Science news. Myelination and its early diagnosis
What is myelin and why should it be measured?
Myelination of nerve endings is the formation of a special layer of substance called “myelin” around the axial cylinder of the nerve fiber during its maturation. It's like insulating a wire. This amazing process begins at the 5th month of intrauterine development of the fetus and basically ends at the end of the second year of the child’s life. According to some data, the process of myelination continues until adolescence, and sometimes up to 40 years of age. Myelin, which covers nerve endings, increases the speed and accuracy of impulse transmission in the nervous system and protects nerve fibers from damage. Therefore, its deficiency causes various disorders in the functioning of the nervous system.
Russian neuroscientists are working on introducing a new approach to diagnosing the quantitative level of myelin. It consists of identifying biomarkers of maturation or damage to the nervous system of the body of children, including in the fetus from the 20th week of intrauterine development. These studies will provide invaluable assistance in the prevention of perinatal mortality and death of newborns. Detection of myelin levels will also be of great importance in preventing the development of severe diseases and defects of the central nervous system (CNS), cognitive disorders, including such a common disease today as early childhood autism.
From the history of the issue
It should be noted that the world's first non-invasive (bloodless, without penetration into the body and forced damage) method for assessing myelin was developed several years ago under the leadership of Tomsk State University and Washington University scientist Vasily Yarnykh. The new approach has already proven its effectiveness and is being implemented in several clinics in the Russian Federation. This method has become a great help for determining damage to nerve fiber sheaths in people who have suffered a stroke...
...And within the framework of the new project, a unique approach will be used to assess myelination in normal conditions and in various pathologies of the brain, both during the period of intrauterine development of a child and after his birth.
The essence of the new project
Myelination of nerve fibers is clearly visible in the picture obtained using magnetic resonance imaging (MRI). But MRI in the prenatal period (the period of intrauterine development) is an almost impossible task, since the fetus cannot be motionless for any period of time during the scan.
Therefore, to obtain an objective picture, special programs are used that allow combining MRI images (the so-called “Method of mapping the macromolecular proton fraction”) obtained against the background of fetal motor activity. The new method has already been tested in examining children in the first years of life and fetuses during intrauterine development. New data have been obtained on the features of the development of fetal brain structures at different stages of intrauterine development.
Thus, it has been established that the amount of myelin in the fetus in the second trimester (13-24 weeks) is still minimal. And first of all, it is formed in structures that are responsible for vital functions - breathing, blood circulation, cardiac activity.
But in the third trimester (25-40 weeks), the initial myelination of the structures responsible for movement and their coordination becomes noticeable.
When examining children 2-3 years old with pathology of the nervous system, a number of cases were identified where the new method helped to obtain additional diagnostic information that was very important for doctors.
Benefits of the new method
These studies are supported by the Russian Science Foundation and will be carried out for another three to four years. They will allow us to develop the technology for quantitative mapping of myelin in the prenatal period and the period after the birth of a child. Based on the results of the study, a normative quantitative digital atlas of fetal and child brain myelination, necessary for doctors and scientists, will be created.
The data obtained will provide doctors with additional information about the causes of developmental delays in children and will be useful for predicting their cognitive and intellectual abilities.
Prediction or diagnosis of incipient myelination disorders at an early age is also important from the point of view of identifying risk groups of patients with mental retardation, autism and other serious mental illnesses.
Such information can be used as a proactive preventive method: to prescribe early behavioral therapy and develop social adaptation skills.
What to do until this unique technique becomes widespread?
Only preventive measures!
Our center carries out a great deal of work on the prevention and early correction of developmental disorders in young children.
Expectant mothers receive information about the specifics of caring for a newborn at perinatal risk and its early development.
We work with young mothers to anticipate the pathological process in the baby from birth, when the changes are not yet visible to anyone. Parents sometimes do not believe in the possibility of developmental disorders in their baby, because “there are no manifestations yet.” And they miss precious time that you will never get back!
Our methodology of advanced and corrective development is aimed at stimulating the formation of age-related skills, the development of the motor , sensory , speech , communicative and emotional spheres of the child from birth. There's still time! After all, the myelin sheaths have not yet formed completely and have not blocked the enormous compensatory capabilities of the newborn’s body!
Therefore, thanks to our method, a healthy baby will receive training in all body functions, and a baby at risk of pathology will undergo stimulation of skills, which will restore damaged pathways and stimulate the appearance of new ones.
Magnetic resonance imaging (MRI) in St. Petersburg
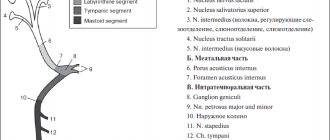
Myelination is an increase in lipid content and a decrease in water content in the membranes of nerve tracts. The process of myelination of the brain begins in the fifth month of intrauterine development and continues actively until 2 years. In MRI of the brain, the signal from the myelinated white matter of the brain, due to the reduction in relaxation times, is clearly different from areas with incomplete myelination.
Since the white matter in a newborn is not yet mature, the ratio of the signal intensity of white and gray matter is the opposite of that of an adult: on T1-weighted MRIs of the brain, the white matter is darker than gray, on T2-weighted MRIs of the brain it is brighter. White matter maturation therefore appears as an increase in white matter signal intensity on T1-weighted brain MRIs and a decrease on T2-weighted brain MRIs. Up to 6 months of age. T1-weighted MRIs of the brain are more sensitive to the process of myelination.
On T1-weighted MRIs of the brain at birth, a normal signal for the adult brain is produced by the posterior portions of the medulla oblongata and midbrain, the cerebellar peduncles, the anterolateral portions of the thalamus opticus, the posterior limbs of the internal capsule, the optic nerve, its chiasm and tract. The process of myelination proceeds from the center to the periphery, from bottom to top and from back to front. By 3 months of life, the optic radiation and cerebellum acquire a high signal, by 4-6 months - the corpus callosum, 7-11 months. – white matter upward from the centrum semiovale, from 8 to 12 months. – maturation of the subcortical areas of white matter ends at 12 months. - periventricular white matter, myelination of the frontal lobes is completely completed by 11-14 months, temporal - 14-18 months.
On T2-weighted MRIs of the brain, the same process seems to be slower. The low signal typical for the adult brain at birth is produced by the white matter of the posterior parts of the brainstem and the inferior and superior cerebellar peduncles. The entire cerebellum becomes hypointense only by 18 months of age. Between 6 and 8 months the corpus callosum matures, by 11 months the anterior limb of the internal capsule matures, by 14 months the white matter in the deep parts of the frontal lobe matures, and between 18 and 24 months the maturation of the subcortical areas of the white matter ends.
A small area of unmyelinated white matter in adults is sometimes found at the anterior horns and less commonly behind the posterior horns of the lateral ventricles. It reflects slow myelination and is not a pathological condition. Appears as symmetrical “clouds” on T2-weighted MRI of the brain, separated from the horns by a thin layer of normal white matter. This dark layer is important in the differential diagnosis from demyelination, necrosis, or edema that is adjacent to the ventricles. An important feature of tomograms obtained using the FLAIR MRI sequence (inversion - recovery with a suppressed signal from the fluid) is the “emphasis” of the contour of the lateral ventricles. The bright line is thicker around the posterior horns. This should not be mistaken for myelination disorder or myelin destruction.
T2-weighted MRIs of the brain can trace brain maturation not only through myelination, but also through the accumulation of iron in subcortical structures. At 6 months, the subcortical nuclei acquire a low signal. Only by the age of 9-10 years does the globus pallidus, substantia nigra and red nucleus become low in signal, and the intensity of the signal continues to decrease in the second decade of life. The dentate nucleus of the cerebellum begins to darken after the age of 15, and the process occurs slowly throughout life.
When performing MRI in St. Petersburg for children under 2 years of age, we pay close attention to incomplete myelination so as not to miss dysmyelogenous diseases and the consequences of ischemic disorders. The process of myelination is equally visible in high fields and in low fields on open MRIs.
Leave feedback.
09/29/2016 Added by Oleg Zimin
MRI in St. Petersburg, USA
Thanks for the thorough and detailed explanation. If clarification is necessary, I will refer to your email. resource.
business 0.3 MRI in St. Petersburg, USA 5.0 5.0 1 1 Thank you for the detailed and detailed explanation.
If clarification is necessary, I will refer to your MRI in St. Petersburg USA
Epilepsy without seizures in children
Epilepsy is a disease associated with disruption of certain groups of nerve cells. Epilepsy can be congenital or acquired. Sometimes it begins due to damage to the brain due to injury or tumor. It can also be caused by a congenital cyst or other features of the brain structure. It happens that epileptic seizures begin to occur for no apparent reason due to a hereditary predisposition.
Epilepsy in children can manifest as seizures of the whole body or one limb, as well as “off” episodes.
Non-convulsive seizures of epilepsy in children
Epileptic seizures with convulsions are more typical for children from birth to 2–3 years. Children over 4–5 years of age are more likely to have epileptic seizures without convulsions.
The most common non-convulsive seizure is absence, a short-term loss of consciousness. From the outside it looks like the child is “stuck” and lost in thought. The gaze is not focused. During an attack, the baby stops activities (for example, playing, walking, writing) and freezes. At the same time, he can perform stereotypical movements (for example, flexion and extension of fingers).
During an attack, the child does not react to anything, it is impossible to bring him out of this state. After a few seconds (usually from 2 to 20), the attack ends, the child “turns on” again and continues what he was doing before the attack. He doesn’t remember the attack itself.
There can be several dozen such absence seizures per day. Typically, an attack is triggered by hyperventilation caused by rapid breathing. Absence seizures can go unnoticed for a long time even by the child’s close relatives.
If you notice that your baby often freezes during play, watch him more closely. If you have any doubts, it is better not to wait for anything, but to visit a pediatric neurologist with your baby as soon as possible.
What are the dangers of epilepsy in childhood?
Epileptic seizures (even if they occur without convulsions), especially frequent ones (several times a day), interfere with the normal functioning of the brain and further disrupt the development of the child’s nervous system. Such children may lag behind their peers in development.
Epilepsy, especially when it begins in childhood, is characterized by special personality changes. These changes are associated not only with attacks, but also with medications taken and the attitude of others. With age, people suffering from epilepsy develop irritability, excessive thoroughness, and slowness of thinking.
Impaired motor coordination in children
Impaired motor coordination in children is a condition that occurs as a result of improper functioning of the nervous system. The consistency of interaction between human muscles is disrupted.
Impaired coordination of movements may indicate diseases of the musculoskeletal system, as well as diseases of the central nervous system. Movements may not be symmetrical or precise. If you detect any abnormalities in your child, contact the Epihelp clinic. Qualified neurologists will diagnose and prescribe treatment.
Movements are carried out thanks to the work of the cerebellum and cerebral cortex. It connects to the nervous system with 3 pairs of legs. When moving through the spinocerebellar tract, information is delivered to the cerebellum and cerebral cortex, where they are processed and regulated by accuracy, proportionality, correctness and coordination of movements, as well as regulation of muscle tone.
Diseases in which coordination of movements is impaired:
- Dyspraxia;
- Catalepsy;
- Ataxia;
- Hydrocephalus;
- Traumatic brain injury;
- Tumors;
- Diseases of the musculoskeletal system;
- Complications of infectious diseases;
- Cerebral palsy.
The most common is dyspraxia.
Dyspraxia is incoordination of movements. Commonly known as “clumsiness syndrome.” Schoolchildren suffer from this syndrome. The disease can manifest itself as:
- it is difficult for a child to learn to ride a bicycle or skate;
- confusion in the sequence of actions;
- inaccuracy in eating;
- difficult to tie shoelaces;
- speech disorders;
- illegible handwriting;
- slowness.
Causes of dyspraxia
The causes of dyspraxia are not clear. Possible causes include a lack of coordination between certain areas of the brain, slow development of its individual parts, or damage to the child’s nervous tissue. It is possible that heredity may also play a significant role.
Treatment of dyspraxia
Treatment of motor coordination disorders in children should only be carried out by a qualified specialist. Only a doctor can tell you how to treat poor motor coordination in a child, how to get rid of complications from poor motor coordination and prevent its occurrence. The main specialist in this field is a neurologist . He evaluates the child's coordination and motor functions. Treatment can improve behavior, reduce anxiety and other emotional problems for both the patient and all members of his family. Physical therapy is an important aspect of treatment. Its main goal is the gradual development of the necessary motor skills in children. Often children with this disease are sent to swim. They give recommendations on how to perform certain exercises.