Indications for the study
The presence of a retrocerebellar cyst can be suspected by some characteristic symptoms:
- Severe headaches that do not go away even after taking painkillers;
- Unreasonable loss of consciousness or fainting state;
- Sensation of squeezing and pulsation in the head;
- Deterioration of hearing or vision;
- Arterial hypertension;
- Numbness of the limbs;
- Impaired coordination of movements;
- Epileptic seizures.
Magnetic resonance imaging is required if surgical intervention in the brain area is necessary.
Note that the clinical picture and severity of symptoms depend on the exact location and size of the retrocerebellar cyst.
Treatment
In neurology departments, when treating colloid cysts of the third ventricle, doctors adhere to the following tactics: small formations without symptoms of the disease are not treated, the patient is sent for an annual MRI or CT scan, which evaluates the size of the formation and its tendency to grow.
For large tumors with clinical manifestations or with progressive enlargement of the cyst, consultation with a neurosurgeon is indicated to decide on surgical treatment. During surgery, the cyst is completely removed, the cerebrospinal fluid ducts are cleared, and thereby the syndrome of increased intracranial pressure is eliminated. The following surgical techniques are used: craniotomy and endoscopic removal. Craniotomy is an opening of the skull and open brain surgery; it allows you to completely remove the tumor, examine the cavity of the third ventricle, and restore the cerebrospinal fluid tract. Its disadvantages are greater trauma and cosmetic defects after surgery. Endoscopic removal of a colloid cyst is carried out through a small hole in the bones of the skull using a special apparatus, which allows both to examine the cavity of the third ventricle and to remove the tumor. After surgery to remove the cystic formation and restore the flow of cerebrospinal fluid using modern methods, an almost complete recovery of patients is noted. In rare cases, the pathological process recurs, and then a repeat operation becomes necessary. To prevent the onset of colloid cyst growth in adults, it is necessary to lead a healthy lifestyle.
Contraindications
Magnetic resonance imaging is safe for the body only if all contraindications are excluded.
Magnetic resonance imaging is not recommended in the following cases:
Very often, to obtain more informative images, doctors prescribe additional contrast. In this case, you must ensure that there are no following contraindications:
- Pregnancy of any stage.
- Breastfeeding period.
- Kidney failure.
- Chronic liver diseases.
- Allergic reaction to components included in contrast agents.
Types and stages of the disease
Cystic formations can be single or multiple. They can form in the right and left kidneys, in different parts of the organ. Most often, a cyst forms in the thickness of the tissue or under the kidney capsule. The content is transparent, which indicates the good quality of the process. But there are also hemorrhagic (with blood impurities) and purulent cysts. Their cysts are thin, with signs of chronic inflammation.
There are also simple and complex cysts. The predisposition to simple renal cysts increases with age. They are a spherical cavity with a transparent liquid. They are most common and are considered safe, including with regard to the development of kidney cancer.
Complex kidney cysts differ from simple ones in the presence of segments and chambers, as well as uneven contours. In the case of thick walls, there is a risk of malignant degeneration. The size of a kidney cyst rarely reaches large values.
Depending on the structure, there are:
- Renal sinus cyst. Simple, located at the gate of the renal sinus or the kidney itself. It is more common in women over 50 years of age.
- Parenchymal cyst. Most often it is congenital in nature, in some cases it can resolve. The formation is located directly in the parenchyma of the kidneys, hence the name.
- Solitary cyst. A simple round cyst without inclusions or septa, not associated with the excretory system of the kidney.
Preparation rules
During a routine examination, doctors recommend following a few simple recommendations:
- If it is necessary to administer contrast, you must come to the clinic on an empty stomach, that is, do not eat food for 7-8 hours.
- If you are afraid of research or confined spaces, be sure to consult with a specialist. Your doctor may prescribe you sedatives to make the examination process more comfortable.
- Do not bring any metal products inside the tomograph. For this reason, doctors recommend removing metal accessories in advance.
- Prepare a change of clothes that do not have metal or metal-containing accessories.
- The duration of the diagnostic test is about 40 minutes. Empty your bladder in advance to avoid discomfort during the procedure.
How is an MRI performed?
To ensure that the procedure is as informative as possible and that the images are clear, experts recommend performing magnetic resonance imaging in closed-type tomographs. Before starting the study, the patient must change into clothes without metal structures, take off his shoes and lie down on a retractable table. If the doctor has prescribed additional contrast enhancement, a special drug is injected into a vein, which is distributed throughout the circulatory system in just a few minutes. Then the table moves inside the tomograph, where the research process takes place.
Maintaining immobility is the main requirement for the patient! Remember that even minimal movements can lead to a decrease in the information content of the procedure.
It is also worth noting that when performing magnetic resonance imaging, a specific loud noise is observed. If this scares you, you can use earplugs.
Patients generally tolerate MRI well. Inside the tomograph there is good lighting and ventilation, there is a loudspeaker, as well as a panic button for emergency stop of the study.
The main reasons for the development of dangerous pathology
A cyst on the spinal column can occur due to:
- inflammatory processes in the back areas;
- getting injured;
- strong physical activity;
- inactive lifestyle;
- hemorrhages;
- worm infections;
- lower back pain.
In any case, the appearance of pain in the back should serve as an alarm bell for a person. To prevent further development of the disease and promptly begin treatment of a cyst in the cervical spine, you should consult a specialist doctor.
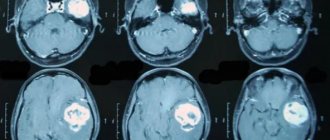
MRI with contrast
In most cases, magnetic resonance imaging of the brain is performed with contrast, especially if any neoplasm is suspected. This makes it possible to examine the tumor in detail and distinguish a benign tumor from a malignant one.
The contrast agent clearly highlights the vessels, which allows you to see any tissue pathologies. Don't worry, contrast agents are safe for the human body. Most patients tolerate this procedure well. You must first consult a doctor and exclude all possible contraindications.
Types of neoplasms
Today, doctors classify cysts depending on their shape, location, causes of appearance, size and structure. According to these factors, the following types of pathology are distinguished:
- Pararticular cyst. Most often, the disease occurs in older people and is localized in the intervertebral joints in the middle and upper parts of the spine.
- The cyst of the cervical spine is ganglionic. The peculiarity of this type of neoplasm is that it affects the cervical and lumbar spine. These areas bear the heaviest mechanical loads.
- Perineural formation. The anomaly is a congenital disorder. The location of the cyst is the lower spine.
- Arachnoid cyst or Tarlov cyst also refers to congenital pathologies. The peculiarity of this type of neoplasm is its location in the canal of the sacral part of the spine.
- Aneurysmal formations. Diagnosed rarely and more often in pediatric patients. The tumor forms in the body of the spinal column itself.
Depending on the degree of development of the perineural cyst of the spine, a treatment method is selected. In most cases, drug therapy, physical therapy, and cyst removal in combination are recommended.
Decoding the results
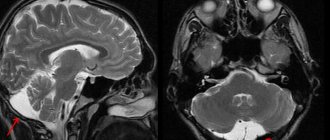
A retrocerebellar cyst is located in the brain behind the cerebellum, in the posterior cranial fossa. During magnetic resonance imaging, it is possible to clarify the exact location and size of the formation.
The report will contain all the information, but the MRI specialist cannot make a diagnosis - this must be done by your attending physician. If the diagnosis of retrocerebellar cyst is confirmed, the doctor will determine treatment tactics. For benign tumors, it is often possible to do without surgical interventions - they are required only in cases of large tumors or rapid growth. To avoid serious consequences, consult a doctor at the first alarming symptoms. Be healthy!
Ovarian cysts
Ovarian cyst is a common diagnosis. However, most often there is nothing to worry about. Most ovarian cysts are benign and go away on their own, but there are exceptions that are best known in advance.
Concept and symptoms
A cyst is a thin-walled formation filled with liquid contents. Sometimes, instead of fluid, there may be blood, fat, or other tissue inside the cyst. Cysts on the ovaries occur at any age, starting from the prenatal period of development of a female fetus, but are more often found during reproductive age.
Sometimes cysts can cause dull, aching pain in the lower abdomen, which appears for no apparent reason, either during physical activity or during sexual intercourse. And it is extremely rare to feel sudden sharp pain in the lower abdomen, nausea, forcing you to immediately seek help. This means that the cyst has ruptured or twisted.
But in most cases, ovarian cysts do not cause any symptoms at all. Doctors discover them by chance during an examination on a chair or during a pelvic ultrasound (PUS). This means that you can’t focus on “it hurts or it doesn’t hurt.” Scheduled examinations by a gynecologist are needed.
Types of cysts and treatment approaches
1. Most often, women encounter functional cysts
, which are divided into:
- follicular cysts
are actually an overgrown follicle, growing up to 3 cm or more; - Corpus luteum cysts
are an overly large corpus luteum with a pronounced fluid component. Such a cyst can accompany pregnancy, providing the fertilized egg with a sufficient amount of progesterone.
Most often, functional cysts are an accidental discovery during an examination or ultrasound examination. Sometimes they can make themselves felt by pain or cycle disorders. In any case, such lesions usually completely regress within 6-8 weeks, in most cases without any treatment.
2. Cystadenomas
- more insidious cysts. They can reach large sizes and look quite scary. Ultrasound reveals papillary growths, parietal inclusions - everything is very impressive. This cyst has a malignant form - cystadenocarcinoma, aggressive and dangerous. Treatment is only surgical.
3. Endometriomas
- “chocolate” cysts, filled with viscous, thick contents reminiscent of melted chocolate. They begin to grow on the surface of the ovary and protrude inward. Treatment is only surgical, but the approach must be differentiated. If the endometrioma is small and does not grow, it will not interfere with pregnancy, and during the operation the ovarian reserve will be severely damaged. If the endometrioma is more than 3 cm, then the reserve will suffer - it will crush and damage good follicles, so surgery is necessary.
Teratomas are sometimes found in the ovaries, as in other organs.
(or
dermoid cysts
) - formations consisting of cells of nails, hair, skin, teeth, fat and other passions. The tissues within a teratoma are ALWAYS foreign to the anatomical location (in this case, the “dental tissue” in the ovary is clearly not in place). Teratomas do not resolve in any way; their drug treatment is completely pointless. If the teratoma is very small, it can be monitored using ultrasound. But if the size of the formation is more than 3 cm, treatment is only surgical. Teratomas have a malignant form (immature teratoma that can grow into surrounding tissues and metastasize), so you should not delay the operation.
Polycystic ovary syndrome
is not “horror, horror, a lot of cysts.” This is a completely different disease, which we have already talked about.
In fact, there are many more types of ovarian tumors—several dozen. The final diagnosis, answering the question of what kind of cyst we encountered this time, will be given by a pathologist who will examine the removed tissue and give a histological conclusion. Based on this conclusion, the attending physician will build a further treatment/observation plan.
This is why it is so important not to be lazy and go “for histology” in a couple of weeks or make sure that the conclusion is sent to you by mail. You will then show these documents to your attending physician. But general phrases like “they said that the histology is good” will certainly please the attending physician, but will not help him make important clinical decisions.
Should we observe or operate?
If the cyst is large (more than 5 cm), has a suspicious echostructure, or causes pain, surgery will be the right choice of treatment. Observational tactics depend on the woman’s age, ultrasound picture and the level of the Ca-125 tumor marker.
During reproductive age, if the cyst does not bother the patient in any way, the doctor may suggest repeating the OMT ultrasound in 6–8 weeks. In most cases, the cyst will disappear or shrink in size. If the cyst does not increase in size and its structure does not change over a long period of time, observation can be continued.
In postmenopause, the risks increase, you will have to be examined more often - after 55 years, even a small, seemingly harmless cyst can turn out to be cancer at an early stage, discovered by chance. Therefore, we will need a tumor marker test and frequent monitoring until we are sure that it is not cancer. For diagnosis, the most important thing is that cancer grows: everything that does not grow is not cancer.
What if we miss cancer?
This question always worries both the doctor and the patient. Unfortunately, the world has not yet come up with any method of screening for ovarian cancer. Perhaps because this disease is very diverse and has dozens of varieties. Unfortunately, the diagnosis of ovarian cancer is made almost by accident or late - when a huge belly filled with fluid has grown and pain has appeared. This is why the doctor will be especially picky about any ovarian cysts in high-risk patients:
- age over 55 years;
- family history of breast cancer, ovarian cancer, colon cancer, or endometrial cancer;
- personal history of breast cancer;
- mutations in BRCA1/BRCA2 (see the story about Angelina Jolie and cancer);
- absence of childbirth;
- infertility;
- endometriosis;
- Lynch syndrome (hereditary colon cancer without polyposis).
Tumor markers: urgently?
Many patients place excessive hopes on determining the level of the tumor marker Ca-125 in the blood. Not long ago, they even tried to use this indicator as a screening indicator, including it in the medical examination program.
Unfortunately, ovarian cancer is not diagnosed based on the results of the Ca-125 test, because a normal result does not mean that there is no cancer - that’s just it. Ca-125 can be elevated in other diseases (for example, endometriosis, heart failure, inflammatory diseases, liver and kidney diseases) - to name two. Nevertheless, a significant increase in this marker is diagnostically important. Most likely, cancer has actually been detected. But the norm or a slight increase does not provide information about the presence or absence of cancer.
Ca-125 can be looked at if an ovarian cyst is discovered in postmenopause, if a young woman has a very large cyst or its ultrasound picture is suspicious. There is a whole group of tests for tumor markers that can be used, but the results of these examinations should be treated with great caution. Tests are performed every 3 to 6 months until the cyst disappears or until a decision is made about surgery.
Oksana Bogdashevskaya
Photo istockphoto.com