Hemangioma
– a common benign tumor of vascular tissue. Outwardly it resembles a bright crimson or red formation that rises above the skin. Its surface is lumpy and uneven, sometimes it heats up on its own for a short period of time.
Hemangioma in adults cannot provoke any serious disturbances in the functioning of the body, but everything depends on the location of the growth and its size. Hemangioma located on internal organs, such as the kidneys or liver, can cause mechanical compression, which leads to impaired functional activity.
Where does hemangioma appear?
In 80% of cases, hemangioma in adults, a photo of which you can easily find on the Internet, occurs in the form of a single structure; in the remaining cases, several such elements are observed in one place at once. Very rarely, the lesion occurs in the area around the ear.
There are cases when hemangioma occurs on the lip of adults, which causes a lot of inconvenience and discomfort. Also, such lesions can be located in the genital area. This course of the disease is considered the most dangerous, as it is often accompanied by bleeding, infection, and ulceration. Most often, this lesion occurs in the neck or head:
- On the eyelids and around the eyes.
- On the cheeks: both on the outer and inner sides.
- In the region of the nose.
- Near the hairline.
Often vascular hemangioma in adults spreads throughout the body. It can also affect internal organs, which can be detected by ultrasound and computed tomography. If you begin to notice that a hemangioma has begun to grow on your skin, consult a doctor immediately. The sooner you start treatment, the easier and faster it is to get rid of the problem.
Statistical report
In the general group of all intracranial primary tumors, cerebral hemangioblastomas (CHBs) account for 1%-2.5%, and more often (85%) they are diagnosed in the cerebellar hemispheres. The prognosis after complete (!) surgical removal of a tumor with a sporadic occurrence scenario is positive, they do not recur .
But in 25% of cases, the neoplasm is detected as a manifestation of a hereditary disease - Hippel-Lindau disease. Cerebral tumor associated with this disease often has a poor prognosis. In patients with such a genetic pathology, the tumor process can resurface even after complete resection, and not necessarily in the same place; it can appear in any other part of the central nervous system.
The greatest number of cases with HGM is observed in men, who suffer from them 1.5-2 times more often than women. The peak age range when lesions are detected in patients is 40-50 years. For the first time, a neoplasm combined with Hippel-Lindau disease appears in adolescence and young adulthood (up to 30 years).
Hemangioblastomas are characterized by slow growth and benign biological behavior. However, sometimes (rarely) they are complicated by spontaneous significant hemorrhages in the posterior cranial fossa. Massive hemorrhages usually occur with large tumor sizes (more than 1.5 cm).
Any hemangioblastoma in the brain is a serious problem that requires timely detection and treatment. In every patient, the tumor becomes the cause of progressive neurological deficit and a non-stop decline in quality of life. Mortality is not excluded. Unfortunately, this diagnosis cannot be treated conservatively. The only chance for the patient to survive and recover is purely neurosurgical intervention.
Causes
To date, doctors have not been able to determine the exact cause of why hemangioma occurs in adults on the arm or any other part of the body.
The nature of the congenital form of the lesion is as follows: during the period of growth, the body produces an excessive amount of connective tissue, which is why it has to become denser. The luminaries of modern medicine do not have the necessary equipment that would allow them to identify hemangioma on the body in adults in the early stages, a photo of which you can easily find on the Internet.
A hemangioma on the leg of an adult, which manifests itself as a bright red tumor, will not grow over time or torment you with unpleasant sensations. It is not known for certain what causes an adult body to manifest such an ailment on the skin. Common causes of hemangioma in the adult population include:
- Hereditary predisposition.
- Environmental influence.
- Diseases of internal organs, in particular the endocrine system.
- Disorders in the cardiovascular system.
- Exposure to sunlight or ultraviolet radiation.
Kinds
There are 11 types of benign meningiomas:
- meningothelial meningiomas – 60%;
- transitional meningiomas – 25%;
- fibrous meningiomas – 12%;
- rare types of meningiomas – 3%.
A brain tumor can be located in different areas of the brain:
- convexital tumor – 40%;
- parasagittal – 30%;
- basal location of the tumor – 30%.
Meningioma of the brain of the frontal lobe
Meningioma of the frontal region forms very often, in most cases it does not bother the patient for a long time. If the meningioma is located in the right frontal lobe, symptoms will appear on the opposite side of the body.
The reasons for the development of meningioma of the frontal region are various: traumatic brain injury, inflammatory disease of the meninges, genetic predisposition, food high in nitrates, neurofibromatosis and other reasons. Radiation exposure is considered a proven cause of tumor development; all other causes are considered risk factors.
Meningioma of the frontal region can cause blurred vision, headache, paresis of the facial nerves, arm muscles, lethargy and other symptoms.
Anaplastic meningioma
Anaplastic meningioma is a grade 3 brain tumor; tumor recurrence occurs in all patients within three years after treatment.
Parasagittal meningioma
Parasagittal meningioma is located in the occipital, parietal or frontal part along the longitudinal midline. Often this tumor is accompanied by a pathological increase in the content of bone matter in the bone tissue. Parasagittal meningiomas, growing in the frontal part of the head, cause:
- increased intracranial pressure;
- development of congestive optic discs in the fundus;
- severe nausea and vomiting, headache;
- epileptic seizures.
Parasagittal meningioma of the parietal region of the head is characterized by sensory disturbances and epileptic seizures. Meningioma of the occipital region is characterized by increased intracranial pressure and hallucinations.
Atypical meningioma
Atypical brain meningioma is a grade 2 tumor; tumor recurrence occurs in 30% of patients within 10 years after treatment.
Meningioma falx
A tumor growing from the greater falciform process of the brain is called falx meningioma. Over time, the tumor grows into the sagittal venous sinus, resulting in impaired venous circulation and intracranial hypertension. The growth of the tumor causes the following negative symptoms: epileptic seizures, impaired sensitivity and motor activity of the legs, pelvic disorders.
Symptoms of hemangioma in adults
Hemangioma of the skin is quite difficult to recognize in the initial stages. At first, you will be able to notice how your skin begins to gradually turn red, small spots of irregular shape appear on it, which can be easily picked out. Over time, they unite into one large formation with a large tumor point in the center, from which all the small blood capillaries diverge.
It should be noted that hemangioma on the head of an adult develops quite quickly; it grows to its peak state in 2-3 weeks.
There are several types of hemangiomas, which are differentiated by location and manifestation of symptoms. Most often, simple, cavernous, combined and mixed types are distinguished. Only a qualified specialist can determine what has affected your skin. Sometimes a hemangioma can occupy significant areas on the human body, causing serious discomfort.
Signs of pathology
The first manifestations of the tumor process in 90% of patients are general cerebral symptoms characteristic of intracranial hypertension, these are:
- severe headaches (usually in the back of the head);
- nausea, vomiting;
- forced head position (a person intuitively tilts his head to the side to facilitate the conditions for liquor outflow);
- blurred vision.
A feature of clinical signs, as a rule, is increasing or wave-like dynamics with long light intervals. Then, after a few months, focal signs join the symptoms of ICH, these are:
- movement coordination disorder;
- instability, unsteadiness of gait;
- pyramidal insufficiency;
- speech motor disorders;
- involuntary pendulum-like eye movements;
- mental disorders (neurasthenia, depressive neurosis, dysphoria, personality disorientation, etc.).
The listed clinical picture, based on the symptoms of ICH and cerebellar disorders, is characteristic of many cerebral pathologies. Therefore, they cannot be called pathognomonic, that is, specifically for angioreticularis. This fact does not apply only to patients with Hippel-Lindau disease, in whom this symptomatic complex is always combined with retinal angiopathy. In any case, the final diagnosis can be established only after a comprehensive diagnosis, including examination by a neurologist and ophthalmologist, MRI/CT, and selective angiography.
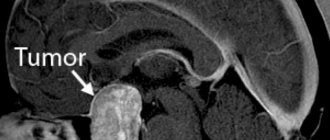
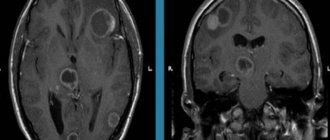
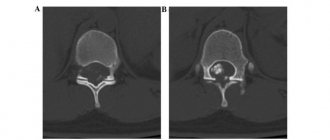
Education on MRI images.
Treatment
Hemangioma on the skin does not pose any danger to the body other than aesthetic discomfort. However, if such a formation begins to grow, it can lead to some negative consequences, such as infection, blood loss, impaired blood clotting, and an effect on some internal organs. In rare cases, tumors disappear on their own; in others, measures need to be taken.
At the Healthy Skin Center, experienced specialists using modern diagnostic methods will easily select for you an effective and safe treatment that will save you from hemangioma on the skin forever.
At the Healthy Skin Center, you will be offered a radio wave surgery method to get rid of hemangioma. This effect allows you to achieve both clinical and cosmetic effects. After exposure to a demato-oncological magnifying glass, no scars or cicatrices remain on the skin. Under the influence of high-frequency radiation, the affected cells completely evaporate, which protects the treated area of skin from the subsequent development of hemangioma.
Contact the Healthy Skin Center, they will always help you.
Radiosurgery
Stereotactic radiosurgery is recommended for a separate group of patients for whom classical surgery is contraindicated due to health conditions or the dangerous location of the tumor. Radiosurgery is also prescribed after incomplete surgical excision of hemangioblastoma in order to eliminate its remaining elements. In the arsenal of neurosurgery, there are 2 methods of stereotactic exposure (without incisions, trepanation and without pain) - Gamma Knife and Cyber Knife.
- Gamma Knife is a radiological procedure specifically designed to specifically destroy abnormal structures within the brain using Cobalt-60 ionizing radiation. Before the operation, a helmet system is put on the patient’s head, which makes it possible to accurately determine and neutralize the focal area. The radiation “works” strictly within the tumor and does not cause harm to nearby healthy brain structures. To install a stereotactic structure on the head, local anesthesia with a long-acting local anesthetic is performed locally (in the places where it is fixed). The course of Gamma Knife therapy consists of 1-3 procedures. Time of 1 session – 30-180 minutes.
- Cyberknife is a procedure for targeted irradiation of pathological tissues using a robotic installation that generates 6 MeV photon radiation. The principle of therapeutic action and effectiveness are approximately identical to the Gamma Knife. But the CyberKnife radiosurgical device, unlike the Gamma installation, is universal. It can be used to treat oncology in different parts of the human body. During this procedure, you do not need to place your head in a frame, and no anesthesia is required.
Contraindications to Gamma Knife and CyberKnife surgeries are tumors that have reached a size of 3.5 cm or more.
Hemangioma
Hemangioma is a benign vascular tumor. Depending on the damage to the vessels, capillary, arterial, arteriovenous and cavernous forms are distinguished.
- Capillary hemangioma
- Arterial hemangioma
- Arteriovenous hemangioma
- Cavernous hemangioma
Capillary
– presented in the form of spots, slightly protruding above the skin level, of varying diameters, from bright pink to bluish-purple. A variant is telangiectasias (“spider veins”), in which rays – stripes, like cobwebs – diverge from the spot.
Arterial
– is a spot from pale to deep pink, clearly demarcated, with superficial localization a pulsation is detected.
Arteriovenous
The form is distinguished by a large affected area (up to 10 cm in diameter), superficial location, bluish-purple color, tortuous bundles of blood vessels, thinning and easy bleeding.
Cavernous
– develops in newborns and increases as the child grows. It is presented in the form of a single formation, which has a lobular structure and protrudes above the skin level like a “mulberry”, bluish-purple in color. There is no favorite localization; it can spontaneously regress.
Clinical picture of the disease
The clinical picture of the disease largely depends on the location of the formations. The most typical clinical manifestations of cavernomas are epileptic seizures and acutely or subacutely developing focal neurological symptoms. The latter can occur both against the background of general cerebral symptoms and in their absence. In some cases, the reason for examination is nonspecific subjective symptoms, most often headaches. In some patients, all these manifestations in various combinations are possible. Epileptic seizures are typical for patients with supratentorial cavernomas, in which they occur in 76% of cases, and when cavernomas are localized in the neocortex - in 90%. The course of the epileptic syndrome is varied - from extremely rare seizures to the formation of drug-resistant forms of epilepsy with frequent seizures. Focal symptoms are typical for cavernomas of the deep parts of the cerebral hemispheres, brain stem and cerebellum. The most severe picture can develop with cavernomas of the diencephalic region and brain stem, which are characterized by the formation of alternating syndromes, including severe oculomotor disorders, pseudobulbar or bulbar symptoms. Repeated hemorrhages in this area lead to permanent disability. With a certain localization of the cavernoma, the clinical picture may be due to occlusion of the cerebrospinal fluid pathways. Asymptomatic cavernomas are usually discovered during examination for some other disease, during preventive examinations, as well as during examination of relatives of patients with clinically manifested cavernomas.
Diagnosis and treatment of hemangioma
Diagnostics: Skin ultrasound, deep dermatoscopy, cytology.
Treatment: removal using radiosurgery.
In our center, tumor removal is performed by a dermato-oncologist using radio wave surgery under local anesthesia.
In order to remove the formation more efficiently, the doctor uses a dermato-oncological magnifying glass, which allows for more detailed and complete removal of skin tumors without leaving pathological cells in the wound. Therefore, after removal, we can say with complete confidence that the formation has been completely removed and you will no longer have it. Read more about tumor removal in our center...
The cost of removing a single hemangioma starts from 900 rubles.
Surgery for brain hemangioblastoma
During a conventional operation, which is the “gold standard” for this diagnosis, the tactics of craniotomy are used to create a retrosigmoid approach. Trephination is performed in the area of the foramen magnum; the diameter of the trepanation window is 2-4 cm. The surgical process occurs under the control of an ultra-powerful intraoperative microscope. The operation to completely remove the GBM lasts from 2.5 to 5 hours. Let's consider the main stages of surgical intervention.
- The hair from the scalp in the appropriate area is first shaved.
- In most cases, combined general anesthesia with tracheal intubation and artificial ventilation is chosen for pain relief.
- The patient's position is on his side or stomach, with his head turned to the side. The head is fixed using a special bracket with spikes.
- A longitudinal skin incision is made within the surgical field or a skin flap is cut out and then folded over the mastoid process of the temporal bone.
- Next, a bone hole is formed in the trephinated part of the occipital bone (downward and medial to the sigmoid sinus).
- At the next stage, the neurosurgeon performs a correct opening of the dura mater. After opening the dura mater, access to the surfaces of the cerebellum and other structures of the PCF is freed.
- The specialist begins the process of eliminating the tumor focus with complete preservation of functionally significant brain structures.
- The hemangioblastoma node is removed completely as a single block. All vascular formations feeding the neoplasm are coagulated and intersected as close as possible to its surface.
- If the tumor is a cyst, its contents are carefully aspirated. The walls of the cysts are not removed.
- At the end of the surgical session, the dura mater is sutured, bone fragments are returned to their place and strengthened, and the skin wound defect is closed.
Click on the link to watch a video of the operation to remove hemangioblastoma
The goal of an open operation is to remove the solid component completely, without any residue. It can be completely removed in most cases, in 85-90% of patients. In this situation, we can expect favorable forecasts with a high degree of confidence. But! If partial or subtotal resection is performed, the tumor will continue to grow. It is noted that incomplete removal often leads to the development of hydrocephalus, hemorrhages and hematomas, and death in the very early period.