Neurologist (algologist)
Vasilenko
Marina Gennadievna
25 years of experience
Head of the Pain Treatment Center, neurologist-algologist, member of the Society of Neurologists and Neurosurgeons, Russian Society for the Study of Pain, Association of Interdisciplinary Medicine, International Association for the Study of Pain (IASP)
Make an appointment
Migraine has been known to mankind for many centuries. This disease is characterized by severe paroxysmal headaches. Experts define migraine as a type of neurological pathology, which is characterized by pain localized in one half of the head. The nature of the pain and the absence of organic causes causing it significantly complicate the diagnosis of the disease. Migraine, the symptoms and treatment of which depend on many factors, is classified by doctors as a chronic disease that is practically untreatable. At the same time, provided that certain preventive measures and rules are followed, attacks can be successfully stopped and their number reduced. Questions regarding how to treat migraines are found quite often on the Internet. The best way to solve this problem is to timely contact a qualified doctor who will conduct a comprehensive examination and suggest a course of treatment.
Symptoms and signs of migraine
In most cases, migraine manifests itself, the symptoms of which depend on the cause of the pathology, severe throbbing pain in the head. In addition to severe pain with throbbing, hemicrania is characterized by:
- nausea or vomiting, loss of appetite and often slight weight loss;
- dizziness;
- irritability up to attacks of aggression;
- drowsiness;
- increased sensitivity to smells, tastes and light.
Symptoms depend on the stage of development of the pathology. After the migraine attack passes, patients usually feel well. Experts identify the following stages of disease development:
- precursors of migraine are characterized by manifestations of depression, fatigue, and irritability several hours before the attack. Some patients, on the contrary, feel an increase in activity and appetite;
- aura, which is a reflection of certain processes occurring in the brain that are associated with the mechanism of migraine development. The duration of the aura is on average up to 30 minutes, but in some cases the stage can be longer. This stage is characterized by visual effects such as blind spots, flashes of light, sensory effects such as numbness or tingling sensations, problems finding words or difficulty speaking. Symptoms may appear individually or in combination;
- The headache can last from 2-3 hours to several days. Very strong pain of a bursting or pulsating nature can cover the entire head or be localized in the temporal region. At this stage, nausea or vomiting attacks and a desire to hide in a dark room alone are common;
- resolution follows the headache phase and is accompanied by fatigue, depression, or irritability. Concentration is difficult. Symptoms persist for up to a day.
Clinical picture
Pain can occur due to sudden changes in weather, taking medications, eating certain foods and alcoholic beverages, or emotional stress. An attack of headache can occur in women during the premenstrual and menstrual periods.
The intensity of the sensations can vary from moderate to strong, the pain is concentrated on one side, less often on both. Sometimes the pain syndrome spreads to the neck, eyes, and lower jaw. Migraines can be aggravated by even minor physical exertion, which often leaves patients unable to work.
In addition, the list of migraine symptoms includes:
- High sensitivity to light, photophobia;
- Photophobia;
- Dizziness;
- Nausea and vomiting;
- Deterioration of spatial orientation.
Migraines with aura may include blurred vision, speech disturbances, and hallucinations preceding or accompanying attacks. Any migraine may be accompanied by emotional changes, such as aggressiveness and short temper, or drowsiness and apathy.
Signs and aura
The signs of migraine are determined by the form of the pathology. There is no particular difference between the symptoms in men and women, but women have attacks more often. Experts distinguish migraine, the causes of which are different, with and without aura. Aura with hemicrania is a complex of neuropsychological symptoms caused by spasms of cerebral vessels at the initial stage of development of the next attack.
There are the following types of aura, classified according to the symptoms that appear:
- visual with characteristic glare, distortions, flashes in the eyes, loss of visual fields;
- auditory with characteristic auditory hallucinations, tinnitus;
- motor, manifested by difficulties when moving;
- sensory, characterized by changes in smell and taste;
- vestibular with dizziness and even falls;
- aphasic with speech impairment.
Migraine specialists consider two main forms: regular and pathological with neurological symptoms.
Complications
The pathology can be complicated by the following conditions:
- Chronic migraine. A common complication. The number of attacks per month is more than 15. The headache occurs immediately after waking up and does not disappear during sleep. The patient suffers from insomnia and fatigue, depression and anxiety increase.
- Migrainous status. It is a serious complication and often develops in patients with hypertension. It is characterized by a series of painful attacks that last several days or an attack that lasts for 3 days. Accompanied by severe neurological symptoms, intense and bursting pain in the head, repeated vomiting and dehydration. It is fraught with the development of other serious complications.
- Migraine stroke. It is a rare but serious complication. Accompanied by constant, bursting headaches, blurred vision, and a feeling of numbness/tingling in the head. Confirmed by MRI, CT.
- Persistent aura. It proceeds like a classic migraine, but with a collection of aura signs for more than 7 days. Occurs in 1-2% of cases.
- Convulsive seizure. A quarter of people with epilepsy suffer from migraines. A migraine attack increases the likelihood of developing an epileptic seizure by 4 times.
Classification of hemicrania depending on symptoms
- Migraine headache without aura is defined by episodic headaches without neurological deficits.
- Cervical migraine with severe headaches due to impaired blood flow through the vertebral artery.
- Paroxysmal chronic, which is characterized by short-term pain repeated several times a day.
- The ocular one, which lasts no more than half an hour, appears due to circulatory disorders in the occipital part of the cerebral cortex.
- Ophthalmoplegic with characteristic gas motor disorders due to compression of the gas motor nerve and spasms of the artery supplying the nerve.
- Retinal with characteristic attacks of transient blindness due to spasms of retinal vessels.
- Afactual with speech disorders during severe pain.
- Basilar (rare), characterized by tinnitus, visual disturbances, incoordination, dizziness, loss of consciousness and severe prolonged pain. Most often, this variety occurs during puberty in girls.
- Abdominal, accompanied by nausea, diarrhea, vomiting and severe abdominal pain, occurs only in children.
- Hemplegic with short attacks, weakness in the body and limbs.
- “Beheaded” is distinguished by visual disturbances and is difficult to diagnose.
Only a qualified doctor after an examination can answer the patient’s question as to why the migraine appeared.
Prognosis for migraine
For many patients, migraines go into remission over the years and may even disappear completely. This is especially true for older women whose estrogen levels decrease after menopause. However, in a number of situations complications occur.
One of these complications is the risk of heart disease and stroke before age 50. Migraine with aura is more dangerous than migraine without aura, especially for women's health.
One cannot ignore such an item as a decrease in the quality of life due to constant emotional stress. Permanent stress negatively affects personal life and work productivity. People who have migraines are uncommunicative and often prone to attacks of panic, anxiety and depression.
Causes
The reasons why hemicrania appears are still not fully understood. During the research, scientists determined the fact that predisposition to this disease is inherited. The disease, namely the characteristics of the nervous system, is transmitted by women who suffer from hemicrania much more often than men.
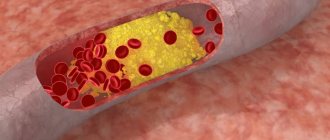
The main cause of attacks is said to be activation of the trigeminal nucleus, which alternately leads to spasm and subsequent dilation of the arteries of the brain. It has also been determined that a failure of seratonin metabolism in the central nervous system is involved in the formation of pain.
Predisposition appears when exposed to triggers or certain factors, which doctors have divided into 4 groups:
- psychological triggers, including stress, emotional and mental stress;
- external triggers, the list of which includes changes in atmospheric pressure, loud sounds, bright lighting, odors, stuffy atmosphere, etc.;
- physiological triggers, which include fatigue, insomnia, hormonal imbalances;
- food triggers. Doctors call alcohol and tyramine contained in many foods (citrus fruits, smoked meats, cocoa, cheese, nuts, chocolate, etc.) the main stimulants of hemicrania attacks.
An attack can also be caused by insufficient consumption of clean water and food, diet or caffeine withdrawal, traveling with a change in time zones, weather changes, menstrual cycles in women, relaxation after severe stress. Migraines can occur in men and women due to hormonal imbalances due to external factors, as well as due to prolonged abstinence during sexual activity.
Pathogenesis
Scientific American 299, 56 - 63 (2008) The pathophysiology of migraine has always remained mysterious, so by the end of the 20th century, three directions in its pathogenesis had emerged. All of them have received experimental and clinical confirmation. The first direction is based on the assumption: attacks are associated with narrowing or expansion of intra- and extracranial arteries. This is one of the initial theories. She suggests that migraines are caused by sudden constriction of intracranial vessels, causing cerebral ischemia and resulting aura. Following this, expansion of the extracranial blood vessels occurs, which causes headaches (Wolf, 1930). the shunt theory was proposed (G. Hake, 1960s). The headache was explained by the fact that during an attack, blood tends to pass from the artery directly into the vein through the arteriovenous shunt, bypassing the intracranial capillaries. This causes cerebral ischemia, which is the main cause of headaches. The platelet theory suggests that migraine is caused by a primary platelet disorder. When platelets stick together, a significant amount of the neurotransmitter 5-hydroxytryptamine (5-HT) is released. This theory is proven by the fact that platelets of migraine patients have a more pronounced ability to stick together than those of healthy people, and are more sensitive to factors that provoke the release of 5-HT. The second direction explains pain by a discharge arising in the trigger zone of the midbrain (possibly in the serotonergic dorsal raphe nuclei of the brainstem). Recent positron emission studies have shown that the dorsal region near the midbrain aqueduct is activated during migraine. This activity is not reduced even by sumatriptan, even if it reduces migraine pain. These areas of the brain contain serotonin-, norepinephrine-, endorphin- and GABAergic systems. It is assumed that the triggering factor for migraine is the disturbance of this particular complex of neurophysiological interactions in this area. A sharp release of serotonin leads to vasoconstriction of blood vessels (prodromal period), however, 5-HT is quickly processed and removed from the blood, which leads to vasodilation and the development of a headache attack. Therefore, a number of researchers (Vein A.M. et al.; Gtsbel H.) believe that migraine is a primary neurogenic cerebral dysfunction with the presence of genetically determined brain stem failure, severe cortical hyperactivity with periodically occurring dysfunction of the hypothalamus. Finally, the third direction is associated with the excitation of neurons of the trigeminal nucleus in the brain stem (the so-called trigeminovascular system). The axons of these neurons terminate in the arterial walls and release vasoactive neuropeptides. (M. Moskowitz et al., 1989). According to this theory, the source of headaches are the cranial vessels and vessels of the dura mater, which have trigeminal innervation and are under the control of the mid-stem structures of the brain. During a spontaneous migraine attack, the brain stem structures located near the aqueduct of Sylvius, in the area of the locus coeruleus and the reticular formation, are activated, which are a kind of generator of a migraine attack. This leads to antidromic activation of the trigeminal-vascular system with the release of neuropeptides into the vascular wall (substance P, a neuropeptide associated with the gene that controls calcitonin), causing their dilatation, increased permeability and, as a consequence, the development of neurogenic inflammation in it. Aseptic neurogenic inflammation activates the nociceptive terminals of the afferent fibers of the trigeminal nerve located in the vascular wall, leading to the formation of a feeling of pain at the level of the central nervous system. As already mentioned, special attention is currently paid to serotonin as a key link in the pathogenesis of migraine. It is assumed that it is the triggering factor for the development of migraine, and the attack itself can occur through any of these mechanisms or a combination of them. The serotonin theory is also confirmed by the fact that during a migraine attack:
- The content of 5-HT in platelets drops sharply (by 30-40%)
- There is an increased content of serotonin metabolic products in the urine
- Migraine attacks can be provoked by taking reserpine, which promotes the release of 5-HT
- Known anti-migraine drugs (ergotamine) interact with 5-HT receptors
- Intravenous serotonin may relieve migraine attacks.
Hemicrania in women
Migraine is diagnosed, the symptoms of which in women depend on the cause much more often than in men. Among the main causes of attacks in women:
- changes in vascular tone under the influence of hormonal levels changing throughout the menstrual cycle. For some women, migraine pain occurs during bleeding, for others during ovulation. Migraine medication is prescribed taking into account the patient’s hormonal background and her age;
- pregnancy, during which the load on the pregnant woman’s circulatory system increases significantly. Treatment of migraine in pregnant women requires caution when choosing medications;
- menopause, with the onset of which the ratio of hormones in a woman’s body changes significantly.
Since migraine, the symptoms and treatment of which in women depend on the individual characteristics of the body, can appear unexpectedly, doctors recommend taking preventive measures. Prevention using traditional medicine, massage and other types of therapeutic effects can significantly reduce the risk of an attack.
Treatment at the Energy of Health clinic
Neurologists at the Health Energy clinic are ready to help with migraines of any severity. We offer each patient:
- individual selection of drugs for the relief and prevention of attacks;
- training in relaxation and self-help techniques;
- sessions of restorative massage and physical therapy in the absence of contraindications.
Treatment is selected according to the individual characteristics of the body. Before prescribing a specific regimen, a complete examination of the patient is carried out to exclude other causes of headache.
Hemicrania in children
Migraines in children appear in most cases due to overwork due to heavy workload at school. Another cause is hormonal changes due to puberty. If migraine occurs more often in women than in men, then in childhood, on the contrary, boys suffer from migraine attacks more often. It is very difficult to diagnose migraine in young children who cannot formulate their complaints clearly. Migraine medications for children and adolescents are prescribed based on examination data.
Risk factors
Risk factors for hemicrania are:
- genetic predisposition;
- age – most often the disease occurs in patients 30-39 years old;
- frequent stressful situations;
- some food products, including those of artificial origin or low quality;
- fasting or irregular, poor nutrition (diet);
- changing sleep patterns;
- weather changes or moving to a different climate zone;
- intense physical activity;
- taking medications.
When to see a doctor
The Pain Treatment Center provides diagnosis and treatment of migraines. You should make an appointment with a neurologist for suspected migraine if you have the following symptoms:
- vision is blurred;
- flies float in front of your eyes;
- severe paroxysmal, pressing or throbbing headache;
- feeling sick or vomiting;
- dizzy;
- state of drowsiness and weakness;
- increased irritability.
In order to eliminate unpleasant consequences, it is enough to make an appointment with a neurologist at Meditsina JSC (academician Roitberg’s clinic) in the center of Moscow.
JSC "Medicine" (academician Roitberg's clinic) has modern diagnostic and medical equipment and a comfortable hospital. The Pain Treatment Center uses effective programs for the treatment, therapy and prevention of neurological diseases. The clinic's doctors widely use modern methods of physiotherapy. Contacting a clinic provides an opportunity to reduce the likelihood of developing migraines and avoid the consequences of the disease becoming severe.
Advantages of the clinic
Medical facilities are equipped in accordance with modern standards of diagnosis and treatment of diseases. We try to make every patient feel comfortable within the walls of the clinic and offer:
- consultations with doctors of various specialties;
- informative methods of instrumental, functional and laboratory diagnostics;
- individual selection of treatment regimen;
- complex effect on the body using not only drugs, but also additional methods: physiotherapy, massage, exercise therapy, manual therapy, etc.
Reception is by appointment, without queues or long waits. The location of the centers allows both motorists and those traveling by public transport to reach us comfortably.
If migraine attacks are making your life miserable, do not endure the pain. Contact the neurologists at Health Energy. Together we will find a way to relieve you of this disease.
Diagnostics
Diagnosis of migraine is carried out on the basis of collecting complaints and anamnesis of patients, examining the patient and talking with him. If the initial consultation does not allow you to accurately diagnose the disease or identify the causes of the pathology, the neurologist can give a referral for an extensive examination using modern diagnostic equipment:
- MRI of the neck and brain;
- CT scan of the brain;
- brain scinography;
- electroencephalography;
- duplex scanning of arteries;
- Doppler ultrasound.
Consultation with an ophthalmologist allows you to determine the condition of the fundus and cerebral vessels. The presence of migraine symptoms may indicate serious pathologies, so a thorough examination is mandatory. JSC "Medicine" (academician Roitberg's clinic) is equipped with the latest diagnostic equipment, allowing examination of any complexity. The clinic is located in the center of Moscow at 2nd Tverskoy-Yamskaya lane, 10, a five-minute walk from the Mayakovskaya metro station.
Migraine is often a symptom of more severe diseases, so high-quality diagnosis using modern diagnostic equipment is an effective way to timely detect pathologies. Timely detection of diseases and contacting qualified doctors is a prerequisite for recovery and full restoration of vital activity.
JSC "Medicine" (clinic of academician Roitberg) is a multidisciplinary center, which provides patients with the opportunity to easily consult with specialists in various fields of medicine.
Treatment
If a patient is diagnosed with migraine, the doctor selects treatment taking into account many factors, including examination results:
- Drug therapy is symptomatic. The main goal of drug therapy is to reduce the intensity of attacks. The doctor selects tablets for migraine taking into account the form of the disease, the patient’s health condition and the nature of the attacks;
- for minor pain, non-steroidal anti-inflammatory drugs can be prescribed;
- for infrequent attacks and mild forms of the disease, anilades in combination with the effect of vasoconstriction are effective against migraines;
- triptans for migraines with a vasoconstrictor effect.
It is important to remember that migraine medications are selected for the patient and prescribed only by a doctor, since uncontrolled use of medications can cause side effects and complications that will lead to serious deterioration in health.
Non-drug methods include organizing a work and rest schedule, eliminating foods that stimulate attacks, giving up alcohol and smoking, selecting a diet, etc.
Among non-drug methods, mention should be made:
- neck massage;
- acupuncture;
- acupressure.
Specialists at the Pain Treatment Center of JSC “Medicine” (academician Roitberg’s clinic) approach the treatment of migraines in a comprehensive manner. An integrated approach allows us to minimize the impact of the disease on the patient’s body and the patient’s health as a whole. The combination of various methods of rehabilitation and therapy allows you to achieve excellent results in a short time. Contacting the neurologists of JSC "Medicine" (clinic of Academician Roitberg) provides the opportunity to significantly improve the quality of life.
Modern approaches to the treatment of migraine
Migraine is a common disorder, occurring in 6% of men and 18% of women (Rasmussen BK et al., 1991). Despite the fact that migraine therapy is well developed (according to the American Headache Association, the effectiveness of correct treatment can reach 95%), more than 70% of patients are not satisfied with the result of treatment (Lipton RB, Stewart WF, Simon D., 1998). This is partly the fault of the patients themselves, who do not see a doctor, self-medicate, and ignore the recommendations they receive. However, in many cases, the low effectiveness of therapy is the result of inadequate medical care. Some doctors continue to manage patients with migraine based on outdated information, without considering the possibilities of modern migraine treatments. However, the difficulty of treating headaches is not only due to the “correct” choice of medication. Migraine is a complex neurobiological disorder with a multifactorial pathogenesis, and the problem of its treatment cannot be solved with the help of any one drug, even a new and effective one. To achieve success, it is necessary to take into account a number of aspects, both purely medical and psychological.
In the treatment of migraine, three tasks can be distinguished - prevention of attacks, their treatment and prevention.
- Preventing migraine attacks . By teaching the patient to identify warning signs, identify migraine triggers, and avoid situations that provoke migraine, it is possible to prevent or significantly reduce the number of attacks without the use of drugs.
- Treatment of seizures . Many patients suffering from migraine are maladjusted by the fear associated with anticipating an attack. In this regard, it is very important to work together with the patient on treatment tactics for various scenarios of migraine development.
- Preventive treatment of migraine . If migraine attacks are frequent (more than 2 times a week) and/or if behavioral and pharmacological measures are ineffective, it is necessary to consider preventive treatment. Some specific forms of migraine are also indicated for preventive treatment: hemiplegic migraine or migraine with aura with persistent neurological deficit.
Preventing migraine attacks
The success of treatment largely depends on the doctor’s ability to teach the patient to recognize triggers and avoid situations that provoke migraines. According to our study, when first told, the connection between the onset of a headache and some factors is noted by about 30% of patients visiting a doctor (Danilov A. B., 2007). With careful questioning using a special questionnaire that lists all possible headache triggers, the frequency of identifying such factors increases to 85%.
The difficulty of detecting provoking factors may be explained by the fact that some of them never cause a migraine attack in some patients, while in others they do, but not always. For example, many patients sensitive to alcohol notice that if they are in a good mood, relaxed, and following a low-carb diet, then a moderate amount of white wine does not lead to negative consequences. If these patients are tense and eat a lot of sweets, then the same wine can cause them a severe migraine attack. When the presence of migraine triggers is not obvious, it is useful to use a headache diary, which helps to recognize the factors that provoke the development of migraines.
In a study conducted at our department, it was shown that in some patients a migraine attack did not occur at the height of emotional stress, but at the end of a stressful situation: after an important speech, after signing a complex contract, at the beginning of a vacation (“weekend migraine”), after receiving a promotion, etc. Chronic stress (family conflicts, work overload) contributed to an increase not only in the frequency of attacks, but also in the intensity of headaches. At the same time, the strength of the provoking factor depended on the significance that the patient attached to the events in accordance with his attitudes and coping strategies - the situation became/did not become “stressful” depending on the patient’s individual reaction to it. It was noted that men were more likely to attach importance to problems related to professional activities, and women were more concerned about their social relationships at work and at home (Danilov, 2007).
In susceptible individuals, foods may cause headaches. Most often, such triggers are meat (pork, game), as well as animal organs (liver, kidneys, goiter, brains), sausages and frankfurters, herring, caviar and smoked fish, vinegar, salted and pickled foods, some types of cheese (cheddar, "brie"), products containing yeast (especially fresh bread), chocolate, sugar and products containing it, citrus fruits (if consumed in large quantities), cream, yoghurt, sour cream, legumes, flavor enhancers such as monosodium glutamate, caffeine ( black tea, coffee), alcohol, especially red wine. It should also be taken into account that the development of a migraine attack can also be triggered by skipping meals.
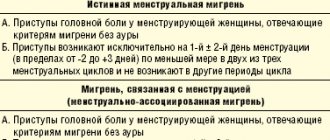
Other migraine triggers are strong odors (even pleasant ones, such as perfumes, cigar smoke), vestibular stress, bright light, noise, and smoking. In women, in addition, the development of headaches can be triggered by certain days of the menstrual cycle or the start of taking oral contraceptives.
Physical activity can also be a migraine trigger. According to our study, 7% of women and 21% of men associate headaches with physical activity. Migraine attacks can be provoked by exhausting physical exercise (for women - fitness, dancing, for men - running, football, fitness). Playing sports without physical exhaustion does not lead to headaches (Danilov, 2007).
In 10% of cases, migraine attacks occur during sexual intercourse (Evans RW, 2001). The cause of headaches that develop during sexual activity may not be migraine, but secondary dangerous disorders - aortic aneurysm and others, so in this case it is advisable to undergo a thorough examination. Fortunately, secondary headaches are rare. However, sexual activity may also help reduce or even stop a migraine attack. In a study by Couch JR and Bearss C. (1990), which involved 82 women suffering from migraine, having sex at the onset of a migraine reduced the severity of headaches and other symptoms in every third patient, and in 12% of women, sex completely stopped the attack. The effect was more pronounced in those women who experienced orgasm. The authors explain the observed phenomenon by the influence of antinociceptive opiate systems, which are activated during sex and help reduce or stop headaches.
A number of migraine triggers, such as weather changes and certain days of the menstrual cycle, cannot be avoided. In these cases, it is important to simply be aware of the possible threat of migraine development and be prepared for the onset of an attack. Most other triggers can be controlled and should be disclosed to the patient. Thus, for many patients it may be an unexpected discovery that a migraine attack can be provoked not only by insufficient sleep and overwork, but also by excess sleep, a situation of recovery from a period of stress, overload.
Currently, many devices are offered to reduce or avoid the influence of migraine triggers, for example, special sunglasses, fluorescent lamps instead of “yellow” ones, earplugs, eye masks, and special pillows. It is also important to be able to relax. There are special techniques that help you relax and prevent the development of headaches in cases where you could not avoid a stressful situation.
Treatment of attacks
Behavioral interventions
Preparing for a possible attack. An important factor contributing to the success of treatment is achieving a sense of control over the headache: the pain can be exacerbated by the anxiety that grips the patient in anticipation of a new attack, and the feeling of helplessness that arises if the patient does not know how to cope with the attack. When the trigger or precipitating situation cannot be prevented, or when the patient fails to follow the doctor's instructions, it is important to teach the patient what to do if the development of a headache is unavoidable.
First of all, it is necessary to help the patient learn to recognize the onset of a migraine. Many patients (usually with many years of migraine experience) accurately distinguish migraine from other types of headaches. For others, the doctor’s explanations about the characteristics of migraine attacks (presence of precursors, aura, impaired concentration, nausea, etc.) will be very valuable. The education of the patient in this case is of direct importance in the choice of medications to relieve the attack. If a migraine of moderate or severe intensity is expected, then the best treatment in this situation will most likely be a drug from the triptan group. If the development of a mild headache is expected or the patient feels that in this case he is developing an episode of tension-type headache, then in this situation it is advisable to use a conventional analgesic or a drug from the group of non-steroidal anti-inflammatory drugs (NSAIDs).
It is important to select a drug in advance to relieve an attack, taking into account previous experience with the use of drugs (efficacy, presence of adverse reactions), the patient’s preferences and expectations, and the severity of the expected attack. The tactic of “waiting” is now recognized as incorrect. Migraine attacks can last up to 72 hours, and the longer it takes for migraine symptoms to appear, the worse the response to treatment. If you take the medicine as early as possible after the first signs of migraine appear, you can often completely prevent or significantly reduce the intensity and duration of the headache and quickly return to social or work activity.
Providing conditions for a comfortable experience of an attack . A number of behavioral interventions can enhance the effectiveness of medications. If a migraine attack begins, it is advisable to stop exposure to irritating stimuli (bright lights, loud speech, working at a computer monitor, activities requiring physical or mental stress). Understanding others is very important here. It makes sense for the patient to warn his family or colleagues and superiors in advance that he has migraine attacks, which can prevent him from working for 24 hours or more. They should be told that if the patient is given the opportunity to stop working, take medication and sit in silence, this will greatly increase the likelihood that after 2 hours he will be able to return to normal activities, successfully coping with the attack.
Drug therapy
To date, many methods have been developed for the treatment of migraines, ranging from tea from wild rosemary branches to triptan drugs. What is the best treatment? The best treatment will be one that is tailored to the individual needs of a particular patient.
Until recently, a stepwise approach was adopted in the treatment of migraine, according to which it was initially proposed to use simple analgesics or drugs from the NSAID group to relieve an attack. If the effect was insufficient, we switched to combination drugs. If the tried remedies turned out to be ineffective, it was proposed to use “upper step” drugs—triptans. Thus, triptans were used only in resistant cases.
This approach has often frustrated patients who would have preferred a doctor to immediately prescribe an effective drug. With a stepwise approach, the average patient tried about 6 drugs before finding the optimal one (Lipton RB, 2000). It should be taken into account that another failure when taking a new drug seriously undermines the patient’s faith in the possibility of success of therapy, increases anxiety, contributes to the development of depression and maladjustment, which worsens the prognosis of therapy.
The stratified approach to migraine treatment has proven to be extremely convenient for clinical use. It is based on assessing the impact of migraine on the patient’s daily activities using the MIDAS (Migraine Disability Assessment Scale). Depending on the answers to five simple questions about time lost due to headaches in three main areas of life (study and work, housework and family life, sports or social activity), the severity of migraine is determined. The MIDAS scale divides patients into 4 groups, where group I corresponds to minimal disruption of daily activities and mild headache intensity, and group IV is characterized by a severe degree of maladjustment and severe headache (Lipton RB, Stewart WF, 1998). Each group offers its own medications.
Treatment of attacks of mild intensity, which practically do not worsen the quality of life of patients. Patients in this group rarely go to the doctor, since they are helped by physical methods of dealing with pain (heat, cold), numerous “folk” methods (cabbage leaves, lemon peel, peeled, etc.). Of the pharmacological agents for rare attacks of unexpressed headache, simple analgesics (Analgin), paracetamol or drugs from the NSAID group are usually effective: ibuprofen (Ibuprofen, MIG 400, Nurofen), naproxen (Naproxen), indomethacin (Indomethacin), diclofenac (Voltaren ) etc. The choice of drug should be made depending on the patient’s preferences, taking into account past experience with drugs and the risk of gastrointestinal complications
Treatment of attacks of moderate intensity. For pain of moderate intensity, NSAIDs are indicated. More effective are combined analgesics containing codeine or caffeine (Caffetin, Solpadeine, Tetralgin, Pentalgin). These drugs can be purchased without a prescription. Many patients, unfortunately, get too carried away with them, believing that it is necessary to be careful only when using medications prescribed by a doctor. It should be remembered that over-the-counter medications, when used in excess, can lose their effectiveness and sometimes even cause an overuse headache, that is, a headache caused by excessive use of the drug.
In cases of severe maladjustment in patients with moderate headache intensity, it may be advisable to start therapy with a triptan drug. The use of triptans can reduce the number of drugs that patients take for the symptomatic treatment of migraine and prevent chronic headaches.
Treatment of high intensity attacks. If the headache intensity is high, it is recommended to immediately prescribe a drug from the triptan group. In some cases, it is advisable to use opioid analgesics. Clinical studies have demonstrated the high effectiveness of the combination drug Zaldiar, which includes the weak opioid analgesic tramadol and the analgesic and antiperetic paracetamol, for relieving migraine attacks. Thanks to this combination, it is possible to achieve high efficiency with a low number of side effects (Ekusheva E. V., Filatova E. G., 2007). Zaldiar does not belong to the group of narcotic analgesics, and any doctor can prescribe it on prescription form No. 147.
Severe headaches are often accompanied by severe nausea and vomiting. In this case, it is advisable to use antiemetics: metoclopramide (Metoclopramide, Cerucal, Ceruglan), domperidone (Domperidone, Motilak, Motilium), chlorpromazine (Chlorpromazine, Aminazine). Some experts recommend using an antiemetic 20 minutes before taking an NSAID or triptan drug. If the attack is accompanied by nausea, it is advisable to use a triptan nasal spray (Imigran) (.).
For very severe persistent migraine attacks, the use of corticosteroids (dexamethasone 8–12 mg intravenously or intramuscularly) is necessary.
Some studies have demonstrated a good effect (“on the needle” effect) of Cormagnesin for relieving migraines of moderate or severe intensity (Danilov A. B. et al., 2004). There are other medical methods for relieving migraines, for example, treatment with leeches, injections of novocaine into trigger points, etc. These methods are very effective in the hands of those specialists who have developed them or have extensive experience in their use. Unconventional approaches to the treatment of headaches can be welcomed if they are effective, but they cannot be recommended for mass use without evidence-based research.
Features of triptan drugs . The gold standard for migraine therapy is sumatriptan. The effectiveness and safety of sumatriptan was studied in 300,000 attacks (more than 60,000 patients) in clinical trials and in 200 million attacks in clinical practice over 15 years of its use. Patient satisfaction with this drug is 63% and significantly exceeds satisfaction with drugs of other classes that are used to relieve migraines (Pascual J., 2007). Sumatriptan is more effective in patients with slow onset headaches. In our country, sumatriptan is produced in the form of tablets under the trade names Amigrenin, Imigran, Sumamigren, in the form of a spray - “Imigran” and in the form of suppositories “Trimigren”. Studies of generic sumatriptan (Amigrenin, Sumamigren) conducted in our country confirmed its high effectiveness (Vein A.M., Artemenko A.R., 2002; Tabeeva G.R., Azimova Yu.E., 2007).
Naratriptan (Naramig), zolmitriptan (Zomig), eletriptan (Relpax) belong to the second generation of triptans and have greater selectivity of action compared to sumatriptan, which leads to fewer side effects and greater effectiveness in some respects. The use of these drugs is advisable when taking sumatriptan is ineffective.
The following recommendations have been developed for the use of drugs from the group of triptans to relieve a migraine attack. After the patient feels that he is developing a migraine attack of severe or moderate intensity, he should take 1 tablet of the drug (minimum dose). If the pain goes away after 2 hours, the patient can return to normal activities. If after 2 hours the pain has decreased, but has not gone away completely, it is recommended to take another dose (tablet) of the drug. Next time you can immediately take a double dose of the drug (2 tablets).
If there is no effect 2 hours after administration, the drug is considered ineffective. In this case, the question of replacing it should be raised. Some headache specialists suggest trying the drug 3 times before giving it up. Other doctors believe that a new drug should be used for the next attack. We adhere to the second point of view, i.e. if the drug was taken in a timely manner during a correctly recognized migraine attack and after 2 hours the intensity of the headache has not changed at all, then at the next attack you should take another drug (a triptan from a different group or from a different manufacturer). Note that there is marked variability in the effectiveness of the drug, including within the triptan series, depending on individual sensitivity. It is important to patiently select from the available arsenal the remedy that will be effective for a given patient.
Once an effective drug has been found, you should not experiment with others. Recommend that the patient always carry the medicine with him. There should be no fear of addiction if the drug is used no more than 2 times a week. Taking triptans more frequently can lead to side effects, including triptan overuse headache (headache caused by drug abuse). Also, do not exceed the maximum daily dose. There are contraindications to the use of triptans, such as the presence of hypertension and other cardiovascular disorders (for a complete list of contraindications, see the instructions for use). The choice of drug should be made jointly by the doctor and the patient, taking into account pharmacochemical characteristics, the presence of contraindications and individual sensitivity.
Preventive treatment of migraine
Prescribing preventive treatment is a responsible task that requires careful preliminary discussion with the patient. Preventative treatment is associated with side effects due to long-term use of medications and requires patience from the doctor and the patient. However, the lack of preventive treatment can lead to abuse of analgesics and the development of abusive headaches. Frequent migraine attacks are the basis for the occurrence of chronic migraine, as well as risk factors for vascular brain damage.
To prevent migraine, various pharmacological agents are used, including those for which the recommendations do not yet include this indication. Monotherapy is preferable; in complex cases, combination treatment is allowed, taking into account concomitant diseases. The drugs of choice are beta-blockers - propranolol (Anaprilin, Obzidan). Antidepressants and anticonvulsants, which occupy a leading position in the effectiveness of preventive treatment, still do not have this indication in the instructions for use. Of the anticonvulsants, the most effective are valproate and the new anticonvulsant topiramate. Clinical studies have shown that topiramate is effective in preventing migraine attacks, significantly reducing their frequency. Its effect develops quite quickly - during the first month of therapy there is a stable, long-term decrease in the number of attacks without the development of resistance. Compared to other anticonvulsants, topiramate has a favorable tolerability profile (Brandes JL, 2004).
Antidepressants have long been used to treat migraines. The basis for their use is the information accumulated in the treatment of chronic pain. Antidepressants reduce the accompanying symptoms of depression, which is either present in the patient initially or develops in connection with frequent migraine attacks. Antidepressants potentiate the effect of analgesics and triptans, and some of them have independent antinociceptive or analgesic activity. The most favorable efficacy/safety ratio is observed in the new generation of antidepressants - venlafaxine (Velafax, Velaxin), duloxetine (Cymbalta), milnacipran (Ixel).
Prospects for migraine treatment
Currently, a phase 2 study is underway in Europe of the CGRP receptor antagonist olcegepant, which, when administered intravenously, prevents intracranial vascular dilatation that occurs during a migraine attack. Research is also being conducted on the first tablet form of the CGRP receptor antagonist, MK-0974, to relieve migraine attacks (Doods H. et al., 2007).
A group of American scientists from the Ohio University Medical Center conducted a study on the use of transcranial magnetic stimulation to interrupt migraine attacks with aura. According to current theory, the development of migraine begins with an increase in electrical activity in the occipital lobe, after which the electrical impulse spreads throughout the brain, causing the symptoms of a migraine aura. The essence of the technique is to interrupt this electrical activity using an electromagnetic pulse. More than two-thirds of patients treated with transcranial magnetic stimulation reported either no or moderate pain two hours after the procedure. Less than half of the patients reported the same effect in the placebo group (Clarke BM et al., 2006).
Clinical trials of a new drug, an aerosol for migraines, are currently underway. To supply the active substance, the patented technology for the manufacture of Stokatto inhalers is used, which has a number of features. The device has a built-in battery, which, when pressed on the piston, heats up one dose of a solid medicinal substance, turning it into an aerosol. The aerosol particle size—1–3 micrometers—is optimal for deep irrigation of the lungs, where the drug is quickly absorbed and enters the circulatory system at a speed comparable to intravenous injections. The new drug, codenamed AZ-001, is the Staccato system of prochlorperazine, a drug used to treat symptoms such as nausea and vomiting. Recently, research results were released that showed that when administered intravenously, this substance is effective for migraines. Thus, if the clinical trials are successful, Staccato Prochlorperazine will have undeniable advantages over tablets and intravenous injections, since it will combine the effectiveness of an intravenous drug with convenience and ease of use, which will allow the use of the inhaler at home (Alexza news release, 2007).
Non-pharmacological aspects of migraine treatment
Despite the fact that advances in the field of pharmacology play a huge role in the treatment of migraine, the skill of the doctor is no less important, and first of all his ability to build a dialogue with the patient. Here are the factors that doctors consider most important when achieving success in treating migraines.
- Collaboration with the patient. Particularly important is the sincere attitude of the doctor towards the patient, which is manifested through non-verbal communication (intonation, facial expressions, gestures). The patient will immediately feel if the doctor tries to hide his irritation behind encouraging remarks due to the fact that the patient is taking up his time with his questions, when the diagnosis is clear and the patient has long been given a leaflet with prescriptions.
- Involving the patient in the treatment process. The essence of the problem, treatment options should be explained to the patient and he should be involved in the choice of therapeutic agents, taking into account past experience, preferences and expectations. The time spent explaining the essence of the problem pays off with high patient adherence to treatment and, as a result, higher rates of effectiveness of the therapy.
- Patient education and training. Many patients are frustrated by the fact that various doctors and numerous tests do not find a physical cause for their headaches. In this situation, it is advisable to spend time explaining the pathogenesis of migraine. In addition, it is important to educate the patient to identify triggers and avoid migraine-provoking situations.
- Assessment of migraine severity. The severity of migraine is determined not only by clinical manifestations, but also by how much the disease interferes with the patient's life.
Critically evaluate the patient's past experiences, attitudes and expectations. Often patients turn to the doctor who have already tried all known medications and have not received the desired effect. In these cases, it is important to carefully question the patient about previous experience with the medication in order to understand what may be causing the lack of effectiveness.
Conclusion
Thus, treating migraine is a complex, complex task that requires erudition, sensitivity to the patient, good communication skills and patience from the doctor. Currently, not only modern drugs have been developed, but also new approaches to treatment that allow its selection based on objective criteria. However, a doctor faced with the treatment of migraine cannot be a simple executor of the proposed algorithms. In order for therapy to be effective and safe, it is necessary to creatively approach the choice of methods, taking into account the individual characteristics of patients. Also very important is the creation of a trusting and at the same time business relationship with the patient, his education and active involvement in the treatment process. If the doctor manages to cope with all of the above tasks, treatment will not only relieve the symptoms of the disease, but also improve the patient’s quality of life by eliminating or mitigating his social and work maladjustment, that is, achieving exactly what the patient comes to the doctor for.
For questions about literature, please contact the editor
A. B. Danilov , Doctor of Medical Sciences, MMA named after. I. M. Sechenova , Moscow
Home remedies
Home remedies for migraines can complement the effects of drug therapy. If migraine is diagnosed, treatment at home can be undertaken after consultation with a doctor. Among the most effective methods it should be noted:
- infusions of medicinal herbs (chamomile, peppermint, lavender, raspberry leaves, etc.);
- infusion of oregano as a preventative measure;
- mumiyo solution before bedtime;
- rubbing essential oils into temples for mild attacks;
- cold compresses on the head;
- rest in a darkened room with clean air in silence.
How to treat migraine with aura and how to relieve pain effectively and quickly
Since it is almost impossible to avoid an attack if there is a trigger, you need to know ways to improve the condition, because migraine is not a death sentence.
The final diagnosis is made by a neurologist. He will tell you what to do, how to treat the disease, how to increase the intervals between attacks.
Treatment for migraines is based on eliminating the pain and making it happen as little as possible or go away altogether. NSAIDs or specific medications, most often triptans, may be used. Intravenous infusion therapy is also used to treat migraines. The effectiveness of pain relief is directly proportional to the time of taking the drugs. You can stop an attack when it has just begun. Unfortunately, many people miss this moment with the thought “what if it doesn’t hurt.” However, at the peak of an attack, the tablets have almost no effect, because with migraine gastrostasis in the intestines, the absorption of any substances is very difficult.
Alternative ways to alleviate the condition are physical activity, exercise therapy, physiotherapy, and psychotherapy. Massage of the collar area is especially useful, because muscle spasm in this area can provoke an attack. Recently, migraines have been successfully treated with injections of botulinum toxin type A. The injections make remission last longer, and in some cases relieve pain for a very long time.
Treatment of migraines using traditional medicine
Many traditional medicine methods can provide relief from pain.
Ginger root
Ginger has the ability to block prostaglandins, thereby reducing the severity of pain. The same principle applies to most NSPVs. Ginger tea is prepared at home. Ginger root is crushed, then added to boiling water and simmered for 10 minutes over low heat. Next, the tea is filtered and drunk plain or with lemon and honey.
Chamomile
Has an anti-inflammatory and calming effect. You need to take two tablespoons of chamomile in a glass of water and cook the mixture for 5 minutes over low heat. Next, you need to strain the broth and drink it plain or with lemon and honey.
Lavender
Lavender oil is used for inhalation. The solution is prepared as follows: a teaspoon of oil is diluted in three glasses of boiling water. Breathe over the resulting solution for 15 minutes. Lavender oil can be mixed with peppermint oil and apply the mixture to the temples, gently massaging it a little. It is best to combine massage and inhalation.
Prevention
In severe forms of hemicrania, preventive drug therapy can be prescribed, the use of which can significantly reduce the frequency and intensity of attacks. A drug for the prevention of attacks of hemicrania is prescribed by a doctor solely based on the data of the examination and examination of the patient. Doctors at JSC "Medicine" (clinic of academician Roitberg) use certified drugs that combine high efficiency with safety for the health of patients.
An important role in prevention is played by giving up bad habits, normalizing exercise and rest, and minimizing emotional and physical stress. During pregnancy, preventive medications are not prescribed due to possible harm to the health of the fetus.
How to make an appointment with a neurologist
JSC "Medicine" (academician Roitberg's clinic) in Moscow offers European-level services for the diagnosis, treatment and prevention of migraine. To receive highly qualified medical care, you must make an appointment with a neurologist who will conduct an examination and a comprehensive medical examination.
To make an appointment with a specialist, use one of the following methods:
- quick registration form on the main page of the clinic’s website;
- by phone 24 hours a day +7 (495) 775-73-60;
- using a mobile application.
The clinic is located in the center of Moscow at 2nd Tverskoy-Yamskaya lane, 10, a five-minute walk from the Mayakovskaya metro station.
JSC "Medicine" (clinic of academician Roitberg) in Moscow also offers emergency call services around the clock by calling +7.