Serotonin syndrome (serotonin intoxication) is a rare but potentially fatal reaction of the body to taking medications or drugs that increase serotonergic transmission. It can occur as a result of poisonings, medications (most commonly with antidepressants), an adverse reaction to a combination of medications or drugs, or the recreational use of certain drugs. It often occurs when two or more drugs are used - for example, the combination of SSRI and MAOI antidepressants leads, according to some data, to serotonin syndrome in almost half of patients.
Clinical picture
The clinical manifestations of serotonin syndrome include symptoms of three groups: mental, autonomic and neuromuscular disorders.
Changes in mental status: agitation, anxiety, delirium, euphoria, mania, hallucinations, confusion, mutism, coma.
Symptoms of autonomic dysfunction: abdominal pain, diarrhea, hyperthermia (from 37-38 ° C to 42 ° C and above), headaches, lacrimation, dilated pupils, nausea, tachycardia, tachypnea, fluctuations in blood pressure, chills, increased sweating.
Neuromuscular disorders: akathisia, bilateral Babinski's sign, epileptiform seizures, hyperreflexia, incoordination, myoclonus, horizontal and vertical nystagmus, oculogyric crises, opisthotonus, paresthesia, muscle rigidity, tremor.
At the initial stage, serotonin syndrome manifests itself mainly from the gastrointestinal nervous system: dyspeptic symptoms are characteristic (seething, abdominal cramps, flatulence, loose stools, nausea, less often vomiting, etc.); extrapyramidal disorders (tremor, dysarthria, restlessness, muscle hypertonicity), hyperreflexia, myoclonic twitching, usually starting in the feet and spreading throughout the body.
As the condition worsens, a patient with serotonin syndrome develops a manic-like state, manifested by racing thoughts, accelerated slurred speech, sleep disturbances, hyperactivity, and less commonly, confusion and symptoms of disorientation. At its last stage, with an extremely rarely observed malignant variant of the course (possible with a combination of SSRIs and MAOIs), serotonin syndrome is close to the clinical picture of neuroleptic malignant syndrome: a sharp increase in temperature, profuse sweating, a mask-like face, greasiness of the face, as well as acute cardiovascular disorders which can be fatal.
Dangerous complications of serotonin syndrome also include disseminated intravascular coagulation syndrome, rhabdomyolysis, myoglobinuria, renal, hepatic and multiorgan failure, metabolic acidosis, leukopenia, thrombocytopenia, and tonic-clonic convulsions. Myoclonus affecting the pectoral muscles can also lead to death due to asphyxia or hypoxia.
Severity
Serotonin intoxication can occur in mild, moderate and severe forms. In mild forms of the disease, slight tachycardia, sweating, increased nervous excitability, anxiety, and dilated pupils are noted. The temperature does not rise.
Moderate severity is accompanied by disturbances in heart rhythm, the appearance of severe tachycardia, abdominal pain, tremors of the extremities, rolling of the eyeballs, hyperreflexia, and increased body temperature.
The severe form of serotonin syndrome is accompanied by the development of complications and poses a threat to the patient’s life.
Pathophysiology
Serotonin syndrome is based on excessive activity of central serotonergic structures: predominantly postsynaptic 5-HT1A receptors, but its development is also facilitated by stimulation of 5-HT2 receptors due to the accumulation of serotonin in the synapse. There is also evidence that hyperactivation of noradrenergic structures may also play a critical role in the occurrence of serotonin syndrome. The role of other neurotransmitters is significantly less: glutamate and GABA; The influence of dopaminergic structures on the pathogenesis of serotonin syndrome is also detected, due to pharmacodynamic interactions, direct interaction between serotonergic and dopaminergic structures, or in connection with other mechanisms.
Serotonin syndrome: description
Serotonin syndrome is a collection of various symptoms caused by excess of the neurotransmitter serotonin in the central nervous system. This condition is also called serotonergic syndrome or central serotonin syndrome.
Excess serotonin is caused by anti-depression medications (antidepressants), which affect the body's serotonergic system.
What is serotonin?
Serotonin (chemically: 5-hydroxy-tryptamine) is an important substance in the nervous system (neurotransmitter). It is found in both the central (brain and spinal cord) and peripheral nervous systems. In the central nervous system (CNS), serotonin is involved in the control of the sleep-wake cycle, emotions, temperature and pain, as well as learning and memory formation.
For example, serotonin stimulates gastrointestinal movements and dilates blood vessels in the skin and skeletal muscles, but constricts them in the heart. Serotonin is also involved in blood clotting (promotes platelet aggregation).
Depression – serotonin deficiency
Serotonin, along with other neurotransmitters, controls several processes in the brain. These include, first of all, emotional processes, attention control and pain suppression.
Experts believe that deficiency of these substances leads to depressive symptoms such as sadness, lethargy, and loss of interest. Therefore, doctors treat depression with drugs that increase serotonin levels in the body. As a result, for example, too high a dose of medication can lead to excess serotonin and ultimately serotonin syndrome.
Prevalence
In 2002, the US Toxicity Screening System compiled data on 26,733 SSRI prescriptions, which resulted in serious toxic effects in 7,349 people, including 93 deaths. Finding out exact epidemiological data on the prevalence of serotonin syndrome is difficult due to the fact that about 85% of doctors are unfamiliar with this pathology and therefore rarely make this diagnosis.
Serotonin syndrome often occurs in elderly patients, children and even infants. It has also been found that it occurs in 14-16% of people with an SSRI overdose.
Etiology
The widespread use of modern antidepressants throughout the world is easily explained by the increase in depressive conditions and the absence of side effects characteristic of other drugs in this group. These medications are easy to purchase and, if necessary, taken in combination with other medications without a doctor's prescription. The human body reacts in a special way to an unfavorable combination of medications. Serotonin intoxication has a negative impact on a person’s overall well-being. Often such patients experience disturbances in the functioning of internal organs and systems. In the absence of medical care, they die.
The modern pharmacological industry is trying every year to improve psychotropic drugs, which include antidepressants. The latest generation of drugs should have a positive effect on the functioning of the serotonergic system and increase the secretion of serotonin during the transmission of nerve impulses. When the amount of transmitter in neurons becomes insufficient, patients develop depressive syndrome.
Drug addiction is the scourge of modern life. Drugs are another cause of serotonin toxicity. Drugs increase the retention of the transmitter in the synaptic cleft, promote its accumulation in the intermembrane space and stimulate serotonin receptors.
Etiopathogenetic factors of serotonin intoxication syndrome:
- unacceptable combination of pharmacological drugs,
- abrupt replacement of one antidepressant with another,
- drinking alcohol during treatment with antidepressants,
- overdose of antidepressants and severe drug intoxication.
It is prohibited to use opioid analgesics, antibacterial agents, antitussive drugs, antiemetic drugs, antipsychotics, anticonvulsants, thyroid hormones, weight loss drugs, lithium-containing drugs, and antiparkinsonian drugs with antidepressants.
Diagnostics
There are no specific laboratory tests, the data of which could be used in the diagnosis of serotonin syndrome; laboratory tests are important only for diagnosing complications (metabolic acidosis, disseminated intravascular coagulation syndrome, rhabdomyolysis) and monitoring the patient. Determining the concentrations of serotonergic drugs in the blood plasma does not play a significant role, since in most cases of serotonin syndrome they do not exceed the permissible level, and their presence in toxic concentrations is not a prerequisite for its development.
Sternbach proposed the following criteria for diagnosing serotonin syndrome:
- At least 3 of the following symptoms are associated with the initiation of therapy with a serotonergic drug, or an increase in its dose, or the addition of another serotonergic drug: agitation, hyperreflexia, diarrhea, increased sweating, mental status changes (confusion, hypomania), fever, myoclonus, disturbances coordination, tremendous chills, tremors.
- Other possible causes have been excluded - infections, metabolic disorders, drug intoxication, withdrawal syndrome, etc.
- Immediately before the onset of symptoms, the patient was not prescribed an antipsychotic drug or, if previously prescribed, its dose was not increased.
Differential diagnosis
Differential diagnosis of serotonin syndrome must be carried out with such conditions as neuroleptic malignant syndrome, malignant hyperthermia, febrile schizophrenia, anticholinergic delirium, acute psychosis, somatic symptoms of depression, heat stroke, meningitis, encephalitis, hyperthyroidism, hypertensive crisis, septicemia, “rigid man” syndrome , tetanus, various intoxications (anticholinergics, amphetamines, lithium, LSD, cocaine, MAOIs, phencyclidine, salicylates, strychnine, sympathomimetics).
Pathogenesis
Serotonin is a biologically active substance that causes the nervous system to work smoothly. By activating one nerve cell, the neurotransmitter penetrates the intermembrane space and attaches to another. This results in consistent stimulation of the entire nervous system, ensuring its functional integrity. With this pathology, the “happiness hormone” is produced in excess.
Neurons of the brain stem are responsible for the functioning of the muscles of the eye and eyelid, masticatory muscles, swallowing and sneezing reflexes, touch, hearing and smell, digestion, sleep, libido, pain sensitivity, and emotional background. With excessive biosynthesis of serotonin, this syndrome develops. Patients experience insomnia, the functions of internal organs and the strength of muscle contractions are impaired.
Taking serotonergic drugs stimulates the biosynthesis of the neurotransmitter, disrupts its reuptake, activates serotonin receptors, and blocks enzymes that break down serotonin. An excess of this substance in the synaptic cleft leads to the development of the syndrome. The disruption of all processes regulated by serotonin is manifested by characteristic clinical symptoms.
Causes and prevention
The main principle of prevention: limit the use of serotonergic drugs in combination therapy and carefully monitor the patient's condition during its use. It is also necessary to monitor the patient's condition during periods when a new drug is included in the regimen or the dose is increased. In particular, the combination of MAOIs and SSRIs, MAOIs and clomipramine should be avoided. One of the principles of prevention is also compliance with the recommended dosages and regimen of taking antidepressants.
A break of at least two weeks is required:
- in the interval between the abolition of fluoxetine (Prozac) and the appointment of an SSRI;
- between discontinuation of SSRIs and administration of other serotonergic agents;
- between discontinuation of SSRIs and administration of MAOIs.
An interval of at least five weeks is required between the discontinuation of fluoxetine and the appointment of an irreversible MAOI, for elderly patients - at least eight.
When transferring from irreversible MAOIs to SSRIs, a break of four weeks should be maintained (according to other sources - two weeks); When switching from moclobemide to SSRIs, 24 hours is sufficient.
After treatment with clomipramine, you must wait three weeks before prescribing other serotonergic drugs.
The duration of the withdrawal period depends on the length of the half-lives of the drugs. The withdrawal period is at least five half-lives, but this is the minimum recommended withdrawal period. The long half-life of fluoxetine and its main active metabolite, norfluoxetine, may pose significant challenges to clinical use.
In addition, serotonin syndrome has been observed:
- when taking SSRIs or MAOIs together with cold medications containing dextromethorphan, which can inhibit serotonin reuptake, SSRIs or MAOIs with meperidine, tramadol, with nefazodone, with herbal antidepressant drugs containing St. John's wort, with 5-hydroxytryptophan and tryptophan;
- co-administration of SSRIs with opioid analgesics, S-adenosylmethionine (SAM, heptral), metoclopramide, trazodone, clomipramine, amitriptyline, buspirone, anti-migraine drugs, levodopa;
- combined use of MAOIs with cyclic antidepressants, venlafaxine, specific serotonergic antidepressants, methylenedioxymethamphetamine (MDMA, “ecstasy”);
- combined use of the following antidepressants: imipramine and moclobemide, trazodone and fluoxetine, trazodone and buspirone, venlafaxine and tranylcypromine, venlafaxine and phenelzine, fluoxetine and selegiline (at high doses of selegiline - over 10 mg/day);
- combined use of an antidepressant and mood stabilizer: SSRI and carbamazepine, SSRI and lithium, MAOI and lithium;
- co-administration of SSRIs and drugs that affect the metabolism of SSRIs (inhibiting CYP2D6 and CYP3A4 isoforms of cytochrome P450);
- co-administration of tramadol and antidepressants of many groups (including SSRIs).
There are isolated reports of the occurrence of serotonin syndrome during monotherapy with SSRIs (at the beginning of treatment, with a sharp increase in dosage, or during intoxication), as well as during monotherapy with clomipramine or trazodone.
Serotonin syndrome is also possible when taking opioid analgesics, cough suppressants, antibiotics, weight loss drugs, antiemetics, migraine drugs, etc.
Literature
- Dopamine diseases;
- Mood mediator receptor;
- Fusar-Poli P., Allen P., McGuire Ph., Placentino A., Cortesi M., Perez J. (2006). Neuroimaging and electrophysiological studies of the effects of acute tryptophan depletion: a systematic review of the literature. Psychopharmacology. 188, 131–143;
- Steenbergen L., Sellaro R., Colzato L. S. (2014). Tryptophan promotes charitable donation. Front. Psychol. doi: 10.3389/fpsyg.2014.01451;
- Van Erp A. M. M. and Miczek K. A. (2000). Aggressive behavior, increased accumbal dopamine, and decreased cortical serotonin in rats. J. Neurosci. 20, 9320–9325;
- Vicario C. M. (2014). Aggression traits in youth psychopathy: the key role of serotonin. Front. Psychiatry. 5, 25;
- Puig M V and Gulledge A T (2011). Serotonin and prefrontal cortex function: neurons, networks, and circuits. Mol. Neurobiol. 44, 449–464;
- Caspi A., Hariri A.R., Holmes A., Uher R., Moffitt T.E. (2010). Genetic sensitivity to the environment: The case of the serotonin transporter gene and its implications for studying complex diseases and traits. Am. J. Psychiatry. 167, 509–527;
- Volman I., Verhagen L., den Ouden HEM, Fernández G., Rijpkema M., Franke B. et al. (2013). Reduced serotonin transporter availability decreases prefrontal control of the amygdala. J. Neurosci. 33 (21), 8974–8979;
- A word about the genetics of behavior;
- A Brief History of Antidepressants;
- Thomas KH, Martin RM, Potokar J, Pirmohamed M, Gunnel D (2014). Reporting of drug-induced depression and fatal and non-fatal suicidal behavior in the UK from 1998 to 2011. BMC Pharmacol. Toxicol. 15, 54;
- Bijl D. (2004). The serotonin syndrome. Net. J. Med. 62 (9), 309–313..
Treatment
No special therapeutic measures have been developed for serotonin syndrome; recommendations regarding its treatment are based on individual case reports. Discontinuation of all serotonergic drugs is the first and main measure for serotonin syndrome, which in most patients leads to a rapid decrease in symptoms within 6-12 hours and to their complete disappearance within 24 hours (in the case of fluoxetine, a more protracted course of several days is possible) .
Other necessary measures are symptomatic therapy and individual care. In severe cases, prescribing serotonin antagonists (cyproheptadine, methysergide); detoxification therapy and other measures aimed at maintaining homeostasis. Paracetamol and external cooling are used to lower body temperature; when body temperature rises to 40.5 C, which indicates a threat to the patient’s life, intensive external cooling, endotracheal intubation with transfer to artificial ventilation and the introduction of muscle relaxants should be used to prevent the occurrence of rhabdomyolysis and disseminated intravascular coagulation. Benzodiazepines (eg, lorazepam) may be used to reduce the muscle rigidity associated with serotonin syndrome and the hyperthermia it often causes. Benzodiazepines can also be used to control agitation; physical restraint should be avoided in serotonin syndrome. For hypertension, direct sympathomimetics in small doses (adrenaline, norepinephrine) are used to maintain normal blood pressure.
The use of propranolol, bromocriptine and dantrolene should be avoided as these drugs may worsen the condition of patients with serotonin syndrome, causing severe side effects and leading to increased mortality. Data regarding the beneficial effects of bromocriptine and dantrolene appear to be the result of misdiagnosis of serotonin syndrome in disorders caused by other causes.
In mild cases (with the presence of hyperreflexia and tremor, but without fever), serotonin syndrome is observed within 24 hours after starting therapy and stopping the drug, but some symptoms may persist for a longer time: this depends on the half-life of the active substance and its active substances. metabolites. Typically, supportive care, including intravenous fluids, vital signs, and benzodiazepines to reduce agitation, is sufficient. However, even such mild patients require supervision due to the possibility of a sudden deterioration in their condition with the need for intensive care.
Neurotransmitter control
Figure 3. Changes in the content of neurotransmitters in rats in a state of aggression. During a fight (gray vertical stripe) and after it, the content of dopamine in the accessory nucleus (A), which regulates behavior and motivation, increases, and the release of serotonin in the frontal cortex decreases (B). Asterisks indicate significant differences from baseline neurotransmitter levels. Figure from [5].
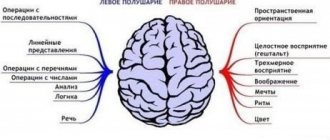
As already mentioned, serotonin is distributed from the medulla oblongata, from the raphe nuclei. A significant difference with the dopamine system is the wider coverage of brain structures by serotonin fibers. This coverage allows serotonin to influence memory processes and cognitive abilities: the pace and quality of thinking. In depression, a decrease in the intensity of serotonin transmission leads to a deterioration in intelligence and slower thinking.
In addition to its effect on intelligence, serotonin has a serious effect on aggressive behavior. For example, the content of dopamine and serotonin in the subcortical structures and frontal lobe was compared in rats during fights [5]. Scientists have found that aggressive behavior in animals is associated with a decrease in serotonin levels in the frontal cortex, which is responsible for planning and controlling behavior (Fig. 3). In humans, a connection has also been shown between reduced levels of serotonin in the frontal cortex and aggressive behavior, but only impulsive behavior that occurs suddenly [6].
Serotonin reduces the activity of neurons in the prefrontal cortex not by directly affecting them, but through inhibitory neurons that secrete gamma-aminobutyric acid (GABA). The neurotransmitter enters receptors located on the body and processes of GABAergic neurons, blocking or triggering signal transmission [7]. It is noteworthy that when the activity of individual neurons decreases under the influence of serotonin, the ordered activity of neural systems increases, that is, serotonin streamlines the joint work of neurons, preventing them from interrupting each other in a polyphonic conversation.
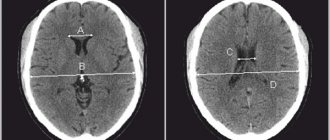
When it comes to the influence of serotonin on personality, it is worth paying attention to one of the genes of the serotonin system - the serotonin transporter protein gene (5-HTT, SERT). There are two variants of the promoter sequence of this gene (serotonin transporter linked polymorphic region, 5-HTTLPR), differing in length, and the short version does its job worse than the long one. When studying the influence of the 5-HTTLPR polymorphism on the characteristics of social life, it turned out that owners of the short allele are more prone to anxious reactions during social interaction [8]. Carriers of the short variant in the homozygous and heterozygous states showed increased sensitivity to emotional stimuli and had worse control over their behavior. A study published in 2013 in The Journal of Neuroscience [9] showed that in those with the short 5-HTTLPR allele, the prefrontal cortex has worse control over the functioning of the amygdala, the center of emotional response (Fig. 4), which is also sensitive to other “emotional” alleles, for example, to polymorphism of the monoamine oxidase-A gene [10]. It was found that throughout life, 5-HTT activity can be influenced by experiences of negative interactions with others, such as childhood abuse. Such events worsen the already weak functioning of the transporter protein, leading to disturbances in brain function, such as those described above.
Figure 4. Excitability of the amygdala (top) and anterior prefrontal cortex (bottom) depending on the polymorphism of the serotonin transporter gene promoter. Owners of the short (S-, dark bars) variant of 5-HTTLPR have higher activation of the amygdala than carriers of the long allele (white bars). On a neurobiological level, this means that the brain is “overwhelmed” by emotions. To cope with this information flow, the observed slight increase in activity of the prefrontal cortex in the left and right hemispheres is not enough. Figure from [9].
Preventive measures
When starting treatment with drugs that affect the serotonin process, constant monitoring by the attending physician is necessary. If any negative consequences occur, the drug is immediately discontinued.
Knowing the possible risk, all drugs from the group of antidepressants are prescribed with extreme caution.
The interval between taking medications or prescribing new types of medications should be at least two weeks. An exception may be the drug Fluoxetine, since the washout time with its use lasts 5-6 weeks, and for elderly patients it is 8 weeks.