What is high intracranial pressure?
The pressure of intracranial contents (substance of the brain and spinal cord, blood and cerebrospinal fluid - cerebrospinal fluid) on the walls of the skull is called intracranial. Liquor circulates in the cerebrospinal fluid pathways: the subarachnoid space and the ventricles of the brain (Fig. 1). If his pressure rises above 10-12 mm Hg. Art., intracranial hypertension occurs. It can manifest itself as depression of consciousness, headache, nausea and can cause damage to brain tissue. If the pressure continues to rise, at 30-40 mm Hg. Art. a person most often falls into stupor (a sharply inhibited state), at 40-50 mm Hg. Art. - in a coma of varying depth.1
Figure 1. Cerebrospinal fluid circulation. Source: OpenStax / Wikipedia (Creative Commons Attribution 4.0 International license)
Intracranial hypertension occurs in children and adults. In infants under one year of age, it is almost always associated with hydrocephalus or birth trauma. In adults, common causes are head injuries and conditions that increase the volume of brain tissue or the cerebrospinal fluid and blood circulating inside the skull.
Basic Concepts
Intracranial pressure is the difference between pressure in the cranial cavity and atmospheric pressure. Normally, this figure in adults ranges from 5 to 15 mmHg. The pathophysiology of intracranial pressure follows the Monroe-Kelly doctrine.
This concept is based on the dynamic balance of three components:
- Brain;
- Cerebrospinal fluid;
- Blood.
A change in the pressure level of one of the components should lead to a compensatory transformation of the others. This mainly occurs due to the properties of blood and cerebrospinal fluid to maintain a constant acid-base balance, that is, to act as buffer systems. In addition, brain tissue and blood vessels have sufficient elasticity, which is an additional option for maintaining this balance. Due to such protective mechanisms, normal pressure inside the skull is maintained.
If any reasons cause a breakdown in regulation (the so-called pressure conflict), intracranial hypertension (ICH) occurs.
In the absence of a focal cause for the development of the syndrome (for example, with moderate overproduction of cerebrospinal fluid or with slight venous discirculation), benign intracranial hypertension is formed. Only this diagnosis is present in the international classification of diseases ICD 10 (code G93.2). There is also a slightly different concept - “idiopathic intracranial hypertension”. In this condition, the etiology of the syndrome cannot be established.
Causes of increased intracranial pressure
Intracranial pressure may increase due to the following reasons:
- Swelling of brain tissue due to injury, hypoglycemia, hyponatremia, the development of hypoxia as a result of a stroke, inflammation due to encephalitis or meningitis, poisoning.
- Increase in volume: when foreign bodies enter, tumors appear, hemorrhage (subdural or epidural hematoma, intracerebral or subarachnoid hemorrhage).
- Development of hydrocephalus: an increase in the volume of cerebrospinal fluid in the cranial cavity.
- Venous congestion: accompanies congestive heart failure and can develop with thrombosis of the cerebral veins.
- Increased cerebral blood flow during epileptic seizures, cerebral hyperperfusion (develops after ischemic strokes, surgical interventions, injuries).
Reasons for appearance
Intracranial hypertension has no specific causes. However, it is associated with the following problems:
- Brain changes: hematomas or tumors, which over time begin to increase in size and compress the tissues located around them, causing intracranial pressure.
- Any injuries to the skull or brain (even 20 years ago). They can provoke an increase in cerebrospinal fluid pressure years later.
- Pathological processes leading to cerebral swelling. A striking example of these deviations: encephalitis, hydrocephalus, meningitis.
- Chronic pulmonary diseases, heart failure.
- Improper blood circulation due to a malfunction of the vascular functioning of the brain.
Excess body weight can also be a source of intracranial hypertension. In this case, you can contact a nutritionist who will prescribe therapy that promotes rational weight loss. As a result, the cerebrospinal fluid pressure will return to normal.
Benign intracranial hypertension can appear as a result of excess/insufficient amounts of vitamins inside the body, as well as during pregnancy.
To determine the origin of hypertension, the doctor considers the factors described above that provoke compression of the arteries of the head. Effective therapy is prescribed after determining the source of the disease.
Who is at risk?
The most common cause of increased intracranial pressure is considered to be traumatic brain injury. At risk are people for whom the risk of such injuries is increased (for example, due to professional activities or playing contact sports). Also, the likelihood of developing intracranial hypertension is higher for people with high blood pressure and the risk of ischemic stroke.
For children in the first year of life, the risk of high intracranial pressure is associated with hydrocephalus - water on the brain. It can be congenital and caused by disturbances during intrauterine development or acquired, resulting from birth trauma or infection.
What are the risks of increased intracranial pressure? Complications and consequences
The brain is the highest energy system in the human body. It needs approximately five times more oxygen than the heart. Therefore, the quality of blood supply to the brain is a vital indicator that depends on two parameters - blood pressure and intracranial pressure. At constant blood pressure, the lower the intracranial pressure, the better the blood supply to the brain. If for some reason intracranial pressure increases, this proportionally worsens the blood supply to the brain, and ischemia develops. Therefore, high intracranial pressure is a dangerous condition that can cause the following complications:
- reduction and complete loss of vision;
- convulsions;
- acute cerebrovascular accident;
- depression and/or disorder of consciousness;
- depression of respiratory and circulatory function.
Important! With a rapid increase in intracranial pressure, there is a threat of death. If the symptoms are severe or appear sharply, suddenly and rapidly increase, you need to call an ambulance.
What is hydrocephalus of the brain, external hydrocephalus
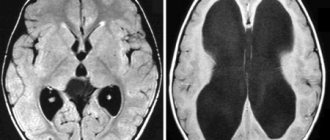
If intracranial pressure is increased significantly and for a long enough time, the fluid cavities of the brain may expand; this expansion is called internal or external hydrocephalus. Since the cranial cavity is a closed space, the expansion of the fluid cavities of the brain occurs due to a decrease in the mass of the brain matter itself. To protect you from the death of working brain tissue, we will offer you a course of medications, in combination with a set of exercises to reduce intracranial pressure and, if necessary, osteopathic correction.
External hydrocephalus (brain) - expansion of the external cerebrospinal fluid spaces of the brain (subarachnoid spaces).
Internal hydrocephalus (brain) - expansion of the internal liquor cavities of the brain (ventricles).
Our clinic pays great attention to finding the root causes of such a condition as increased intracranial pressure. In this case, treatment can be kept to a minimum, and our assistance to patients will be reliable.
Symptoms indicating high intracranial pressure
One of the symptoms of increased intracranial pressure is morning headache.
Photo: AndrewLozovyi / Depositphotos Symptoms can vary greatly depending on how high the blood pressure is, as well as the causes of this condition, the speed of its development and concomitant diseases.
Main features:
- headache;
- nausea or vomiting;
- vision becomes blurred and there may be double vision;
- confusion;
- problems with movement or speech;
- restlessness, anxiety, fear or irritability.
With intracranial hypertension, only some of these symptoms may appear.
They can develop gradually or grow rapidly over several hours or minutes. If blood pressure rises quickly, a person may lose consciousness and fall into a coma (Table 1). Table 1. Symptoms of high intracranial pressure.
| Intracranial pressure (mmHg) | Symptoms |
| 20-30 | Headache, nausea and vomiting, drowsiness, anxiety, psychosyndrome (impaired memory, thinking and emotional reactions), high blood pressure, decreased heart rate, convulsions |
| 30-40 | Sopor |
| 40-50 | Coma of varying depths |
| >50 | Threat of brain death |
Headache with increased intracranial pressure has several features:
- It appears after waking up in the morning, worsens when lying down, and is localized in the back of the head, temples, and forehead.
- The pain is strong, pressing or bursting.
- Painkillers cannot relieve pain.
- Sneezing and coughing, physical activity or lying down provoke attacks of pain.
How to determine intracranial pressure in a child?
In children in the first year of life, intracranial hypertension may appear due to birth trauma, against the background of hydrocephalus (Fig. 3) or swelling of brain tissue.
In older age, traumatic brain injury is a more common cause. Figure 2. Hydrocephalus in children. Source: Journal of Neurosciences in Rural Practice / Open-i (Attribution-NonCommercial-ShareAlike 3.0 Unported (CC BY-NC-SA 3.0)
High intracranial pressure in children of the first year of life has several characteristic signs:
- The shape of the head changes; the bone plates that form the skull can move apart.
- The fontanel protrudes outward and pulsates.
- Increase in skull volume.
- Restless behavior, constant crying, or drowsiness and lethargy.
- Frequent regurgitation or severe vomiting.
- Trembling chin.
- Convulsions, loss of coordination of movements of the arms and legs.
- Visual impairment, limited range of rotation of the eyeballs, strabismus.
- Depression or loss of consciousness.
If these symptoms appear suddenly and increase quickly, you should immediately call emergency medical help.
Diagnosis of intracranial pressure
During diagnosis, the doctor will conduct a general examination, measure blood pressure, and check how the pupils react to light. He will need to talk about the existing symptoms, how long ago and how often they appear, as well as any concomitant diseases. After this, the neurologist will prescribe instrumental diagnostics. It is carried out in two directions:
- brain imaging;
- measurement of intracranial pressure.
Brain imaging is needed to obtain information about the cause of hypertension, how common this process is, and what complications there are. At this stage of diagnosis, a tumor, areas of impaired circulation of cerebrospinal fluid, and signs of strangulation can be identified. Computed tomography or magnetic resonance imaging is performed for imaging. When examining children under 1 year of age, an ultrasound scan of the brain is performed.
Measuring intracranial pressure is possible in one of three ways:
- intraparenchymal;
- intraventricular;
- extracerebral.
All three methods are invasive, require the installation of a special sensor, and are used only in a hospital setting. With such monitoring, external ventricular drainage is sometimes additionally provided, which helps control intracranial pressure (Fig. 3).
Figure 3. External ventricular drainage. Source: Children's Health Queensland, Dermatology reports / NCBI (Creative Commons Attribution 3.0 License (by-nc 3.0)
Noninvasive methods for measuring intracranial pressure do not provide accurate values, but they can be used to confirm hypertension. Among such methods are fundus examination and transcranial Doppler sonography. An ophthalmologist performs a fundus examination. He assesses the condition of the optic nerve and uses it to draw a conclusion about the level of intracranial pressure. Transcranial Doppler is an ultrasound examination that evaluates blood flow in the vessels running inside the skull.
Which doctor should I contact?
If symptoms of liquor-hypertensive syndrome appear, you should contact a neurologist. An experienced specialist can be seen at the medical office by appointment. You can make an appointment by phone @. The doctor will see you at a time convenient for the patient.
The neurologist from the SmartMed clinic has many years of experience in treating noise in the head of various origins, including those caused by intracranial hypertension. To determine the cause of poor health, the doctor will conduct a visual examination.
The examination begins with a study of the patient's complaints and neurological testing. It is important for the doctor to know the person’s medical history, conditions of occurrence, frequency and intensity of noise in the head.
Increased VChP cannot be determined by external signs
The doctor must prescribe instrumental research methods:
- Spinal or lumbar puncture. Designed not only for studying cerebrospinal fluid, but also for measuring intracranial pressure. The procedure is invasive and involves inserting a puncture needle into the spinal canal and then connecting a pressure gauge.
- MRI of the head. Allows you to identify the causes and signs of intracranial hypertension: cerebral edema, vascular thrombosis, enlargement or narrowing of the cerebral ventricles, cysts, tumors, hematomas, hemorrhages. The study is the most informative and safe. In medical MRI of the head, it is carried out on a new ultra-precise Siemens Symphony 1.5 Tesla tomograph, thanks to which it is possible to obtain a highly accurate 3D image. The examination takes no more than 15 minutes, no special preparation is required.
- Ultrasound of the head. Used for children of the first year of life. The study is carried out through an open fontanel.
- Ultrasound of the vessels supplying the brain. Allows you to assess the condition of the arteries, as well as the direction, speed and intensity of blood flow in them, to identify the main vascular disorders that can cause high ICP and noise in the head.
- Electroencephalography. Designed to study the electrical activity of the brain, it allows you to identify areas of irritation of various brain structures.
Additionally, the neurologist may prescribe a consultation with an ophthalmologist. Papilledema, which can be detected during fundus examination, is a sure sign of increased ICP. If necessary, other highly specialized specialists are involved in the examination: a neurosurgeon, an oncologist.
Important! The reliability of the examination for intracranial pressure depends on the technical parameters of the diagnostic equipment and the qualifications of the diagnostician.
Treatment of intracranial pressure
Intracranial hypertension is treated by reducing the pressure to 20 mmHg. Art. or lower and stabilizing the patient's clinical condition. To achieve this, therapy is carried out in several directions.
Conservative approach:
- Maintaining the correct position of the patient (lying position, body elevated by 30 degrees, head position straight).
- Hardware ventilation for breathing problems.
- Reducing body temperature if it is elevated.
- Reducing blood pressure with antihypertensive drugs.
- Reducing stress: stopping vomiting, coughing, eliminating factors that provoke a rise in blood pressure, including shivering from cold, careless transportation, pain and others.
After diagnosis, the cause of hypertension is eliminated. This may require removal of an aneurysm or tumor, bypass surgery, or other major interventions. If there is excess volume of cerebrospinal fluid, punctures are performed to reduce it. After the main stage of treatment, rehabilitation is carried out. The doctor will prescribe medications, diet therapy, and tell you how to adjust your lifestyle.
Prognosis and prevention
When driving at high speed, wearing a helmet is mandatory.
Photo: Paha_L / Depositphotos Increased intracranial pressure is most often associated with head injuries. To prevent them, you need to take precautions: wear a seat belt in a car, use a helmet when riding a bicycle, and reduce the risk of falls.
If there are signs of hypertension, you should see a doctor as soon as possible. The earlier treatment is started, the lower the risk of serious health consequences.
Facts and myths about increased intracranial pressure
There are several misconceptions about intracranial hypertension:
- It does not need to be treated; the condition will go away on its own with age. In fact, both children and adults need treatment to avoid serious complications.
- The condition cannot be treated. False: Treatment results depend on the cause and severity of hypertension. Even if it cannot be completely cured, therapy greatly improves the condition and reduces the risk of health consequences.
- High intracranial pressure always causes developmental delays in children. This is a myth: with timely treatment, such consequences can be avoided.
It is important to know that:
- High intracranial pressure in children most often occurs due to hydrocephalus and birth injuries.
- Homeopathic or herbal preparations do not affect blood pressure in any way and do not help normalize it.
- If a person already has intracranial hypertension, he needs to be examined by a neurologist at least once every two years.
Modern methods of treatment
In some cases, the patient does not require treatment; he is observed and treated for the underlying disease, which caused the increase in ICP.
If it is necessary to treat pathology, two approaches are used - conservative and surgical.
Conservative interventions are carried out for those patients whose ICP elevation is chronic and there is no significant deterioration of the condition over time. The basis of treatment is drugs that have a diuretic effect, which reduce the volume of fluid in the head. The specific medicine is determined by the level of pressure and the situation. In severe and acute processes, osmotic diuretics (mannitol) are used, in chronic cases - furosemide, hydrochlorothiazide, spironalactone. While taking them, you need to drink a potassium preparation - Asparkam, Potassium orotate, Panangin.
Surgical methods for treating increased ICP depend on the stage and severity of the disease. In acute situations, craniotomy is performed to reduce fluid pressure on the brain and drain excess fluid. Special shunts (tubes) are installed as planned, which drain fluid from the brain into the abdominal cavity.