Benedict's syndrome (syn. alternating paralysis syndrome)
The syndrome occurs as a result of a pathological process in the medial-dorsal part of the midbrain at the level of the red nucleus and the cerebellar-rednuclear tract with the preservation of the paramidal fasciculus. The causes of the lesion are thrombosis and hemorrhages in the posterior cerebral artery basin, tumor metastasis.
Clinical signs and symptoms. On the affected side, extrapyramidal hyperkinesis in the limbs and cerebellar ataxia occur. On the side opposite to the localization of the lesion, mild spastic hemiparesis and tremor of the lower extremities develop. Against the background of hemiparesis, increased tendon reflexes are observed.
In addition, there is an increase in overall muscle tone. Eye symptoms are caused by complete or partial paralysis of the oculomotor nerve. Ptosis occurs on the side of the pathological focus. There is a deviation of the eyeball towards the lesion, there may be disturbances in associated eye movements during convergence and the direction of gaze up or down. A differential diagnosis of this syndrome is made with the following syndromes: Claude, Weber-Gubler-Gendrin, Millard-Gubler, Fauville, Nothnagel.
The development of the syndrome is associated with a pathological process located directly in the region of the cerebral peduncles, which occurs as a result of hemorrhages, ischemic cerebral circulation disorders, as well as neoplasms. In addition, the signs of this syndrome may be caused by dislocation compression of the cerebral peduncles by a tumor located at a distance.
Clinical signs and symptoms. Due to damage to the facial and lingual nerves, as well as the pyramidal tract, paralysis of the muscles of the face, tongue and limbs of the central type occurs on the side opposite the pathological focus. Eye symptoms are caused by complete (ophthalmoplegia, ptosis, mydriasis) or partial (damage to only intraocular muscles or individual extraocular muscles ) oculomotor nerve palsy.
Symptoms of paralysis occur on the side of the pathological focus. In case of damage to the extraocular muscles innervated by the oculomotor nerve, the eyeball deviates towards the temple and “looks” towards the pathological focus, “turning away” from the paralyzed limbs. If a pathological process - for example, an aneurysm of the anterior cerebral artery - involves the optic tract or the external geniculate body, homonymous hemianopsia occurs.
Unilateral damage to the ventral part of the pons involving the nucleus or bundle of fibers of the facial nerve, the root of the abducens nerve and the underlying pyramidal tracts leads to the development of this syndrome. The pathological process in this area may be associated with impaired circulation in the paramedian arteries (hemorrhages, thrombosis).
With the development of a tumor of the pons (most often glioma and much less often cancer metastasis, sarcoma, solitary tubercles), a slow gradual development of the syndrome is observed. Clinical signs and symptoms. On the affected side, signs of peripheral paralysis of the facial nerve appear, while central hemiparesis or hemiplegia is observed on the side opposite the lesion.
{module direct4}
Ocular symptoms are caused by damage to the abducens and facial nerves. On the side opposite the pathological focus, signs of damage to the abducens nerve appear - paralysis of the external rectus muscle, convergent paralytic strabismus, diplopia, which intensifies when looking towards the affected muscle. On the contrary, symptoms of damage to the facial nerve are observed on the side of the pathological focus - lagophthalmos, lacrimation.
The pathological process in this syndrome is located at the base of the legs and involves the fibers of the oculomotor nerve. The development of the syndrome is caused by damage to the branches of the posterior cerebral artery - the middle and posterior arteries of the red nucleus, which supply blood to the lower parts of the red nucleus. The most common causes of vascular damage are atherosclerosis and syphilitic endarteritis.
Alternating symptoms of midbrain damage.
The roof of the midbrain is the roof plate, the base is the cerebral peduncles, and the nuclei of the midbrain are located in the middle part.
The dorsal part (roof) of the midbrain has 2 superior and inferior colliculi. The inferior colliculus is responsible for hearing and complex reflexes in response to auditory stimuli.
Alternating midbrain syndromes. Characteristic clinical manifestations of damage to the brainstem at the level of the midbrain are oculomotor disorders, sleep disturbances, motor and mental activity.
Hertwig-Magendie sign
. It consists of different positions of the eyeballs in the vertical plane. On the side of the pathological focus, the eye is deviated downward and slightly inward, and not upward and outward on the opposite side.
Parinaud syndrome
. It is observed with bilateral damage to the tegmentum and roof of the midbrain in its oral part, at the level of the superior colliculus. Manifested by paresis or paralysis of upward gaze, weakness or delayed convergence, partial bilateral ptosis, miosis. decreased photoreactions. In this case, the movements of the eyeballs to the sides are not disturbed.
Nothnagel syndrome.
Clinically manifested by bilateral ophthalmoplegia, lack of pupillary response to light, mydriasis, ptosis, and hearing loss. Various cerebellar disorders are common; sometimes symptoms of bilateral pyramidal lesions are added. Nothnagel syndrome most often occurs with tumors, especially of the pineal gland.
Weber syndrome
occurs in case of damage to the nuclei or fibers of the oculomotor nerve. In this case, symptoms of damage to the third pair of cranial nerves on the side of the lesion, hemiplegia, develop. Weber syndrome is accompanied by simultaneous damage to the corticonuclear tracts of the facial and hypoglossal nerves, which is manifested by central paralysis of the muscles of the tongue and face.
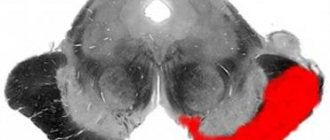
Benedict's syndrome.
In this case, the lesion is located at the same level as in Weber syndrome, but more dorsally. In this case, the red nucleus and substantia nigra are involved in the pathological process. Clinically, the syndrome is manifested by paralysis of the peripheral oculomotor muscles on the affected side and intentional hemitremor on the opposite side. In the case of a larger lesion, simultaneous damage to the fibers of the medial lemniscus occurs. In this case, clinical manifestations are accompanied by impaired sensitivity on the opposite side (superficial and deep).
Superior red nucleus syndrome (Foix syndrome)
occurs if the pathological focus is located in the tegmentum of the midbrain in the area of the upper part of the red nucleus, and manifests itself on the opposite side as cerebellar hemitremor (intentional tremors), which can be combined with hemiataxia and choreoathetosis. The oculomotor nerves are not involved in the process. Described by the French neuropathologist Ch. Foix (1882-1927).
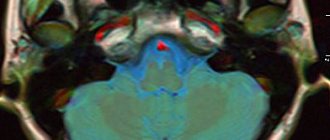
Inferior red nucleus syndrome (Claude syndrome)
- alternating syndrome caused by damage to the lower part of the red nucleus, through which the root of the third cranial nerve passes. On the side of the pathological process, there are signs of damage to the oculomotor nerve (ptosis of the upper eyelid, dilated pupil, divergent strabismus), and on the opposite side there are cerebellar disorders (intentional tremors, hemiataxia, muscle hypotonia). Described in 1912 by the French neuropathologist N. Claude (1869-1946). With this syndrome, coordination of movements is impaired, hemihyperkinesis develops, as well as muscle hypotonia, which is associated with damage to the superior cerebellar peduncle. At the same time, the nucleus of the oculomotor nerve is affected with the development of paralysis of the muscles innervated by it, of a peripheral nature.
Myasthenia gravis
- an autoimmune disease accompanied by weakness and pathological muscle fatigue due to blockade of postsynaptic acetylcholine receptors of neuromuscular junctions by autoantibodies.
Etiology
Myasthenia gravis is not a hereditary disease; its etiology has not been fully established. In 60-70% of patients, changes in the thymus gland are found in the form of a tumor or hyperplasia.
Pathogenesis.
The basis of the disease is a violation of neuromuscular transmission. The pathologically altered thymus gland produces specific antibodies against cholinergic receptors, which causes a competitive block of synaptic conduction.
Impaired acetylcholine synthesis as a result of defective enzyme activity and insufficient sensitivity of cholinergic end plate receptors play a role. In the serum of patients with myasthenia gravis, antibodies to skeletal muscles and to epithelial cells of the thymus gland can be detected.
Clinic:
muscle weakness and pathological muscle fatigue, which may be diffuse or limited. After rest, muscle strength is partially or completely restored.
The disease is more common in adults. The disease begins with the eye muscles. Ptosis of the upper eyelids (unilateral or bilateral), strabismus, and diplopia develop. In the future, generalization of the pathological process may develop: weakness and fatigue of the facial and masticatory muscles, muscles of the tongue, pharynx, larynx, neck, trunk and limbs appear. Respiratory and cardiovascular problems are possible. Deep reflexes in myasthenia gravis are normal or reduced, there are no sensory disorders.
A severe complication of myasthenia gravis is the development of myasthenic crisis, in which there is a sharp deterioration in the condition in the form of generalized muscle weakness, the appearance of bulbar symptoms and breathing disorders. In the absence of urgent resuscitation measures, myasthenic crisis can lead to death.
Treatment
thymectomy, radiation therapy to the thymus region, plasma exchange transfusion, use of immunosuppressive drugs (prednisolone, azathioprine). Symptomatic therapy includes the use of anticholinesterase drugs (proserin, oxazil, kalimine). Emergency therapy for myasthenic crisis consists of intravenous administration of 0.5-1.0 ml of a 0.05% solution of proserin, and then intramuscular injection of 2-3 ml of the same solution.
TASK
Preceded by DZ - syncope associated with overexcitation of the vagus (differencing with a tumor of the left temporal lobe), secondary generalized convulsions.
Topic DZ – damage to the deep parts of the temporal lobe.
The plan is MRI, if it is swollen - difenin, post-traumatic damage - deparkin.
TICKET 19
1. Alternating pontine level syndromes:
Contains a segmental apparatus (gray nucleus) and conductive apparatus (white nucleus). From below it is limited by the medulla, from above it passes into the cerebral peduncles, and its lateral sections form the middle cerebellar peduncles. The substance of the pons contains the nuclei of the V to VIII pairs of cerebral-brain nerves. Nuclei VIII: nucl. cochlearis ventralis et dorsalis; nucl. vestibularis sup, later, med, inf; nucl. ventralis et dorsalis corporis trapezoidei; nucl. lemnisci lateralis. (conducting auditory to the subcortical hearing centers; and vestibular to the spinal cord, cerebellum, medial longitudinal bundle of impulses). Nuclei VII (facial nerve), nucl. solitarius (nucleus of the solitary tract), nucl. salivatorius superior, nucl. facialis, nucl. lacrimalis. Innervates facial muscles, lacrimation, salivation, perception of sensory stimuli (taste, general sensation from the skin of the auricle, external auditory canal, eardrum). VI pair (abducens nerve): nucl.n.abducens: innervates the external rectus muscle, which turns the globe outward. V pair (trigeminal): nucl pontinus nervi trigemini, nucl. motorius n. trigemini (engine). The internal chewing muscle, and its sensory nuclei are carried to the overlying areas of pain and tactile sensation from the skin of the face and mucus of the membranes of the mouth and nose, from the teeth and conjunctiva of the eyes. Bridge nuclei (nucl. pontis), nucl. formatio reticularis.
Clinical syndromes:
Minyar-Gubler syndrome (hemiplegia alternans facialis). Occurs when the pathological focus is localized in the ventral part of the base of the bridge. In this case, the core or fibers of the facial nerve are affected, as well as the pyramidal tract passing here. Clinically manifested by peripheral cutting or paralysis (prosopoplegia) of the facial muscles on the affected side and central spastic paresis of the arm and leg of the opposite side.
Brissot-Sicard syndrome (hemispasimus facialis alternans). It manifests itself as facial hemispasm on the side of the lesion and central paresis of the muscles of the limbs on the opposite side. Facial hemispasm is a consequence of irritation of the nucleus of the facial nerve.
Foville syndrome (hemiplegia alternans abducento-facialis). The clinical picture of the syndrome includes peripheral paresis of the facial muscles on the side of the lesion and paresis of the external rectus muscle of the eye of the same name, and on the opposite side, central paresis of the arm and leg.
Gasperini syndrome occurs with unilateral damage to the anterior part of the rhomboid fossa. The nuclei of the trigeminal, abducens, facial and auditory nerves (V, VI, VII, VIII), as well as the fibers of the medial lemniscus and partially the posterior longitudinal fasciculus are affected.
The pyramidal tract is not affected by this syndrome. Clinically - peripheral paresis of the facial and abducens nerves, the motor portion of the trigeminal nerve, decreased sensitivity on the face and decreased hearing on the affected side. Sometimes nystagmus and Horner's symptom complex are associated. On the opposite side there is conductive hemihypesthesia.
Raymond-Sestan syndrome. It is characterized by damage to the pons involving the pyramidal tract, medial lemniscus, posterior longitudinal fasciculus, and pontocerebellar tracts in the middle cerebellar peduncle. Clinically manifested by cerebellar disorders on the side of the lesion (homolateral asynergia), gaze paralysis towards the lesion, contralateral hemiplegia and hemianesthesia.
“Isolation syndrome”: all arbitrariness of movement is absent (spastic tetraplegia, pseudobulbar palsy with anarthria, aphonia, dysphagia and immobility of the tongue, lack of facial movements), except for vertical movements of the eyeballs and blinking. Causes: thrombosis of the bases of the artery, tumor of the bridge, skull trauma.
Horizontal gaze palsy: near the nucleus of the VI nerve, the pontine gaze center is located, its damage => gaze paralysis towards the focus => the eyeballs deviate towards the preserved center.
Central pontine myelinolysis: characterized by an increase in spastic tetraplegia and pseudobulbar palsy, rapid development of a coma. A focus of demyelination in the central part of the pons (chronic alcoholism).
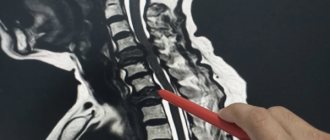
Spinal cord injuries
Includes open and closed damage to structures resulting from direct and indirect exposure to various trauma agents.
Etiology, pathogenesis. Causes: back injuries resulting from car accidents, accidents in production, at home, during sports, iatrogenic effects, gunshot and stab wounds of the vertebrae and the areas closest to them. Fur plays a leading role in pathogenesis. (morphological and functional changes in the tissues of the SM), which for injuries with pressure from spinal formations from bones, ligaments, intervertebral disc matter, foreign bodies, hematomas, as well as sprains, movement. due to hyperflexion of the spine and vascular factors arising in the area of injury and in nearby areas, circulatory disorders and swelling, which aggravate the severity of the primary damage to the spinal column.
Classification: Injuries to the spinal column and spine are divided into open and closed. The causes of open injuries in the vast majority of cases are: injuries. There are penetrating (characterized by a violation of the integrity of the spinal canal with injury to the spinal column by primary (bullets, balls) or secondary (fragments of vertebral bones) wounding projectiles) and non-penetrating wounds (the integrity of the walls of the spinal canal is not compromised, damage to the spinal column occurs due to the transmission of the impact force of the wounding projectile from the vertebrae to the spinal structures).
The main clinical forms of closed brain injuries are: concussion, bruise, hematomyelia (bleeding into the brain) and hemorrhage (bleeding into the membranes).
In the development of a traumatic disease, SM is differentiated: acute, intermediate, or recovery, and late periods.
The acute period lasts for 1-2 months after the injury and is characterized by necrosis of spinal neurons and their processes in places of direct traumatic impact, as well as the development of spinal shock (diaschisis).
The recovery period (up to a year from the moment of injury) is characterized by the beginning of the formation of a post-traumatic scar and the development of regenerative and reparative processes. During this period, the true extent of damage to the spinal cord and the possibility of restoring the existing morpho-functional defect are determined.
In the late period of TB SM, the formation of secondary necrosis, cysts, edematous melting of nervous tissue comes to the fore, rough collagen scars are formed, ascending and descending degeneration of spinal conductors occurs, and infectious and trophic complications develop.
Wedge picture. OPD immediately after injury, most often spinal shock. There is paralysis of the limbs and anesthesia below the level of injury, retention of urination and defecation. The phenomenon of spinal shock is observed for several hours, and sometimes several weeks, after which the clinical caritina is determined by the severity of the damage.
SM concussion is the mildest form of trauma, cat. manifested predominantly sensory disorders of the conduction type below the level of damage, most often in the form of hypo- and parasthesia. Movement disorders include weakness in the arms and/or legs, depending on the injury. Sometimes revealed pelvic disorders in the form of constipation, urinary retention or increased frequency.
All clinical manifestations regress within 2-3 weeks, because There is no mass death of nerve cells and conductors.
SM contusion – injury to the SM, with a cat. Fractures of the vertebral bodies and arches with displacement into the spinal canal and compression of the spinal column are observed. In neurological status: pronounced motor disorders in the form of a center. and peripheral (depending on the level of damage) paresis or paralysis. Below the site of injury there is a conduction-type sensitivity disorder in the form of hypo- and anesthesia. If the roots are damaged, there are shooting pains in the corresponding zones. After a few weeks, in areas where soft tissue can be compressed by bony protrusions, bedsores® infection® sepsis® let.ex..
Dr. complications: urosepsis and pneumonia.
Hematomyelia is a hemorrhage in the brain matter, most often affecting the gray matter of the brain in the area of the cervical and lumbar thickening. In the innervation zones of the affected segments there is flaccid paresis, a disorder of superficial types of senses. Ref. injury depends on the volume and location of the hemorrhage; the function has not fully recovered.
Hematorachis - hemorrhage into the membranes of the spinal cord, caused by trauma to the vertebrae. At the site of the hematoma there is pain when tapping on the spinous processes of the vertebrae, reflex. tension of the paravertebral muscles, pathological fixation of nearby motor segments.
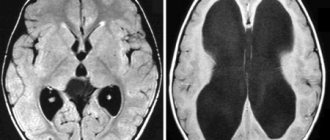
Diagnostics. Clinical and neurological examination and X-ray examination methods - CT, MRI, spondylography, positive myelography and pneumomyelography.
Treatment. Immobilization of the spine, catheterization of the bladder, administration of analgesics and antibiotics, and if hemorrhage is suspected, coagulant solutions. If the spinal column is compressed, urgent surgery is required. Then: corticosteroids, enzymes, immunomodulators, vitamins, antihypoxants, vasoactive drugs, absorbable medications, PT, exercise therapy.
TASK
Clinical DZ – volumetric formation. Tumor of the right frontal lobe.
Topic DZ is a syndrome of damage to the right frontal lobe.
Plan – CT, MRI.
TICKET 20
Brachial plexus
The brachial plexus (pl.brachialis) is formed by the anterior branches of C5-T2 cm.
Arr. 3 bundles: upper C5-6, middle C7, lower C8, T1, T2. Moving under the clavicle and into the axillary cavity, the primary bundles of the plexus are divided into anterior and posterior branches. By connecting with each other, the branches form secondary plexus bundles:
-external (anterior branches C5-7)
-internal (anterior branches C8T1-2)
-posterior (posterior branches of the three anterior bundles)
external sec. the bundle gives rise to the musculocutaneous nerve. The upper peduncle of the median nerve. Parts of the radial nerve.
Int. sec. the bundle forms the ulnar nerve, internal cutaneous nerve of the shoulder and forearm, the lower leg of the median nerve.
Rear sec. bundle of the radial and axillary nerves.
In addition, the brachial plexus forms the nerves of the neck and shoulder girdle (subclavian nerve, anterior thoracic nerves, posterior thoracic nerves, dorsal scapular nerve, suprascapular nerve, subscapular nerve, dorsal thoracic nerve)
Symptoms of damage:
Lesion of the primary upper bundle (C5-6)
Loss of function of the axillary and musculocutaneous nerve, partially the radial nerve. proximal paralysis develops (Herb-Duchenne palsy): the arm hangs like a whip, it is impossible to raise the arm, bend it at the elbow joint, abduct it and turn it outward.
Movements in the distal parts of the arm are preserved. The ulnar flexion is weakened and the carpal-radial R. senses are weakened. broken on the outer surface of the shoulder and forearm. Soreness at Erb's point. (Anteriorly from the sternum-key-nipples we are above the collarbone)
The defeat is primary. beam.
loss of basic function portions of the radial nerve lateral root (upper pedicle) of the median nerve. weakening of extension of the forearm, hand and fingers, pronation of the forearm, opposition of the thumb. Extensor ulnar carpal-radial R. disorder disappears. feelings on the back on top. forearms and on the back of the hand along the rad. edge.
Damage to the primary lower bundle. (Dejerine–Klumpke palsy)
loss of the ulnar nerve, the skin of the internal nerves of the shoulder and forearm, the medulla root (lower peduncle) of the median nerve. nature of distal paralysis: atrophy in the muscles of the hand. flexion of the hand and fingers is impossible. Sensations are affected on the inside of the shoulder, forearm, and ulnar part of the hand.
With high damage to the bundle or roots of the development. Claude-Bernard–Horner sign
(ptosis, miosis, enophthalmos), damage to the second outer bundle. — loss of the musculocutaneous nerve, partial loss of the median nerve (pronation of the shoulder) of the radial nerve (supination of the forearm of the hand)
damage second internal beam
- nar f-ii of the ulnar nerve, skin of the internal nerves of the shoulder of the forearm, median nerve.
Damage to the second rear of the beam
- nar f-th of the radial and axillary nerve.
Total brachial plexus syndrome
- disruption of the functions of all muscles of the shoulder girdle, maintaining a shrug (trapezius muscle and accessory nerve)
2. Rheumatic chorea ( “ trochea” translated from Latin means “dance”).
The disease arose in childhood and adolescence; the main manifestation was choreic hyperkinesis, which begins acutely or subacutely, then spontaneously regresses.
Ethiol:
suffered streptococcal infection, acute rheumatic fever, rheumatic carditis.
MH is one of the forms of rheumatism. Family predisposition Pathogen:
main link: Ab, cross-reacting with both streptococcal Ag and basal ganglia Ag.
Patomorphol MX is a mild generalized encephalitis with non-specific manifestations, namely widespread perivascular infiltration, diffuse degeneration of neurons, basal ganglia, cortex, cerebellum. Clinic:
hyperkinesis, muscle hypotonia, incoordination, mental and vegetative disorders.
Choreic movements: fast, irregular, randomly distributed, most pronounced in the distal parts of the limbs and face. Hyperkinesis of the larynx and tongue, which manifested itself as dysarthria and impaired swallowing. Decreased depth of reflexes, Gordon's phenomenon (prolonged choreic contraction of the quadriceps femoris muscle when inducing the knee reflex). With outstretched arms, a tendency to pronation may be revealed, as well as flexion of the hands with hyperextension in the metacarpal joints and ghosting of the thumb (“choreic hand”). Psychological changes: affective lability, anxiety, impulsivity, impaired concentration, decreased memory. Duration of the disease is from 1 to 3 months. The disease can recur with an exacerbation of the rheumatic process or the presence of factors that allergize the body (pregnancy, hypothermia, hyperinsolation, etc.). Sometimes after suffering from chorea, hyperkinesis in a limited muscle group may be observed for a long time, intensifying with excitement. Hyperkinesis often occurs in the distal parts of the extremities and intensifies with exacerbation of the rheumatic process. Treatment:
in the acute period, bed rest. When combining MX with acute rheumatic fever, Nester anti-inflammatory cf. Strept – bicillin 1,500,000 units 1 time every 3 weeks for 5 years. In severe cases (with active inflammation), a short course of prednisolone at a dose of 1-1.5 mg/kg per day, plasmapheresis, IV Ig. To reduce hyperkinesis, barbiturates, benzodiazepines, etc., for severe hyperkinesis, haloperidol at 1.5-3 mg/day. Mild chorea (paralytic): a variant of minor chorea with severe muscle hypotonia simulating paralysis. Chorea of pregnancy - minor chorea in pregnant women due to exacerbation of the rheumatic process. Huntington's chorea is a genetically determined disease, cathar-yut: progressive course of hyperkinesis, inherited type of disease, late development (35-45 years), increasing dementia. Senile chorea - having developed in old age, there are no inheritances of the disease, in the status it reveals symptoms not only of extrapyramidal disease.
TASK
Character: secondary generalized epileptic seizures.
DZ – consequences of an open head injury, brain injury with the development of secondary epilepsy.
Factors: non-compliance with work and rest schedules, alcohol.
Plan – MRI, CT, EEG, anticonvulsants.
TICKET 21
Diagnostics and therapy
As a rule, the diagnosis of such a disease is made based on the patient’s medical history and external manifestations. In the case of Zakharchenko syndrome, the result is obvious. In addition to examining and interviewing the patient, the doctor must conduct a number of clinical and instrumental tests to exclude other diseases with similar symptoms, including the following:
- MRI of the brain;
- Doppleroscopy of the cervical spine;
- CT head;
- clinical blood test;
- a series of neurological tests.
Confirming the presence of Jacksonian epilepsy in a patient is extremely difficult, since its clinical picture is similar to other disorders. For example, with the myoclonic form of the disease and hysterical seizures. Therefore, during the diagnosis, the neurologist first examines the patient’s medical history, listens to his complaints, and only then sends him for a full examination of the body.
The patient, in addition to standard tests, needs to undergo electroencephalography. Using this diagnostic method, discharges of epileptic activity are detected. Additionally, MRI of the brain is prescribed to differentiate Jacksonian epilepsy from other pathologies (tumors, abscess, encephalitis).
If you suspect Jacksonian epilepsy, a person should consult a neurologist. He will listen to the patient's complaints and then refer him for examinations. People are required to undergo echoencephalography, MRI and CT scans, as well as blood tests. Based on the results of the research, it will be approximately clear what exactly we are dealing with.
For a complete cure, it is recommended to perform neurosurgical intervention, the purpose of which is to remove the pathological focus. If the restoration of nerve tissue is successful, then the symptoms will gradually subside. In this case, you will have to carry out maintenance therapy in order to achieve recovery faster.
If characteristic symptoms appear, a person must immediately consult a doctor and undergo an examination. Even with the help of medications, you can significantly improve your well-being. With the correct selection of medications, the manifestations of the disease will not only not intensify, but will also be significantly weakened.
Pathogenesis
The nuclei of the cranial nerves are located in the cerebral trunk. In the same part there is a pyramidal tract through which impulses are transmitted from the cortex to the neurons of the spinal cord. Sensory and motor nerve fibers intersect at the level of the spinal cord, so the innervation of one part of the body is carried out by nerve pathways that pass in another part of the trunk. If a brainstem lesion occurs involving the nuclei of the cranial nerves, then cross-symptoms appear. Such symptoms also appear with damage to the extra-stem part and motor cortex.
Nothnagel syndrome (syn. quadrigeminal syndrome)
The syndrome occurs with extensive lesions of the midbrain involving the roof, tegmentum and partly the base of the brain - the quadrigeminal plate is affected; red nuclei or superior cerebellar peduncles, nuclei of the oculomotor nerves, medial geniculate bodies, central gray matter in the circumference of the aqueduct of Sylvius.
The main cause of the pathological process is pituitary tumors. Clinical signs and symptoms. At the onset of the disease, signs of cerebellar damage appear: ataxia, intention tremor, choreiform or athetoid hyperkinesis; There is a decrease in hearing on both sides or only on the side opposite to the localization of the lesion.
https://www.youtube.com/watch?v=ytoSdJfFgpg
In some cases, spastic paresis of the limbs develops. Due to bilateral pyramidal lesions, central paresis of the facial and hypoglossal nerves occurs. Eye symptoms are caused by damage to the oculomotor nerves. Bilateral ophthalmoplegia, mydriasis, and ptosis are observed. In the case of a unilateral lesion, the symptoms are more pronounced on the side opposite the lesion.
Causes of the disease
There can be many reasons for this type of disease. Among the most common are:
- Blood supply disorders. This includes hemorrhagic and ischemic strokes, which are the most common causes of alternating syndromes.
- Neoplasms in the brain. If the brain stem is affected by a tumor, compression of the nerve endings occurs, which provokes the development of the disease.
- Inflammatory diseases that are localized in the trunk and act as an impetus for the development of pathology.
- Traumatic brain injury. Very often the disease occurs after damage to the skull.
Complications
Alternating syndromes that appear simultaneously with spastic hemiparesis cause the appearance of joint contractures. This complication has a negative impact on already existing motor disorders. Paresis of the 7th pair of cranial nerves causes a distortion of the face to one side, which is why the patient not only experiences a lot of inconvenience, but also develops many complexes.
If the auditory nerve is affected, the patient will soon develop hearing loss, which can even lead to complete hearing loss over time. Paresis of the 3rd and 4th pairs causes a significant deterioration in vision and the appearance of double vision.
The most serious complication is damage to the brain stem, because It is here that all the most important centers for maintaining life are located. Such patients in most cases die.
Diagnostic methods for determining the disease
The type and presence of cross syndrome can be determined at an appointment with a neurologist. Already as a result of the initial examination, the doctor can judge the prevalence of the pathological process and its severity. If the root cause of this condition is a tumor, then the symptoms will gradually increase every month. If such a condition is caused by an infectious nature, the patient will complain of a change in health for the worse. During a stroke, alternating symptoms always appear suddenly and always increase rapidly.
To identify the root causes of this disease, the patient may be prescribed a series of examinations:
Magnetic resonance imaging. The study allows us to examine the lesion due to the fact that after its completion, specialists can evaluate three-dimensional images in high quality, due to which errors in making a diagnosis are practically eliminated.- Ultrasound diagnostics. One of the most common and accessible methods that provides detailed information about the condition of blood vessels and tissues.
- Neuroimaging of blood vessels. If doctors suspect that a patient has had a stroke, regardless of its type, magnetic resonance imaging of the blood vessels is prescribed. This diagnostic method allows you to identify the exact location of the pathological focus and its severity.
- Cerebrospinal fluid examination. A puncture is taken if an infectious disease is suspected.
Pontine group
Millard-Gübler syndrome appears against the background of damage to the 7th nucleus of the cranial nerves and fibers of the pyramidal tract. Clinically manifested in the appearance of facial paresis and hemiparesis on the other side. In the Brissot-Sicard form, the lesion is located in a similar way, but in this case there is hemispasm on the face. Foville syndrome involves the presence of paresis of the 4th nerve, as a result of which patients develop strabismus. In Gasperini syndrome, nerves 5-8 are affected. Facial paresis, hearing loss, strabismus, and in some cases nystagmus are observed.
Bulbar group
Jackson syndrome occurs when the 12th nerve nucleus, as well as the pyramidal tracts, are affected. In such patients, partial paralysis of the tongue is observed: when protruded, it tilts towards the lesion, there are obvious signs of atrophy, and the articulation of individual sounds is impaired. Hemiparesis is observed on opposite limbs, and in some cases even sensitivity is lost.
Avellis syndrome is manifested by paresis of the laryngeal muscles, vocal cords, and pharynx due to damage to 10-11 nerve nuclei. Such patients very often have speech and voice disorders, and sensitivity in the opposite limbs decreases.
With Schmidt's syndrome, 9-12 nuclei of the cranial nerves are affected, which causes paresis of the trapezius and sternocleidomastoid muscles. In patients on the side that was affected, the shoulder drops significantly, and patients cannot raise their arm up.
Clinic of alternating syndromes
The signs of the disease in each patient are always obvious, which allows the neurologist to make the correct diagnosis after the initial examination. Patients show signs of dysfunction of the cranial nerves on the side of the body where they were affected, and there are various disorders: motor or sensory on the other side. Alternating symptoms can appear either gradually with an increase, or very abruptly and are accompanied by an increase in intracranial pressure and a deterioration in the general condition.
Treatment
Treatment is aimed at eliminating the underlying pathology and includes many techniques:
- Conservative therapy. Patients are prescribed neuroprotective, decongestant and neuroprotective agents. For ischemic strokes, vascular therapy is carried out, for hemorrhagic strokes, calcium and aminocaproic acid preparations are prescribed.
- Neurosurgical treatment. In some particularly severe cases, it is performed for hemorrhagic stroke. The advisability of such an operation should be assessed by a neurosurgeon.
- Rehabilitation. After conservative therapy, patients must undergo a rehabilitation stage, which includes physical therapy, massage and other procedures.