Werdnig-Hoffmann genetic disease belongs to the group of spinal amyotrophies and is inherited in an autosomal recessive manner.
Spinal muscular atrophy (SMA) is characterized by congenital or acquired degenerative changes in the striated muscles, symmetrical muscle weakness of the trunk and limbs, absence or reduction of tendon reflexes while maintaining sensitivity.
Morphological studies reveal pathology of motor neurons of the spinal cord , “fascicle atrophy” in skeletal muscles with a characteristic alternation of affected fibers and healthy ones.
There is a violation of the conductive function of nerve fibers and a decrease in muscle contractility. Statistics
1 in 40-50 people is a carrier of the mutant SMN gene. The pathology occurs with a frequency of 1: 6,000 - 10,000 newborns.
How to recognize SMA
Muscle atrophy in children diagnosed with SMA (spinal muscular atrophy) can begin at different times.
The most severe form of muscle atrophy in newborns appears in the first six months of life. The baby is lethargic and sucks poorly. At 3-4 months the child does not roll over on his own and does not attempt to crawl. With spinal muscular atrophy, the baby's posture resembles a “frog”. There is a type of disease that appears after 7-18 months. Muscle atrophy leads to regression of acquired skills in the child. The baby, who was crawling and starting to get up, suddenly becomes inactive. Over time, he stops sitting up straight. With spinal atrophy, reflexes from the upper and lower extremities disappear.
Symptoms of muscle atrophy with spinal muscular atrophy may appear closer to two years of age. Patients have already mastered the skills of standing and walking. At the same time, muscle atrophy confines them to a wheelchair. Intelligence, urination and defecation functions are preserved. SMA after 2 years is the mildest type of the disease.
Muscle atrophy (spinal muscular atrophy) has the following symptoms:
- Appears in infancy or childhood;
- Accompanied by disturbances in walking, running, and standing;
- Tremors and fasciculations (twitching) are detected;
- The “rollback” of motor skills is determined;
- With spinal atrophy, no impairment of intelligence or autonomic functions is detected.
If a child has these signs, he should be consulted with specialists. The diagnosis of SMA is made based on DNA testing.
WERDNIG-HOFFMANN SPINAL AMIOTROPHY
Inherited in an autosomal recessive manner. Underdevelopment of the cells of the anterior horns of the spinal cord, demyelination of the anterior roots, and similar changes in the motor nuclei and roots of the Y, YI, YII, IX, X, XI, XII cranial nerves are detected. In skeletal muscles, neurogenic changes are characterized by “bundle atrophy,” an alternation of atrophied and preserved bundles of muscle fibers.
CLINIC
There are three forms of the disease:
- congenital;
- early childhood;
- late childhood
.
In congenital form
children are born with flaccid paresis. From the first days of life, generalized muscle hypotonia and decreased or absent tendon reflexes are evident. Bulbar disorders are detected early, manifested by sluggish sucking, weak cry, tongue fibrillations, and decreased pharyngeal reflex. The disease is combined with osteoarticular deformities: scoliosis, funnel chest, joint contractures. The development of static and locomotor functions is sharply slowed down. Reduced intelligence. Congenital malformations are often observed: congenital hydrocephalus, cryptorchidism, hemangioma, hip dysplasia, clubfoot, etc.
The course is rapidly progressive and malignant. Death occurs before the age of 9 years. One of the main causes of death are severe somatic disorders (heart and respiratory failure), caused by weakness of the chest muscles and a decrease in its participation in the physiology of breathing.
With early childhood form
The first signs of the disease appear in the second half of life. The disease develops subacutely, often after infection or food intoxication. Flaccid paresis is initially localized in the legs, quickly spreading to the muscles of the trunk and arms. Diffuse muscle atrophy is combined with fasciculations, fibrillations of the tongue, fine tremor of the fingers, and tendon contractures. Muscle tone and tendon reflexes decrease. In the later stages, generalized muscle hypotonia and symptoms of bulbar palsy occur.
The course is malignant, death occurs by 14–15 years of age.
In late form
signs of the disease appear at 1.5 - 2.5 years. The disease begins unnoticed. Movements become awkward and uncertain. Children often trip and fall. The gait changes - they walk with their legs bent at the knees (the gait of a “wind-up doll”). Flaccid paresis is initially localized in the proximal muscle groups of the legs, then relatively slowly moves to the proximal muscle groups of the arms and trunk muscles; muscle atrophy is usually subtle due to the well-developed subcutaneous fat layer. Fasciculations, fibrillations of the tongue, fine tremor of the fingers, bulbar symptoms - fibrillations and atrophy of the tongue, decreased pharyngeal and palatal reflexes are typical. Tendon reflexes fade in the early stages of the disease. Osteoarticular deformities develop parallel to the underlying disease. The most pronounced deformation of the chest.
The course is malignant, but milder. Patients live up to 20 - 30 years.
Diagnostics.
Autosomal recessive type of inheritance, early onset, the presence of diffuse atrophies with predominant localization in the proximal muscle groups, generalized muscle hypotonia, fasciculations, fibrillations of the tongue, absence of pseudohypertrophies, progressive, malignant course, electromyography data and morphology of skeletal muscles, revealing the denervation nature of the changes.
Spinal muscular atrophy (amyotrophy) Werdnig-Hoffmann is a hereditary malignant disease, the onset of development of which occurs from birth to 1-1.5 years. This is one of the most severe forms of muscle atrophy. There is a diffuse increase in muscle atrophy throughout the body. The child loses the ability to sit and move independently, and paresis progresses.
The disease was first described by scientists Werdnig and Goffman. They proved the morphological essence of spinal amyotrophy. But they assumed the existence of only one form of the disease. Later, other scientists Welander and Kueckelberg described another form of spinal muscle atrophy. All variants of the disease have the same genetic nature. Today there are no methods that can completely cure this pathology. Therapeutic measures are aimed at improving the trophism of muscles and nervous tissue.
Disorders with similar symptoms
Symptoms of the following diseases may be similar to those of Werdnig-Hoffmann disease. Comparisons can be useful for differential diagnosis:
- Prader-Willi syndrome is a rare genetic disorder characterized by decreased muscle tone (hypotonia), feeding difficulties, and inability to grow and gain weight (failure to thrive) in infancy; short stature; abnormalities of the genital organs; mental retardation. In addition, between approximately 6 months and 6 years of age, patients may develop excess weight (obesity), especially in the lower parts of the body (eg, lower abdomen, thighs, buttocks). Progressive obesity occurs as a result of insufficient physical activity and excessive food consumption, which can be associated with a lack of satisfaction (fullness) after finishing a meal, obsession with food, unusual eating rituals and eating habits that cause overeating. Patients with Prader-Willi syndrome may also have a characteristic facial appearance due to certain features, including almond-shaped eyes, a thin upper lip, and full cheeks. The diagnosis is made on the basis of chromosomal analysis.
- Pompe disease is an inherited metabolic disorder caused by a complete or partial deficiency of the enzyme alpha-acid glucosidase. This enzyme deficiency causes excess glycogen to accumulate in the lysosomes of many cell types, but predominantly in muscle cells, including cardiac muscle cells. Pompe disease is a single continuum of disease with a variable rate of progression. The infantile form is characterized by severe muscle weakness and abnormally decreased muscle tone (hypotonia) and usually appears during the first few months of life. Additional abnormalities may include enlargement of the heart (cardiomegaly), liver (hepatomegaly), and/or tongue (macroglossia). Progressive heart failure usually causes life-threatening complications between 12 and 18 months of age. The childhood form usually begins in infancy or early childhood. The extent of organ damage may vary between individuals; however, skeletal muscle weakness is usually present with minimal cardiac involvement. Treatment for Pompe disease is available.
- Congenital muscular dystrophy (CMD) is a general term for a group of genetic muscle diseases that occur at birth (congenital) or in early infancy and have similar features on microscopic examination of muscle tissue. Congenital muscular dystrophy is usually characterized by decreased muscle tone (hypotonia); progressive muscle weakness and degeneration (atrophy); abnormally fixed joints, which occur when tissue, such as muscle fibers, thicken and shorten, causing deformities and limiting movement of the affected area (contractures); and delays in achieving basic motor skills such as sitting or standing without assistance. Some forms of AMD may be associated with structural defects of the brain and possibly mental retardation. The severity, specific symptoms, and progression of these disorders vary greatly. Almost all known forms of AMD are inherited in an autosomal recessive manner.
- Congenital myopathies are a group of muscle disorders (myopathies) that are present at birth (congenital). These disorders are characterized by muscle weakness, loss of muscle tone (hypotonia), decreased reflexes, and delay in achieving motor milestones (such as walking). In some diseases, muscle weakness progresses and can lead to life-threatening complications. This group of disorders includes central core disease, central core nemaline myopathy, hyaline body myopathy, central nuclear myopathy, and congenital structural myopathy with muscle fiber type disproportion. Congenital myopathies usually appear in the newborn (neonatal) period, but may appear much later, even in adult life. In most cases, the inheritance of these disorders is either autosomal recessive or autosomal dominant. The diagnosis is made by microscopic examination of muscle tissue.
Additional disorders are included in the differential diagnosis of spinal muscular atrophy, including arthrogryposis multiplex congenita , adrenoleukodystrophy , and myasthenia gravis congenita .
Treatment
The main goal of research aimed at treating spinal muscular amyotrophy is related to increasing the level of SMN protein. Currently, medications are being tested, and official Russian medicine does not use them.
Treatment today includes medications that improve the passage of nerve impulses. Nootropic drugs are prescribed, the main task of which is to improve brain function. Dietary supplements are prescribed to improve metabolism. Vitamin therapy is indicated, in particular, taking B vitamins.
Drugs affecting neuromuscular conduction:
- Alpha lipoic acid
- Acetyl L-carnitine
- Alpha glycerophosphocholine
Vitamins and vitamin complexes:
- Thiamine (B-1)
- Pyridoxine (B-6)
- B-complex
Important treatment methods are massage, physiotherapy, and neuromuscular stimulation. Exercise therapy is prescribed. Physical exercise helps maintain strength, on the other hand, doing it in society, going to the pool helps to socialize and communicate with other people.
Patients with SMA are advised to follow a diet. Food is a source of substances needed by muscles. Thus, the necessary amino acids are found in grains, meat, fish, mushrooms, nuts, and dairy products. Recommended dishes made from oats, wheat and brown rice.
We advise you to study - Consequences of removal of intervertebral hernia
Spinach, broccoli, herring, onions, grapefruit, and watermelon will help to naturally maintain and grow muscles. To increase testosterone, men are recommended to take dill, parsnips, ginseng, and parsley.
Therapeutic measures
In the 21st century, scientists have still not been able to invent a method for fully treating the described disease. In modern medicine, specialists are focused on improving the metabolism of the PNS and muscle areas, which provides an optimal level of inhibition of the spread of symptoms. For such events the following is prescribed:
- Method 1: medicines consisting of pork brain hydrolysate, B vitamin complexes, gamma-aminobutyric acid, etc.
- Method 2: Galantamine and other pharmaceutical drugs aimed at facilitating neuromuscular transmission.
- Method 3: methionine and many agents that have the ability to improve trophism.
- Method 4: medications to increase the level of blood circulation in the body.
In addition to various types of medications, doctors prescribe therapeutic procedures:
- Health-improving gymnastics.
- Massage sessions.
- Orthopedic correction.
For patients with the presented diagnosis and to make the lives of their relatives easier, there are a large number of engineering techniques, for example: wheelchairs, transportable ventilators, etc.
Treatment
A practical patient's guide to the legal basis for the provision of medical care to patients with SMART This guide presents articles and materials on the legal basis for the provision of medical care and drug provision to patients, requirements for the preparation of medical documentation and its forms, and answers to the most frequently asked questions. SMA Families Foundation
Intellect in SMA disease remains completely intact; it develops in the same way as in healthy people. Thus, despite physical limitations, children can live a full life: communicate, play, do physical therapy, and go for walks.
At the moment the disease is incurable. Specialists from different countries are working on drugs to treat SMA, but so far there are no publicly available drugs that can completely cure the disease.
At the end of 2021, the first drug for the treatment of SMA, Spinraza (Nusinersen), appeared in the world. This medicine can slow the progression of the disease, and in some cases improve the condition, but still does not cure the disease completely. At the moment, Spinraza has not yet been registered in Russia - this is a matter for the near future.
In addition, several innovative drugs for the treatment of SMA are currently in development and are at the stage of clinical trials. Detailed and up-to-date information about this can be found on the website of the SMA Families Foundation in the “Research” section.
Nevertheless, we can already do a lot, and with the help of symptomatic therapy and a variety of supportive techniques, slow down the progression of the disease and, in some cases, prevent the development of complications.
Helping organizations
The SMA Families Charitable Foundation is the only organization in Russia that specializes in helping families dealing with spinal muscular atrophy. It provides charitable, informational and psychological support to families, and advises specialists on the disease and methods of working with patients with SMA.
Hospice Assistance Fund "Vera". Charitable and advisory assistance to families with terminally ill children and terminally ill adults.
CSCH No. 1 Department of palliative care for children, Yekaterinburg, Sverdlovsk region. Medical, informational, social and psychological assistance is provided to families raising a disabled child with a palliative condition.
“Research Clinical Institute of Pediatrics named after Academician Yu.E. Veltishchev" FSBEI AT RNRMU named after N.I. Pirogov. The institute is located in Moscow. Residents throughout Russia can seek medical help for children with SMA and other neuromuscular diseases.
Clinic "Chaika". Consultations with pulmonologist Vasily Andreevich Shtabnitsky for children and adults with SMA.
Children's hospice “House with a Lighthouse” (Moscow, near Moscow region). Medical, psychological, legal, social, and charitable assistance to families with terminally ill children and young adults (up to 25 years of age).
Marfo-Mariinsky Medical Center (Moscow). Medical, psychological, legal assistance, nanny assistance, events, spiritual support, charitable assistance to families with terminally ill children.
You will find more detailed information on the website of the SMA Families charity foundation and their special project about life with spinal muscular atrophy
The special project is intended for those who have been diagnosed with SMA and would like to know all the most important things about this disease: which specialists and where to go, how to care, what to watch for, what to remember, what therapy exists today.
To study Bandage for the lumbosacral spine
Diet for spinal amyotrophy
At this time, no diet has been proven to be beneficial for SMA.
According to a large number of parents, a diet that includes a lot of protein or special food additives can increase the strength of the child's muscles. But, despite the obvious need for good nutrition for a sick child, it has not yet been proven that he needs a specific diet. Moreover, some products can even harm his body.
For example, the amino acid menu is sometimes fraught with even greater problems for those children who have too little muscle tissue in their bodies. According to some experts, if there is a lack of muscle tissue, it cannot properly process amino acids and then their level in the blood rises too much.
Doctors have not proven that any diet will improve the condition of a patient with SMA, but proper nutrition can make his life easier.
Some children find it healthier to eat small amounts, more often than three or four times a day. You just need to divide for the patient the entire amount of food taken by a healthy peer of the patient per day into several parts.
Principles of treatment of spinal amyotrophy
Unfortunately, this is an incurable hereditary disease. At the present stage, research is being conducted that may help regulate the synthesis of the SMN protein, but there are no results yet.
The following help alleviate the condition of patients with spinal amyotrophy:
- periodic course intake of drugs that improve the metabolism of nervous tissue and muscles (Cerebrolysin, Cytoflavin, Glutamic acid, ATP, Carnitine chloride, Methionine, Potassium orotate, Tocopherol acetate, etc.);
- B vitamins (Milgamma, Neurovitan, Combilipen);
- anabolic steroids (Retabolil, Nerobol);
- agents that improve neuromuscular conduction (Proserin, Neuromidin, Galantamine, Dibazol);
- massage and physical therapy courses;
- physiotherapy (electrical muscle stimulation, carbon sulfide baths);
- methods of orthopedic correction (with the development of joint contractures and spinal deformities).
Werdnig-Hoffmann spinal amyotrophy, like other forms of this disease, is a pathology that is inherited. The appearance of the disease in a child is explained by the presence of a mutant gene in both the mother and father. The disease is characterized mainly by muscle weakness, which causes immobility and respiratory problems. The disease is currently incurable.
Diagnostics
Manifestations of proximal spinal amyotrophy often resemble the course of other neurological and congenital diseases, as well as traumatic injuries to the structures of the spinal cord and brain. Diagnosis of this disease is especially difficult in newborns and young children.
The key points in diagnosing spinal amyotrophy are the following studies:
- Careful history taking. The presence of cases of spinal amyotrophy in relatives allows us to suspect this hereditary disease.
- Electroneuromyography is a special study of the neuromuscular system. In this case, primary muscle damage is excluded and signs indicating pathology of the motor neurons of the spinal cord are identified.
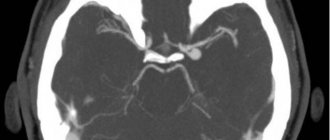
- Computed and magnetic resonance imaging. These methods sometimes make it possible to detect atrophic changes in the anterior horns of the spinal cord. However, more often they are used to exclude other pathologies from the structures of the spinal column and brain.
- Muscle biopsy followed by histological examination of the biopsy sample. Specific muscle changes are revealed, consisting in the alternation of bundled atrophic and unchanged muscle fibers. In addition, compensatory hypertrophied muscle areas can be detected, as well as replacement of muscle tissue with connective tissue.
- Genetic analysis. Allows you to identify the exact cause of the disease: DNA testing reveals a gene mutation on the fifth chromosome.
If there have been cases of the birth of children with spinal amyotrophy in the family, when planning a subsequent pregnancy, the married couple is sent for consultation with a geneticist. Prenatal fetal DNA testing is also mandatory. Detection of Werdnig-Hoffman syndrome at the stage of prenatal diagnosis serves as an indication for termination of pregnancy.
How is this pathology diagnosed?
To make a correct diagnosis, a neurologist must have information about at what age a person first developed symptoms and how quickly they progress. He should also find out neurological data. Moreover, the most important information here is whether the patient has peripheral motor disorders along with complete preservation of sensitivity. It is also important for the neurologist to find out whether the patient has congenital abnormalities or bone deformities. Werdnig-Hoffmann amyotrophy can also be diagnosed by a neonatologist. Using the differential technique you can diagnose:
- myopathy;
- developing Duchenne muscular dystrophy;
- amyotrophic lateral sclerosis;
- syringomyelia;
- polio;
- floppy child syndrome;
- cerebral palsy;
- metabolic pathologies.
To confirm the diagnostic results, electroneuromyography is performed. This is the name of an examination of the neuromuscular system. It allows you to detect the changes necessary to exclude the primary muscular type of the disease, as well as to verify the presence of motor neuron disease. Biochemical blood tests are too small to detect any serious increase in creatine phosphokinase levels, which occurs during the development of muscle dystrophy. By doing an MRI/CT scan of the spine, it is occasionally possible to detect atrophy of the anterior horns of the spinal cord, but using this technique you can make sure that there is no other spinal disease.
A thorough examination is necessary to make a diagnosis.
A definitive diagnosis of Werdnig-Hoffmann amyotrophy is made only when data from a muscle biopsy and DNA analysis are obtained. Using a morphological examination of a muscle biopsy, it is possible to identify pathognomonic fascicular muscle atrophy, interspersed with zones of atrophy of myofibrils and healthy tissue, individual hypertrophied myofibrils, as well as places of connective growths. Mandatory genetic studies include direct and indirect diagnostics. The direct technique makes it possible to identify heterozygous carriage of a gene aberration, and this is necessary for genetic counseling of patients’ relatives, as well as spouses planning to have a child. In all this, quantitative research on the SMA locus genes is important.
By conducting a prenatal genetic examination, you can reduce the risk of giving birth to a baby suffering from Werdnig-Hoffmann amyotrophy. To obtain fetal genetic material, invasive fetal diagnostic techniques should be used:
- amniocentesis;
- chorionic villus biopsy;
- cordocentesis.
Cordocentesis
Having discovered Werdnig-Hoffmann amyotrophy in the fetus, the question of abortion should be raised.
Spinal amyotrophy of Werdnig-Hoffmann - is this disease curable?
Spinal amyotrophy Werdnig-Hoffmann is a hereditary pathology of the nerves that affects the part of them that controls the skeletal muscles. It is characterized by weakness of all muscles in the body at once. More than half of the nerve cells that control muscles are located in the spinal cord.
That is why the disease is called “spinal”. It is also called “muscular” because of the detrimental effect on the muscles: they do not receive any signals from these same nerves. "Atrophy" is a medical term that refers to the wasting or shrinking of something that is not used. Here it concerns inactive muscles.
A person with such a disease has no ability to sit, move, or even take care of himself. There is no cure for this. By conducting prenatal diagnostics, you can prevent the birth of a baby with this disease.
Here we will talk about how this pathology is inherited, what its manifestations are, and also about how you can help a sick person.
We advise you to study - Cervical radiculitis: symptoms
Spinal amyotrophy Werdnig-Hoffmann is named after the two scientists who first described it. In the second half of the 19th century, they proved the morphological essence of the disease. At first, both scientists believed that this pathology had only one form.
But already in the 20th century, scientists Kueckelberg and Welander discovered another clinical form of it, with a genetic cause similar to that discovered by Werdnig and Hoffman. Several clinical forms of spinal amyotrophy are now known.
They are united by a common hereditary defect.
This pathology is hereditary. It is based on a mutation on chromosome 5. The gene that produces the SMN protein is mutated. This protein is necessary for motor neurons to develop exactly as needed.
If the fifth chromosome mutates, it will negatively affect motor neurons, interfering with their development, or even completely destroying them. As a result, the muscle cannot receive control signals from the nerves, and therefore cannot function.
It turns out that not a single movement associated with it is performed.
The mutated gene has an autosomal recessive mode of inheritance. The phrase is deciphered as follows: for the development of spinal amyotrophy, it is necessary that both parents have a mutant gene.
To put it simply, the disease will not develop if at least one of the parents was not a carrier of the mutated gene. At the same time, they themselves do not get sick: people have paired genes, and the healthy gene dominates in the father and mother of the child.
In this case, a sick baby is born in about a quarter of cases. Scientists estimate that about 2% of living people are carriers of a gene with such a mutation.
Classification
Three types of this pathology are known.
- The most severe, manifesting itself earlier than others.
- Medium-heavy.
- The mildest, manifesting itself at a very late age.
According to some doctors, there is another type: moderate/mild SMA, which manifests itself in an adult.
It is worth noting that in addition to Werdnig-Hoffmann spinal amyotrophy, there are other types of SMA, which differ in symptoms and types of inheritance. They are listed in the table below.
| SMAX1 | X-linked recessive | It is observed mainly in the elderly, affects the bulbar nerves of the skull, causing descending paralysis. |
| SMAХ2 | X - clutch. recessive | Congenital aggressive form, leading to death before 3 months. Causes weakness, areflexia, contractures and fractures. |
| SMAX3 | X - clutch. recessive | It mainly affects boys. Atrophy of all distal muscles. Slow increase in symptoms. |
| Distal DCMA1 | Autosomal - recessive | Congenital, mainly affects the hands, and severe respiratory disorders are possible. |
| Distal forms DCMA2 - DCMA5 | Autosomal - recessive | All four forms are characterized by slow progression; DCMA5 is diagnosed in young people. |
| Juvenile SMA (HMN1 type) | Autosomal dominant | Occurs in youth |
| Congenital spinal amyotrophy | Autosomal dominant |
Symptoms of pathology
The congenital type of the disease (SMA I) begins to appear before the baby is six months old. Before this, such a child may move sluggishly. It is not so rare that spinal amyotrophy in a baby can be noticed at the very beginning of the postembryonic period of his life - his deep reflexes fade away:
- The baby's cry is not loud enough;
- it is difficult for him to suck;
- he can't hold his head up.
This pathology can be detected in a baby from the first days of life.
If this becomes noticeable later, which rarely happens, the baby can learn to hold his head, or even sit, but pathology quickly reduces such skills to zero. The following is also typical:
- early speech problems;
- worsening of the pharyngeal reflex;
- fascicular twitching of the tongue.
This type of pathology can be associated with oligophrenia, as well as pathologies of skeletal development:
- deformities of the chest (funnel-shaped/keeled shape);
- curvature of the spine (scoliosis);
- joint contractures.
Other congenital diseases are also common. For example:
- hemangiomas;
- hydrocephalus;
- clubfoot;
- hip dysplasia;
- cryptorchidism.
SMA I is the most “harmful”: it is accompanied by developing paralysis, as well as paresis of the muscles responsible for breathing. Because of the latter, respiratory failure develops, due to which the patient may even die. And impaired swallowing can cause food to enter the respiratory tract and develop aspiration pneumonia. It can also lead to death.
SMA II begins to appear after the baby is six months old. At this age, the baby is already satisfactorily developed, he can stand, hold his head, sit down, and roll over. However, almost never a sick baby does not have time to master walking skills. In most cases, this disease manifests itself after the baby suffers some acute infectious pathology. For example, food poisoning.
When SMA II just begins to manifest itself, the baby develops peripheral paresis in the legs, which then quickly appears in the arms and torso. Diffuse muscle hypotonia appears, deep reflexes begin to disappear. You can also notice the following:
- tendon contractures;
- tremor of fingers;
- fasciculations (involuntary twitching) of the tongue.
Important! Later, bulbar syndrome begins to appear and respiratory failure develops. Due to the slow development of this type of SMA, compared with the congenital form, a sick person usually lives up to fifteen years.
SMA III , also known as Kugelberg-Welander amyotrophy, is the least harmful type of spinal amyotrophy. It begins to appear when the child turns two years old. Sometimes it can be asymptomatic even up to 30 years. However, in this case the patient is no longer a child, which, however, does not make him healthier. With SMA III, the development of the psyche is not delayed; the patient can move for a long time without outside help. He even has a chance to be able to take care of himself in his old age.
SMA IV , also known as the adult form of spinal amyotrophy, is a slowly developing pathology. It usually begins after a person turns 35 years old. This form, if it shortens life, does so only slightly. On the other hand, the patient exhibits the following picture:
- weak proximal muscles;
- fasciculations;
- deterioration of tendon reflexes;
- loss of walking ability.
The third type of pathology can be detected much later - it happens that the disease does not manifest itself for decades
The electromyogram shows the “picket fence rhythm”—spontaneous rhythmic activity. This way you can identify pathology of the anterior spinal horns. If you conduct a morphological study of muscle biopsies, you can notice atro- and hypertrophied fibers of the first and second types. Small round fibers also accumulate, which alternate with hypertrophied fibers - this is “bundle” atrophy. If a pathomorphological study is carried out, swelling/shrinking/atrophy of the motor neurons of the spinal anterior horns becomes noticeable, and quite often also the nuclei of the nerves that exit the brain.
What is SMA?
SMA (spinal muscular atrophy) is a genetic neuromuscular disease that affects the motor neurons of the spinal cord and leads to increasing muscle weakness. The disease is progressive, weakness begins in the muscles of the legs and the whole body and, with the development of the disease, reaches the muscles responsible for swallowing and breathing. At the same time, the intelligence of patients with SMA is absolutely preserved.
Depending on the severity of symptoms, there are 3 main types of proximal SMA: SMA 1, SMA 2, SMA 3. The earlier the first signs of the disease appear, the more pronounced the symptoms, the more severe they are and the faster the disease progresses.
SMA I (WERDNIG-HOFFMAN DISEASE)
The most severe form. Age of manifestation of the disease: up to 6 months.
Description
- Severe muscle hypotonia; "floppy child" syndrome; can't hold his head up; does not achieve the ability to sit and roll over; saggy body when held suspended on the stomach;
- Weakened cough, sucking and swallowing reflexes; choking; respiratory disorders;
- There may be a history of decreased intrauterine activity of the fetus. Deformation of joints and limbs may occur due to intrauterine hypotension.
Flow
- Severe delay in motor development;
- Rapid development of contractures and deformities of the chest;
- Progression of bulbar and respiratory disorders, problems with swallowing food and saliva, sputum discharge;
- High risk of developing aspiration pneumonia;
- Rapid increase in respiratory failure, especially when an infection occurs.
Forecast
- The most severe form: in the absence of respiratory support, most children do not survive beyond 2 years of age;
- Death occurs, as a rule, due to increasing respiratory failure and the development of pneumonia;
- Timely respiratory support can increase a child's life expectancy;
- Such children require palliative care.
SMA II (DUBOVITZ DISEASE)
Age of manifestation of the disease: 6-18 months.
Description
- Delayed motor development;
- The ability to sit without support, sometimes to crawl or stand, but these abilities are reduced as they grow older;
- Finger tremor may occur;
- Muscular and skeletal deformities;
- Breathing disorders.
Flow
- Delayed motor development, its stop and regression;
- Weakness of the intercostal muscles, shallow diaphragmatic breathing, weakening of cough function, and over time the development of respiratory failure;
- Increased risk of complications after a respiratory infection;
- Chest deformities, contractures, scoliosis.
Forecast
Timely care and respiratory support increase life expectancy.
Yulia Samoilova. The most famous person with SMA in Russia. Photo: https://www.instagram.com/jsvok/
SMA III (KUGELBERG-WELANDER DISEASE)
Age of onset of disease: after 18 months
Description
- Ability to walk independently (loses over time);
- Difficulty with complex motor skills (eg, climbing stairs, running);
- As the disease progresses, you may experience difficulty chewing and swallowing, as well as breathing and coughing problems.
Flow
- Progresses slowly;
- By adolescence, most patients use a wheelchair, but some may retain the ability to walk independently into adulthood;
- Over time, pronounced contractures and scoliosis appear;
- Risk of complications after respiratory infection.
Forecast
With proper care they have a normal lifespan.
III type
Kugelberg-Welander disease is a variant of late amyotrophy. With this form of diagnosis, the first signs appear after two years, or in adulthood. Children who already know how to walk suddenly become awkward and complain of pain in their legs when walking. They fall too often, walk unsteadily and practically stop running. Many parents notice changes in gait and sudden clumsiness. At the beginning of the development of pathology, the muscles of the legs are affected, then the muscles of the upper limbs and other parts of the body atrophy. Due to the decrease in muscle volume, weight loss is also observed.
Some patients may experience a period of remission, during which the progression of the diagnosis stops. This period can last from several weeks to several decades.
Impaired respiratory function is the most dangerous manifestation of muscle atrophy.
Mental and mental development disorders are not detected.
Diagnostics
In the early development of the disease, it can be difficult to make an accurate diagnosis, since the symptoms are similar to other diseases. First of all, the child should undergo a consultation with a neurologist. If the baby has a disease at birth, then an approximate diagnosis can be made in the maternity hospital. The specialist conducts an examination and checks for violations of the motor system.
The following studies are being carried out:
Magnetic resonance imaging is ordered to check the spine. It is necessarily used for spinal amyotrophy, because it allows you to understand the state of the area of interest. The procedure is considered safe because it does not worsen a person’s health. Moreover, it is recommended even for children who have Werdnig's amyotrophy. If specialists and parents understand that the minor will not be able to lie still for about an hour, then the question of using anesthesia may arise. In any case, you should not refuse an MRI; it will allow you to learn a lot of useful information about your health status and the development of Werdnig’s amyotrophy.
We advise you to study - Spinal cancer symptoms and manifestationsElectroneuromyogaffy helps to study the state of nerve and muscle endings. This is also required in order to understand how severe the disease is.
If a person has spinal amyotrophy, then it is important to collect as much information as possible about the state of the body. In particular, you will have to undergo this examination.
Genetic diagnostics makes it possible to identify gene mutations. This is relevant for cases where Werdnig's amyotrophy is present. Of course, the examination is not the simplest, and not all clinics can carry it out. Moreover, it is mandatory for those people who are faced with spinal amyotrophy.
Congenital pathology can be detected before the baby is born. Diagnosis is carried out if a girl experiences weak fetal movement. Then the pregnant woman should go to the hospital for a full examination.
Exercise therapy
According to most doctors, comfortable physical activity, unless you go to extremes, is very beneficial for the well-being and health of a patient with SMA.
Joints need to be kept mobile and not put at risk of injury. At the same time, you should maintain range of motion to keep the joints elastic. At the same time, you need to maintain blood circulation. Also, most importantly for children, mobility must be kept high to explore their surroundings.
Important! It is best to conduct classes in a pool filled with water at a temperature of 30-32 degrees Celsius. But, firstly, a person with SMA should not go swimming himself, and secondly, certain safety measures must be observed.
According to some doctors, it is not so necessary to pay a lot of attention to the gradual decrease in the already insufficient number of motor neurons in the body. Research is needed to determine whether this should be taken into account when developing a complex of exercise therapy. The opinions of professionals differ: some believe that it is impossible to overload the body with exercises, while others believe that by doing a gymnastic complex “until you are blue in the face,” you can force the death of the remaining motor neurons. So during exercise therapy you need to be careful and gymnastics must be stopped without bringing yourself to the point of exhaustion.
Occupational and physical therapy programs are useful for people of any age who want to learn how to make the most of their remaining muscle functions and how best to cope with everyday tasks.
Physical activity is very beneficial for patients with SMA
Now you can find devices that are useful even for kids - for exploring the surrounding space. Little children can be helped by everything that human genius has come up with to solve this problem, from walkers to orthoses.
Moreover, there are families who independently invent and make their own devices equipped with special functions. For example, those in which you can change the height so that the child can either crawl on the floor or sit on the table.
A person of any age, if he has SMA, will significantly benefit from devices for solving everyday problems that do not cause difficulties for healthy people.
Fazio-Londe disease
This is a special variant of the manifestation of atrophy. Pathology begins to develop, as a rule, by the age of three, and in some cases in adolescence. The disease is characterized by weakness of the facial muscles, including the masticatory muscles. There is difficulty swallowing and voice changes. The pathology is accompanied by atrophy of the tongue, and in some cases ophthalmoplegia may appear. The disease progresses very quickly. After 6-12 months, death occurs. Paralysis and paresis in the limbs may be added to bulbar disorders. In some cases, these symptoms do not even have time to develop. However, an autopsy always reveals a lesion in the cells of the anterior spinal horns along its entire length.
Causes and factors of the disease
Why does spinal amyotrophy appear? What risk factors can be identified? What is the main cause of the disease? The disease is genetic in nature and is transmitted in an autosomal recessive manner. In this case, both parents must have the defective gene. In this case, spinal atrophy occurs in the child in 25% of cases.
How do genes influence the development of the disease? Spinal amyotrophy occurs when there is a deficiency or complete absence of the SMN protein. It ensures the survival of motor neurons. Its deficiency is the main cause of muscle atrophy in SMA. Brain cells die and there is no signal from them to the muscles.
When the long arm of chromosome 5, on which the SMN 1 gene is located, is deleted, the protein is not produced. Spinal amyotrophy develops.
Risk factors:
- Family history is significant for stillbirths;
- The disease was detected in close relatives;
- Familial infant mortality cases;
- Spinal amyotrophy in an older child.
The likelihood of muscle atrophy occurring in younger children is 1:4.
Causes of the disease
The main cause of spinal amyotrophy of Werdnig Hoffmann is a mutation of the SMN gene (from the English survival motor neuron). The motor neuron survival gene is located on chromosome 5 and is represented by two copies:
- SMNt—telomeric copy, functionally active;
- SMNc is a centromeric copy of the gene, partially active.
The product of this gene is the SMN protein, which is involved in the formation and regeneration of RNA.
Lack of protein causes motor neuron pathologies.
In 95% of cases of Werdnig-Hoffmann disease, there is a deletion (loss) of SMNt, which causes a deficiency of the SMN protein. The SMNc copy only partially compensates for the lack of a telomeric copy.
The copy number of SMNc ranges from 1 to 5. The greater the number of centromeric copies, the more complete the protein is reproduced and the less pronounced the neuron pathology.
In addition to the number of copies of SMNc, the severity of the disease is determined by the length of the deletion site and gene conversions of 3 more genes: NAIP, H4F5, GTF2H2. The involvement of additional modifying factors explains the clinical variability of symptoms.
Types of spinal amyotrophies
Spinal muscular atrophy is one of the most dangerous genetically determined diseases that is found in infants, adolescents, and adults.
It's scary to find out that the baby will never sit, stand, or run. It’s even more scary to see how a normally growing and developing child suddenly begins to slowly fade away, constantly fall, after a few months cannot climb the stairs, and one day loses the ability to simply stand up.
Conventionally, proximal and distal forms of SMA are distinguished. 80% of all types of spinal amyotrophy are of the proximal form.
These include, in addition to Werdnig-Hoffmann disease:
- SMA 3 or Kuldberg-Welander disease - occurs between the ages of 2 and 20, and the pelvic muscles are the first to suffer. There is tremor of the hands and lordosis.
- Lethal X-linked form - described in 1994 by Baumbach, is inherited in a recessive manner, predominantly affecting the muscles of the pelvis and shoulder girdle.
- Infantile degeneration - reflexes of sucking, swallowing, breathing are impaired. Death may occur before the age of 5 months.
- SPA Ryukyu - the linkage gene has not been identified, there is a lack of reflexes, muscle weakness of the limbs after birth.
Distal spinal amyotrophies include progressive Fazio-Londe paralysis, Brown-Vialetta-van Laere disease, SMA with diaphragmatic paralysis, epilepsy and oculomotor disorders.
Clinical picture
The symptoms of SMA 1 and SMA 2 are very different. Manifestations of SMA 1 are often detected during pregnancy, since the fetus in the womb is inactive and moves very rarely. After birth, the child experiences respiratory failure, often he cannot breathe on his own, and other innate reflexes are absent. The main manifestations of the disease can be considered:
- Decreased muscle tone.
- Retarded physical development.
- Inability to hold the head upright.
- Cannot independently roll over onto its side, stomach or back.
- Mild paralysis of the limbs.
- Lack of swallowing reflexes.
- Lack of sucking reflex.
The child takes a characteristic position in which he is almost constantly. In most cases, paralysis of the diaphragm may also occur. All this over time leads to disruption of skeletal development, scoliosis appears, the presence of a hump is often noted, and the shape of the chest changes. Only 12% of such children live to be 5 years old.