Home → Information about diseases → Hydrocephalus (hypertensive-hydrocephalic syndrome of HHS)
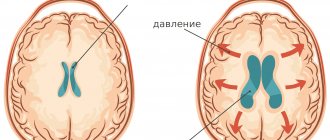
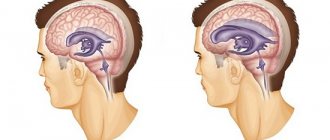
Absolutely all people have a small amount of fluid in the cranial cavity that washes the brain. This liquid is called “liquor”. Liquor is constantly produced and absorbed (renewed). If a person produces more cerebrospinal fluid than is absorbed, it begins to accumulate in the cranial cavity, and intracranial pressure increases. Excess fluid begins to put pressure on the brain, causing various disruptions to its functioning. This is called hydrocephalus (increased intracranial pressure, hypertensive-hydrocephalic syndrome or “dropsy of the brain”).
What is Hypertension-hydrocephalic syndrome (HHS)?
Hypertensive-hydrocephalic syndrome (HHS) is caused by excessive accumulation of cerebrospinal fluid (CSF) in the ventricles of the brain and under the meninges, resulting from obstruction of outflow, excessive formation and impaired reabsorption of cerebrospinal fluid. This is one of the most common syndromic diagnoses in pediatric neurology, especially in young children with perinatal encephalopathy (PEP). It should be noted that the term “hypertensive-hydrocephalic syndrome” is a concept used exclusively in Russia. The causes of HGS can be: unfavorable course of pregnancy and childbirth, hypoxic-ischemic brain damage, deep prematurity, intracranial hemorrhage and intrauterine infections, congenital malformations of the brain, neuroinfections. Research methods to judge the level of cerebrospinal fluid pressure are very limited. Currently, the only reliable and relatively accessible of them is to perform a lumbar puncture of cerebrospinal fluid (CSF) to measure CSF pressure, which is a diagnostic criterion for this pathology. HGS can be either one of the manifestations of hydrocephalus or many other neurological diseases. The diagnostic criteria for HGS include clinical symptoms that indirectly indicate an increase in cerebrospinal fluid pressure and dilation of the ventricles of the brain.
What is the prevalence of hydrocephalus? According to official statistics, up to 70% of newly born children suffer from an obvious (hydrocephalus) or latent form (hypertensive-hydrocephalic syndrome) of this disease.
What is the reason for the widespread incidence of hydrocephalus?
- Weakness of the nervous system of children born from parents who grew up in environmentally unfavorable conditions.
- A large number of “saved” premature babies.
- Frequent use of surgical delivery, which also contributes to the development of hydrocephalus.
- A busy schedule of vaccinations up to 1 year of age contributes to the exacerbation of latent hypertensive-hydrocephalic syndrome.
Early diagnosis (ultrasound, electropuncture) also helps to identify hidden forms of the disease hydrocephalus of the brain. There are many more reasons that can be found. But the fact remains: it is necessary to identify and treat hydrocephalus without waiting for exacerbations of the disease and complications.
What are the manifestations of hydrocephalus? In children under 1 year of age: increased excitability, “unreasonable” crying, sleep disturbance, frequent regurgitation, throwing the head back in sleep, increased muscle tone (hands held in fists, legs resting on toes and crossed), weak support with legs, lack of step reflex, delayed motor and mental development. In preschool children: hypermobility, aggressiveness, hysterical manifestations, stuttering, enuresis, strabismus, frequent colds, delayed psycho-speech development (poor vocabulary, impaired diction, difficulty constructing complex sentences). In schoolchildren: nosebleeds and headaches, memory and concentration are reduced, disinhibition and neuroticism are noted, learning school material is difficult: they complete tasks slowly, make a large number of mistakes, their hands get tired quickly, their handwriting is not even, they read slowly and poorly assimilate the material they read, find it difficult to write a competent story.
What are the worst complications of hydrocephalus? CONVISIONS, CEREBRAL PALSY, MORTONITY.
What factors cause exacerbation of hydrocephalus? Any stress on the body (viral infections, stress, mental and physical fatigue, concussion, vaccinations) can lead to an exacerbation of increased intracranial pressure - especially a combination of these. For example: studying at the gymnasium + flu + stress can lead to exacerbation of hydrocephalus, headaches and a decrease in academic performance and aggressiveness.
What to do if your child has any manifestations of hydrocephalus? Promptly seek advice from the children's department of neurology and reflexology at Reatsentr to clarify whether the child needs to be examined and treated.
Medical Internet conferences
Primary pulmonary hypertension (PPH) - Ayersa's disease - is a rare, severe, progressive disease of unknown etiology and is characterized by a poor prognosis [1, 2]. Pulmonary arterial hypertension (PAH) is diagnosed when the mean pressure in the pulmonary artery increases to or more than 25 mmHg. Art. at rest and 30 mm Hg. Art. under load [3].
According to the literature, the incidence of idiopathic pulmonary hypertension is 1–1.7 cases per million people [2], and the disease is almost 2 times more common in women than in men. The average age of patients with this diagnosis is 36.4 years [1]. Survival statistics for patients with PLH are not reassuring - in the absence of intensive treatment, the average life expectancy is about 3 years from the moment of diagnosis [2].
Despite the active study of the problem, the etiology of PLH remains unclear, but researchers suggest an important role of genetic disorders in the development of the disease [4]. In particular, the development of PLH is associated with a mutation of the BMPR2 gene, localized on the second chromosome, but the pathogenetic relationship between this disorder and PLH has not been discovered [11].
Despite the fact that the factors leading to the triggering of pathological changes in the pulmonary vessels have not been precisely established, today researchers consider the theory of endothelial dysfunction (ED) to be the main one in the etiology and pathogenesis of this disease, which indicates that damage and dysfunction of the endothelium of the pulmonary vessels leads to the development of vasoconstriction and remodeling of the vascular bed. In pathogenesis, four main pathophysiological phenomena are distinguished: vasoconstriction, reduction of the pulmonary vascular bed, decreased elasticity of the pulmonary vessels, their obliteration due to thrombosis and proliferation of smooth muscle cells (SMCs). These processes are induced by an imbalance in the production of vasoactive mediators that occurs during ED, which consists of increased synthesis of vasoconstrictor substances (thromboxane A2, endothelin-1) by endothelial cells and a deficiency in the production of vasodilating substances (NO, prostacyclin). Disruption of the voltage-gated potassium channels of SMCs also plays a role, which causes vasoconstriction and proliferation of SMCs due to increased intracellular calcium ion content. A key role in the development and progression of PAH is played by NO deficiency, which promotes chronic vasospasm, cell proliferation, and intravascular thrombus formation [5].
Thus, a vicious circle is closed - progressive damage to the endothelium leads to vascular remodeling [11].
Pathological processes in PAH affect all layers of the vascular wall, various types of cells (endothelial, SMC, fibroblasts). Structural disorders begin with muscular arteries and pulmonary arterioles. The process begins with hypertrophy and muscularization of the medial tunic of arterioles. In addition, migration of SMCs into the intima of the vessel is observed, in which active proliferation of cellular elements occurs. Initially, intimal thickening is reversible, but soon irreversible changes develop - fibrosis and fibroelastosis. In some cases, concentric intimal fibrosis completely closes the lumen of the vessel. In this case, plexogenic and pleximorphic structures can be determined, which, as a rule, arise proximal to the site of obstruction. The adventitia exhibits increased production of extracellular matrix, including collagen, elastin, fibronectin, and tenascin. The secretion of mediators with a pronounced vasoconstrictor effect transforms the state of the vascular bed from the usual anticoagulant to procoagulant and contributes to the development of thrombosis [10, 11].
Modern functional studies using various non-invasive methods for assessing the state of peripheral blood flow do not confirm the generalization of endothelial dysfunction in patients with PLH, however, an increased constrictor ability of the SMC is noted [6].
An increase in vascular resistance in the pulmonary circulation (PCC) initiates the occurrence of myocardial hyperdynamia syndrome with the development of right ventricular (RV) hypertrophy. This phenomenon is due to the physiological response described by Starling, which consists of an increase in the force of cardiac contraction in response to load by volume or vascular output resistance [7]. Cor pulmonale (CH) develops with primary or secondary PAH resulting from dysfunction of pulmonary vascular endothelial cells and structural and functional changes in the pulmonary vessels [8]. There are several stages in the development of the pulmonary heart. In the initial stage, there is an increase in pulmonary vascular resistance, which is a consequence of PAH. In the second stage, changes in the pancreas are detected in response to an increase in pulmonary arterial pressure. The third stage consists of pronounced hypertrophy and dilatation of the RV, changes occur in the vascularization of the latter, and right ventricular heart failure (RVHF) may be observed [9].
During the formation of LS, changes in the myocardium are observed in the form of hypertrophy, dystrophy, atrophy and necrosis of pancreatic cardiomyocytes. Atrophic-sclerotic processes can be observed in the muscle fibers of the pancreas, and pronounced endocardial fibroelastosis can be observed in the right atrium and pancreas. Less common is dilatation of the left ventricular cavity [12].
Diagnosis of PLH is difficult because patient complaints are nonspecific and may resemble congenital heart disease. In most cases, clinical manifestations develop after the development of irreversible changes in the lungs. Weakness, fatigue, shortness of breath, hemoptysis, anginal pain in the heart area, dizziness, and abdominal discomfort are noted. Upon examination, pulsation of the neck veins, hepatomegaly, peripheral edema, and ascites are detected. Palpation is determined by pulsation in the fourth intercostal space to the left of the sternum, enlargement of the right ventricle. An increase in the second tone in the second intercostal space on the right is auscultated [13].
Conservative treatment of PLH involves, first of all, the prescription of calcium antagonists, anticoagulant therapy, and the use of diuretics for PHF. Sildenafil citrate (the active ingredient of Viagra) has the same vasodilating abilities in both the vessels of the genitals and the lungs, and therefore was approved in the USA as a drug for the treatment of PLH [4]. Surgical treatment is also possible - transplantation of the heart-lung organ complex [11]. However, complete elimination of PLH is currently not possible; treatment is supportive.
Persistent pulmonary hypertension of newborns (PPHN) is included in a separate category due to the presence of characteristic pathogenetic and clinical and morphological aspects associated with the characteristics of the fetal blood circulation and distinguishing it from PHH. PPHN is a disease characterized by abnormally increased pressure in the pulmonary vessels and, as a consequence, right-to-left shunting of blood through the foramen ovale and (or) patent ductus arteriosus in the absence of other heart defects. Among the variants of PPHN, in turn, there are idiopathic (primary) and complicating various neonatal cardiopulmonary complications (secondary) [14]. PPHN occurs in 0.2-0.3 cases per 1000 newborns, but the idiopathic variant accounts for up to 20% of all cases of PPHN [15].
The leading etiology of idiopathic PPHN is prolonged intrauterine hypoxia, which leads to vascular remodeling, which is expressed in vascular smooth muscle hyperplasia, spreading to intralobular arteries, which leads to increased vascular resistance [15].
In healthy newborns, the activity of vasoactive substances changes in response to numerous stimulations that occur during birth, including increases in partial pressure of oxygen and changes in blood pH [14]. The main pathogenetic link of idiopathic PPHN is also considered to be an imbalance in the synthesis of vasoconstrictor and vasodilating substances [15].
Thus, primary pulmonary hypertension is a rare and severe disease with an extremely poor prognosis. However, the accumulated clinical experience provides opportunities to discover the mechanisms of its pathogenesis and develop new diagnostic and treatment methods that can not only prolong the life of patients, but also improve its quality. In this regard, relevant .
Clinical case
From the anamnesis it is known that the boy E.D. was born from the fifth pregnancy (second birth), occurring against the background of the threat of miscarriage, edema of pregnant women, low placentation, partial progressive abruption of the low-lying placenta, a burdened obstetric and gynecological history, chronic intrauterine fetal hypoxia. Preterm birth at 32–33 weeks gestation was resolved by emergency cesarean section.
The newborn was in serious condition with an Apgar score of 4-5-6-6 points. The severity of the condition was due to respiratory disorders, neurological symptoms due to prematurity and morphofunctional immaturity. Anthropometric data of the child at birth: body weight 2530 g, height 47 cm, chest circumference 31 cm, head circumference 33 cm.
From birth he was on a ventilator. At the maternity hospital stage, respiratory, infusion, antibacterial and hemostatic therapy was carried out. For the purpose of further examination, treatment and nursing, the boy was transferred by an air ambulance team from the maternity hospital to the neonatal intensive care unit of the Saratov Regional Children's Clinical Hospital (SODKB).
Based on the examinations performed, the main competing clinical diagnosis was made: 1. Congenital pneumonia. 2. Cerebral ischemia grade 3, acute period. Oppression syndrome. Complications: multiple organ failure syndrome (cerebral edema, stage 3 coma; stage 3 respiratory failure; stage 3 acute cardiovascular failure; acute renal failure in the stage of oligoanuria; edema syndrome; hemorrhagic syndrome; pulmonary hypertension). Concomitant diseases: perimembranous subtricuspid interventricular septal defect 0.24 cm; patent ductus arteriosus: 0.30cm; open functioning foramen ovale: 0.42 cm, left-right reset. Background diagnosis: neonatal respiratory distress syndrome; prematurity 32-33 weeks.
Under the conditions of the therapy (inotropic support, surfactants, increasing ventilation parameters to the maximum possible), the child’s condition remained severe with deterioration dynamics. Against the background of progressive multiple organ failure, asystole was noted, and the biological death of the child was stated.
When opening the chest cavity, the usual arrangement of organs was noted, but the lungs completely filled the pleural cavity. The shape of the heart is cone-shaped, the location is normal. The size and location of the thymus gland are unremarkable. In the soft tissues there are bright red hemorrhages measuring up to 1 cm.
When examining the respiratory tract, swollen pink palatine tonsils of normal size were noted. A small amount of mucous content is detected in the lumen of the larynx, trachea and bronchi. The mucous membrane of these organs is edematous, smooth along its entire length. The leaves of the parietal and visceral pleura are smooth, pale pink. The lungs are dark red in color, dense in consistency, the lung tissue is homogeneous when cut, abundantly saturated with blood; when pressed, liquid blood and edematous fluid are released. The weight of the left lung is 40 grams, the right lung is 37 grams. Pieces cut from the lungs sink when immersed in water. Histological examination of the lungs revealed focal accumulations of erythrocytes and forming hyaline membranes in the lumens of the alveoli; in the vessels, hypertrophy of the muscular layer of arteries and veins was noted by more than 25%, intimal proliferation with fibrosis, as well as thrombotic masses were detected.
An examination of the circulatory system revealed a small amount of yellowish transparent fluid in the cardiac membrane. The pericardial leaves are smooth and shiny. Heart weighing 20 g. Myocardium pink-red, elastic consistency. The valvular and parietal endocardium throughout is thin, translucent, shiny, with a grayish tint. The thickness of the myocardium of the left ventricle is 0.7 cm, the right one is 0.3 cm (normal is 0.2 cm). The perimeter of the pulmonary trunk above the valves is 2.2 cm, of the aorta - 1.9 cm. The intima of the aorta is smooth, shiny, reddish-yellow. There is dark liquid blood in the cavities of the heart and in large vessels. The heart valves are developed correctly and not altered. Interventricular communication measuring 0.2 cm; the oval window measuring about 0.3 cm is open; open arterial duct measuring 0.3 cm. Histological examination revealed dystrophy and hypertrophy of cardiomyocytes.
When opening the cranial cavity, it was discovered that the dura mater was thin, with a pearlescent sheen. The soft meninges are swollen and full of blood. The convolutions of the brain are flattened, the furrows are smoothed. The lateral ventricles are slightly increased in size and contain clear, bright yellow cerebrospinal fluid. In the cavity of the right ventricle there is a small blood clot of bright red color with a volume of about 5 ml. The choroid plexuses are full-blooded, with transparent contents. The white and gray matter of the cerebral hemispheres are distinguishable; dark red dots are identified on the surface of the sections, easily washed off with water. The rest of the brain structures are without visible changes. Brain weight 265 grams. Histological examination revealed uneven blood supply to the cerebral vessels.
When the abdominal cavity was opened, about 5 ml of yellow liquid was released. The loops of the small intestine in the lower parts are dark red in color and slightly increased in size; the intestinal vessels are full of blood. The mucous membrane of the small intestine has a smoothed pattern, dark red in color. There is hemorrhagic content in the lumen of the lower parts of the small intestine. The liver, weighing 105 grams, is red in color and has a normal structure on the surface and in the cut. Histological examination of the liver revealed degeneration of hepatocytes and congestion of the hepatic sinuses.
When opening the kidneys, it was noted that on the section the cortical substance was bluish-red in color, and the medulla was dark red; parenchyma of dense consistency; The mucous membrane of the pelvis is smooth, clean with isolated small hemorrhages. The mucous membrane of the ureters and bladder is without features. Histological examination of the kidneys revealed dystrophy of the epithelium of the convoluted renal tubules, as well as uneven blood supply to the vessels.
During the autopsy of the remaining organs and systems, no significant features were identified.
Based on the autopsy and histological examination, a pathological diagnosis was made - primary pulmonary hypertension; complications of the underlying disease – myocardial hypertrophy of the right ventricle of the heart; secondary hyaline membranes; hemorrhages in the lungs; parenchymal dystrophy of internal organs.
Discussion
In this case, PPH in a newborn was combined with a patent foramen ovale and patent ductus arteriosus, as well as a perimembranous ventricular septal defect, which led to significant changes in hemodynamics in the neonatal period. The consequence of prolonged hypoxia was ischemic damage to various organs, the development of parenchymal degeneration and multiple organ failure, which determined the severity of the patient’s condition. The immediate cause of death of the patient was respiratory failure.
Conclusion
Thus, PPH, a severe progressive disease that is difficult to treat, is complicated in newborns by hemodynamic features and inevitably leads to death. Studying the etiology and pathogenetic mechanisms of idiopathic pulmonary hypertension will allow us to find new ways to help patients suffering from this disease.
Treatment methods for hydrocephalus
The surgical method of treating hydrocephalus is used only in extreme cases (decompensated forms of internal hydrocephalus), excess fluid is drained from the cranial cavity into the abdominal cavity using a tube (shunt), this operation, like any other, is quite traumatic; in the future, several more surgical operations may be required interventions to replace and check the operation of the shunt.
A medicinal method of treating hydrocephalus - the use of diuretics, such as Diacarb, is often used by neurologists in outpatient practice. Diakarb removes fluid not only from the cranial cavity, but also from the body as a whole, at the same time a loss of microelements occurs, the effect of this treatment method is temporary, after its cessation, the fluid begins to accumulate again and intracranial pressure increases.
Herbal medicine - the use of diuretic herbs (horsetail, fennel, lingonberry leaf), does not cause addiction and loss of microelements. It is used, as a rule, for preventive purposes: to avoid exacerbation of hydrocephalus during colds, when changing climatic zones, in the autumn-spring period with pronounced changes in weather conditions.
Massage is an effective method for children with motor impairments (increased muscle tone, delayed motor development), and is mainly aimed at relaxing tense muscles. It is advisable to use only in complex treatment, since massage does not affect the main cause of the disease - hydrocephalus and hypoxia of the cerebral cortex.
MICROCURRENT REFLEXOTHERAPY - the method is effective in children with various manifestations of hydrocephalus, it allows you to eliminate not only external manifestations (hysterics, developmental delays, etc.), but also treat hydrocephalus itself, that is, it has a complex therapeutic effect on the body. The effect of treatment is stable and does not stop after the end of treatment.