room, we returned to our unit, where we spent another 10 days. My son was 4.5 months old at that time. It seemed to me that he had some regression in development - before the operation he could almost hold his head up, but after it he could not (and he started quite late, after 1.5 months). The neurologist explained to me that this was not a skill, but rather a disorder, and he did it solely because of increased tone.
For the next 10 days, we were actively monitored, given injections (Cortexin + vitamin B), as well as gymnastics (a massage therapist came and did 10 minutes). The child felt good, as if even better than before. Dad, who came to visit, recognized and was glad to see him. I ate as usual, my temperature did not rise.
In our case, the head was not greatly enlarged before the operation, but it was somewhat deformed in shape and stretched back. Therefore, after the operation, the doctors told me to use bolsters so that my son would lie on the back of his head. The method, by the way, turned out to be very effective, now he is 1.2 years old and there are no external signs that he has hydrocephalus, the size and shape of his head is normal.
After 10 days, we were discharged with a recommendation to undergo rehabilitation courses for up to 1.5 years every two months. What we did responsibly, in the same hospital. Each time we went to bed for 10 days, we were given injections, massages, and physiotherapy. It seems like a little, but after each course there was a leap in development.