Autoregulation of cerebral blood flow (BFF) is a protective mechanism aimed at maintaining cerebral blood flow in response to changes in cerebral perfusion pressure (CPP) and cerebrovascular resistance (CVR) [1]. The term was proposed by N. Lassen in 1959 [2]. In this case, CPP is the difference between mean arterial pressure and intracranial pressure (ICP) and is inversely proportional to CVR. CVR, in turn, represents the total vascular resistance, including arterioles of the pia mater and penetrating precapillary arterioles of the brain [3]. The speed of cerebral blood flow is directly proportional to CPP and inversely proportional to CVR.
There are a number of mechanisms involved in the regulation of maintaining the level of cerebral blood flow (the norm is 50 ml/100 g/min): 1) metabolic
(blood pH, balance of CO2/O2 dissolved in the blood, nitric oxide, adenosine, products of the functioning of astrocytes and neurons) [4, 5];
2) myogenic
(Ostroumov-Beilis effect - a reaction from the smooth muscle layer of arteries in the form of contraction when blood pressure increases and relaxation when blood pressure decreases);
3) peripheral (or systemic) (activity of the sympathoadrenal system, carotid glomeruli, temperature, endothelial factors); 4) neurogenic
(vasomotor center, centers for regulating the activity of the sympathetic system and, possibly, a number of other brain structures). The links of the latter are the least studied.
All AUB mechanisms ensure the maintenance of cerebral perfusion when blood pressure fluctuates between 60-70 and 170-180 mmHg. When blood pressure increases or decreases beyond this range, a breakdown of autoregulation occurs—a condition in which cerebral blood flow passively depends on systemic blood pressure, and ICP becomes directly dependent on blood pressure. This condition is dangerous both due to the development of ischemia and the development of “luxury perfusion syndrome”, reactive hyperemia, associated with a high risk of secondary ischemic or hemorrhagic complications.
BUN is often disrupted in the acute period of severe traumatic brain injury (sTBI), which occurs with hemodynamic instability and is associated with an unfavorable outcome. Assessing the state of the AUB currently serves as the main objective guideline for monitoring and correcting conservative treatment and making a decision on neurosurgical intervention in the acute period of mTBI [6]. For patients with impaired autoregulation due to TBI, achieving the recommended level of CPP (not lower than 70 mm Hg) may be associated with cerebral hyperemia, predisposing to the formation of intracranial hypertension, edema and intracerebral hemorrhage [6]. Therefore, according to the latest recommendations, for this group of patients the required CPP limit is reduced to 60 mmHg. [7]. Recent studies [3] have shown that maintaining CPP levels below 50-60 mm Hg. is associated with a large number of positive outcomes, while CPP is more than 70-80 mm Hg. more often leads to unfavorable outcomes in patients with impaired BUN.
In the classic works of N. Lundberg [8], three types of spontaneous ICP oscillations are identified: A-waves (plateau), B- and C-waves. Subsequent studies showed that plateau waves reflect cerebral vasodilation, which leads to an increase in cerebral blood flow and, as a consequence, an increase in ICP [9]. Currently, one of the most reliable and safe methods for continuous assessment of the autoregulation of the state of cerebral vessels in the acute period of mTBI is based on the analysis of wave fluctuations of arterial and intracranial pressure - monitoring the reactivity coefficient of cerebral vessels
(pressure reactivity index -
P R x
). PRx is the correlation coefficient between slow-wave fluctuations in blood pressure and ICP [10, 11]. It has been shown that plateau waves of ICP in patients with TBI are more often recorded when the autoregulation of cerebral vessels is preserved. At the moment of formation of plateau waves, maximum vasodilation of arterioles develops and autoregulation is lost, which is recorded by an increase in PRx [12].
Previously, experimental studies [13, 14] showed that damage to certain structures of the brain stem and hypothalamus is accompanied by the development of cerebral edema. Electrical stimulation of individual brainstem structures initiates processes leading to cerebral vasodilation and an increase in volumetric cerebral blood flow [15, 16]. It is assumed that the brainstem may be directly involved in the generation of waves characteristic of intracranial hypertension, but the anatomical pathways and mechanisms of this influence are still not well understood. A number of experimental studies have shown the effect of stimulation of individual structures of the brainstem (including the locus coeruleus - locus coeruleus) of the reticular formation of the medulla oblongata and hemispheric structures of the brain (in particular, the anterior cingulate gyrus and anterior parts of the hypothalamus) on changes in ICP [17]. It was also previously shown that damage to brain stem structures and frontal lobes during TBI can lead to changes in the activity of the sympathetic nervous system, affecting arterial tone [18].
A feature of DAP is the predominant damage to the subcortical and stem structures of the brain involved in maintaining vital functions, including the regulation of cerebral vascular tone and BUN.
The purpose of this work is to identify anatomical damage to deep brain structures that influence the degree and duration of BUN disturbances in the acute period of severe DAP.
Material and methods
The analysis included 37 patients with mTBI (3-8 points on the Glasgow Coma Scale) who were treated in the intensive care unit of the National Medical Research Center for Neurosurgery named after. N.N. Burdenko in the period from 2009 to 2014. The inclusion criteria were met by patients who, according to clinical indications, required monitoring of blood pressure, ICP, CPP and in whom MRI of the brain revealed signs of DAP. Monitoring data was stored, analyzed and calculated using ICM Plus software. In total, the analysis included 23 men and 12 women, whose average age was 28±12.4 years. Seven patients in this group underwent decompressive craniotomy due to diffuse cerebral edema.
In the intensive care unit, patients were given mechanical ventilation, PaCO2 was maintained at 35-45 mm Hg, PaO2 was not lower than 100 mm Hg, sedation and analgesia were administered (propofol 1-3 mg/kg/h or midazolam 10-30 mcg/kg/h, fentanyl 1-2 mcg/kg/h). CPP was maintained above 60 mm Hg. When ICP is above 20 mm Hg. bolus administration of 15% mannitol (0.25-1 g/kg) or Hyperhaes at a dose of 2-3 ml/kg was used.
The Glasgow Coma Scale (GCS) was used to assess the depth of coma [19, 20]. TBI outcomes were assessed using the Glasgow Outcome Scale (GOS) [20, 21]. Brain damage in DAP was assessed using a classification based on MRI data [22]. The location and level of brain damage were assessed using the MRI classification proposed by N.E. Zakharova et al. [23].
All patients underwent ICP monitoring in accordance with international recommendations and the protocol of the Association of Neurosurgeons of the Russian Federation [7, 24]. ICP monitoring was carried out using a Codman ICP Express Monitor and a Codman MicroSensor (Jonson & Johnson Professional, Inc., Raynham, USA). The ICP sensor was implanted into the white matter of the brain through the trefination foramen in the projection of Kocher's point into the premotor zone of the subdominant hemisphere. BUN was assessed by monitoring the cerebral vascular reactivity index PRx [10]. The average duration of PRx monitoring was 7 days. The ratio of the duration of the period of impaired autoregulation to the total duration of monitoring of this parameter was also assessed.
BP monitoring was performed using direct measurement through an arterial catheter placed in the radial, femoral, or dorsalis pedis arteries.
Based on the calculation of the average PRx coefficient for the entire observation period when monitoring ICP and CPP, two groups of patients were identified:
1st group
— with preserved AUB — PRx [–1; 0];
2nd group
— with partially or completely lost AUB — PRx (0; 1].
The characteristics of patients in each group are presented in Table. 1.
Table 1. Comparative analysis of groups with intact and impaired AUB Note. Abbreviations: GCS - Glasgow Coma Scale, GOS - Glasgow Outcome Scale, DAP - diffuse axonal injury, ICP - intracranial pressure, ICH - intracranial hypertension, PRx - cerebral vascular reactivity coefficient. Group 1 consisted of 19 patients. In 16 (84.2%) of them, the cause of injury was a traffic accident. Brain stem damage was diagnosed in 15 (78.9%) patients during MRI.
Group 2 was represented by 18 patients. In 15 of them, the cause of injury was a traffic accident. Seven patients underwent decompressive trepanation due to diffuse cerebral edema. In 15 (83.3%) patients in this group, brain stem damage was visualized during MRI.
Neuroimaging methods.
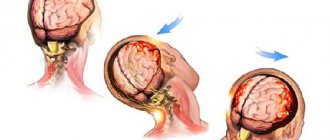
MRI of the brain was performed on a 3 T GE tomograph in standard modes (T1, T2, FLAIR) and SWI/T2* GRE, DWI modes, which made it possible to evaluate both ischemic and small hemorrhagic focal lesions. In each patient, according to MRI data, damage to individual subcortical structures and areas of the brain stem, which are projections of the main neurotransmitter systems of the brain, was assessed (Fig. 1),
Rice.
1. Location of brain structures included in factor analysis. NC - caudate nucleus, Put - putamen, GPi - internal segment of the globus pallidus, GPe - external segment of the globus pallidus, Tha - thalamus, SN - substantia nigra, VTA - ventral tegmental area, MN - Meynert's nucleus, LDT - laterodorsal tegmental nucleus, PPN - pedunculopontine nucleus, NR - red nucleus, LC - locus coeruleus. Dopaminergic brain structures are highlighted in red, noradrenergic in blue, cholinergic in green, glutamatergic in orange, and GABAergic brain structures in purple. as well as areas of damage to the frontal lobes (mediobasal, pole and dorsolateral sections). Statistical methods.
Data processing was carried out in the Statistica 8.0 software package.
(StatSoft Inc, USA). In all cases, nonparametric tests were used for statistical evaluation. To analyze qualitative characteristics, Fisher's test ( F
) was used; odds ratios, sensitivity and specificity of each factor were calculated to assess the influence of anatomical factors on the risk of developing unstable hemodynamics.
Results were considered statistically significant at p
< 0.05.
Cerebrovascular disorders are one of the main causes of mortality and the leading cause of disability in the adult population [1]. To date, the mechanisms of acute stroke have been studied in detail, risk factors for the development of the disease have been established, and information has been obtained about its characteristics and prevalence in the population. Chronic cerebrovascular disorders (CCD) pose a serious problem: many issues of pathogenesis and classification of this pathological condition require clarification; many aspects of pathogenetic therapy of patients with CCD require further study.
In real practice, there is often a contrast between acute cerebrovascular accidents (stroke) - a clinical syndrome, the most important distinguishing feature of which is the acute occurrence of focal neurological deficit, and CRMC, in which, despite the existing structural changes in the brain substance caused by its vascular damage, diffuse (fine-focal) neurological symptoms, the exact timing of which cannot be determined. The severity of such symptoms may be so insignificant that its identification requires the use of additional diagnostic methods (neuroimaging, neuropsychological examination). In the domestic literature, CRMC is traditionally considered as discirculatory encephalopathy. This term refers to brain damage caused by a vascular disease, which has a chronic progressive course and against which paroxysmal (step-like) episodes of deterioration of the patient’s condition are observed. Currently, to diagnose this condition, the term “chronic cerebral ischemia” is used, which is not fully identical to the concept of “dyscirculatory encephalopathy”. It is not always possible to draw a clear line between acute and chronic ischemic brain lesions, especially based solely on an analysis of the clinical picture of the disease. In this regard, of interest are asymptomatic (“silent”) cerebral infarctions, which, without clinically manifesting themselves as focal lesion syndrome, over time lead to an increase in neurological deficit and the formation of cognitive impairment [2].
To describe similar pathological conditions, it is proposed to use the term “small vessel disease” (SVD) [3]. It is believed that damage to the brain substance in this condition may be caused by damage not only to arterioles and small arteries, but also to the involvement of capillaries and small veins in the pathological process [4]. The main consequences of BMS are structural lesions of the medulla in the form of ischemic strokes (primarily lacunar), cerebral hemorrhages, and leukoaraiosis [5]. Obviously, the combination of chronic and acute cerebral circulatory disorders in BMS more accurately characterizes the pathogenesis of CRMC and is more consistent with the concept of “dyscirculatory encephalopathy” than “chronic cerebral ischemia.” The development of BMS is closely associated with arterial hypertension (AH), diabetes mellitus, and age [6, 7]. The course of the disease is largely determined by the nature of the damage to the vascular bed (involvement of large or small arteries in the pathological process), and the presence of concomitant diseases.
Microangiopathies
One of the common causes of CRMC is damage to small-caliber arteries (myocroangiopathy). A feature of the blood supply to the brain is the presence of powerful systems of anastomoses between large (circle of Willis, extra- and intracranial anastomoses), as well as pial arteries, providing the possibility of blood flow. The collateral circulation system allows you to compensate for even a pronounced narrowing or complete occlusion of one of the main arteries of the head. A significant part of the brain substance is supplied with blood by penetrating arteries that arise from the pial arteries and rush deep into the brain parenchyma [8]. These vessels extremely rarely anastomose with each other, and with their stenotic or occlusive lesions, the possibility of developing collateral blood flow is insignificant, which creates the preconditions for ischemic damage to the structures they supply [9].
On the other hand, small-caliber arteries and arterioles that provide blood flow to the basal ganglia and brain stem arise directly from the vessels of the circle of Willis and its proximal large branches, as a result of which they are significantly susceptible to changes in hypertension and increased stiffness of the wall of the aorta and great arteries [10]. These vessels do not have the conditions to compensate for high pulse pressure, which results in expansion of the perivascular spaces. A characteristic consequence of hypertension is hypertensive microangiopathy with a decrease in the lumen of arteries and arterioles, a decrease in vascular reactivity and a decrease in tissue blood flow. Morphological changes in the vascular bed in hypertension, features of damage to small arteries and the resulting changes in the brain substance have now been studied in detail [11]. Due to the fact that hypertension affects various parenchymal organs with a network of small-caliber arteries, the clinical picture of the disease is characterized by diffuse damage to the brain, retina, kidneys, etc. [12].
Diabetes mellitus plays an exceptional role in the development of microangiopathy [13]. The progression of the pathological process becomes more rapid when diabetes mellitus and A.G. are combined. An important mechanism of vascular damage is endothelial dysfunction, which occurs in both hypertension and diabetes mellitus. Hyperglycemia, insulin resistance, hyperlipidemia and hyperhomocysteinemia, which are integral parts of the pathogenesis of diabetes, initiate the activation of systemic inflammation and disorders of nitric oxide synthesis, which leads to even more rapid progression of microangiopathy [14].
Modern diagnostic methods for studying the vascular bed (contrast angiography, magnetic resonance angiography) do not allow intravital assessment of the state of the microvascular bed and verification of the presence of microangiopathy. Its diagnosis is possible on the basis of indirect signs: impaired cognitive functions and markers of brain damage detected using magnetic resonance imaging in the form of small (lacunar) infarctions, hyperintense white matter lesions, expansion of perivascular spaces, microhemorrhages and medulla atrophy [15]. It is the expansion of the perivascular spaces that is currently considered one of the most important neuroimaging markers of microangiopathy. In a study of 2612 elderly and senile patients, expansion of the perivascular spaces was detected in 16.2% of the examined [16]. Its presence was associated with a high risk of developing subcortical infarction, microhemorrhage, as well as a 4-fold increase in the risk of developing dementia.
One of the common forms of damage to small-caliber cerebral arteries is amyloid angiopathy, characterized by the deposition of β-amyloid in the leptomeningeal and cortical arteries and arterioles with a violation of their elastic properties [17]. The consequences of such angiopathy are the development of lobar intracerebral hematomas and microhemorrhages. The risk of developing amyloid angiopathy increases with age, and its presence is associated with cognitive decline and Alzheimer's disease. There is evidence that various microangiopathies, including inflammatory and genetically determined ones, are more common in the Asian population compared to the European population, and damage to small arteries is associated with older age and the presence of hypertension [18].
Damage to large arteries
The state of cerebral hypoperfusion is possible not only with damage to small-caliber arteries, but also in conditions of stenosing damage to larger arteries of the arterial trunks located proximal to the circle of Willis. It should be noted that for a long period of time, starting from the beginning of the 20th century, it was “hardening of the arterial wall” that was considered as the main cause of the development of dementia (atherosclerotic dementia) [19].
An important factor limiting the flow of arterial blood to the brain is an increase in the stiffness of the arterial wall of the aorta and large arteries. Hemodynamic disturbances in this situation are caused not directly by stenotic (usually atherosclerotic) lesions, but also by disturbances in the regulation of the lumen of blood vessels. The results of a large-scale Reykjavik study [20], which included 1860 patients, showed that increased aortic wall stiffness (assessed based on pulse wave velocity and calculation of the carotid-femoral index) was significantly associated with the severity of periventricular white matter lesions. According to the authors, more pronounced damage to the medulla in the elderly patients included in the study, due to increased rigidity of the vascular wall, occurred due to the involvement of small-caliber arteries in the pathological process and their remodeling.
Due to the aging of the body, a decrease in the elasticity of the vascular wall is observed, which is primarily recorded in large arteries of the elastic type. It is believed that the earliest increase in vascular wall stiffness occurs in the aorta; these changes precede changes in the physical properties of smaller arteries, in particular the brachial one [21]. An increase in vascular resistance is recorded even before the development of hypertension; it is noteworthy that the level of diastolic blood pressure (BP) is usually identical when measured in the aorta and brachial artery, while systolic blood pressure values differ depending on the diameter of the artery, which can be considered as one from the cardiovascular risk stratification criteria [22]. In this regard, the connection between an increase in aortic wall stiffness in middle-aged patients and the degree of damage to the periventricular white matter, considered as a marker of CRMB, is quite understandable [23]. Noteworthy is the fact that damage to the periventricular white matter, in terms of the time of its occurrence, precedes the development of hypertension in such patients (at the stage of prehypertension). Early damage to the medulla under these conditions may be due to the proximity of the aorta, brachiocephalic trunks and cerebral arteries directly, which ensures the transmission of high pulse hypertension to intracranial structures [24]. Factors predisposing to early damage to the brain substance with increased rigidity of the aortic wall are the high need of brain tissue for blood flow, as well as the insufficiency of damping mechanisms of its vascular system, the presence of which would reduce the level of pulse blood pressure [25]. It has also been shown that increased aortic wall stiffness is associated with white matter damage not only in elderly patients with other cardiovascular risk factors, but also in young and middle-aged patients (30-45 years) [26].
Deterioration of the elastic properties of the wall of large arteries is observed not only with their atherosclerotic lesions, but also with some other pathological conditions, in particular with hyperhomocysteinemia. In conditions of an experimental nutritional increase in the concentration of homocysteine in the blood of healthy people, an increase in pulse pressure, a marker of the stiffness of large arteries, was shown, but not a violation of endothelium-dependent vasodilation caused by a violation of the regulation of the lumen of small arteries [27]. Probably, normalization of vascular resistance would improve the hemodynamic situation and help slow down the rate of progression of vascular damage to the brain under these conditions.
Cerebral blood flow and blood pressure levels
Hypertension is an important factor in reducing local cerebral blood flow. Normalization of systemic blood pressure, even in the case of adequate control of hypertension using various classes of antihypertensive drugs, in itself is not able to ensure the proper level of cerebral perfusion and preservation of brain tissue volume. It has been demonstrated [28] that patients with essential hypertension have a progressive decrease in gray matter, which increases to a much greater extent than in their elderly peers with normal blood pressure levels.
Despite the fact that disturbances in the supply of oxygen and glucose to brain cells predominate in the development of CRMC, the pathogenetic role of ischemia itself is modulated by other factors. In particular, the severity of damage to the white matter of the cerebral hemispheres is significantly influenced by the processes of systemic inflammation. It has been demonstrated [29] that the presence of markers of a systemic inflammatory process in the peripheral blood (the study authors determined the concentration of C-reactive protein in the blood) in middle-aged patients is associated with more pronounced damage to the periventricular and deep white matter in old age. Interestingly, this association turned out to be characteristic only for APOE-ε4-positive patients. Also noteworthy is the lack of connection between high blood concentrations of C-reactive protein in middle-aged patients and the presence of cerebral infarctions and cerebral hemorrhages in old age.
The presence of hypertension is a factor contributing to the progression of cognitive impairment in patients with Alzheimer's disease [30]. The authors of this study found that Alzheimer's disease patients with hypertension had decreased hippocampal glucose metabolism and worse neuropsychological testing results compared with Alzheimer's disease patients with normal blood pressure levels. There was no connection between the presence of hypertension and the level of amyloid accumulation in the brain tissue (assessed based on the study of cerebrospinal fluid and using positron emission tomography with phlobetapir), which allows us to consider hypertension as an independent risk factor for the progression of cognitive impairment in Alzheimer's disease.
To date, sufficient information has been accumulated that in a significant proportion of patients, arterial hypotension is closely associated with the risk of damage to brain tissue, primarily white matter [31]. The adverse effects of arterial hypotension on the structure and function of the brain were noted both for persistent hypotension and for orthostatic and postprandial arterial hypotension.
There is a risk of developing cerebral hypoperfusion and, accordingly, brain damage in patients with low blood pressure levels. This dependence is especially characteristic of elderly and senile patients. However, arterial hypotension itself is not always directly related to the risk of brain damage. Thus, it has been shown that increasing atrophy of the gray matter of the cerebral cortex is associated with low levels of systolic and pulse blood pressure, as well as with a decrease in tissue cerebral blood flow [32].
Dysregulation of cerebral circulation
Providing the brain with blood and, accordingly, oxygen and glucose is a complex physiological process, which is determined by a number of factors: first of all, the need of neuronal populations for the supply of energy substrates, secondly, the state of central hemodynamics, mainly systemic blood pressure. Modern ideas about the physiological mechanisms of blood supply to the brain are described by the concept of a neurovascular unit, which ensures the most complete correspondence of blood flow to certain areas of the brain with their need for energy substrates in a specific period of time [19]. The supply of blood adequate to the needs of the tissue is ensured by fine adjustment of the lumen of the vessels, which is produced in response to fluctuations in the level of systemic blood pressure and changes in local neuronal activity, while the most important stimuli that determine vasodilation are carbon dioxide tension and the extracellular concentration of potassium ions, nitric oxide, arachidonic acid metabolites acid, adenosine, some neuropeptides and neurotransmitters [33]. Numerous physiological signals coming from astrocytes, pericytes, endothelial cells embedded in the walls of arteries and arterioles and efferent nerve endings control the contractions of smooth muscles and the regulation of the lumen of arteries and arterioles. In addition, receptors embedded in the vascular wall are able to perceive mechanical stimuli that reflect tension in the lumen of the vessel due to increased blood pressure, due to which the mechanism of autoregulation of cerebral circulation is realized, ensuring the constancy of cerebral blood flow even with significant fluctuations in systemic blood pressure [34]. Exact compliance with the needs of neurons and glia cells of incoming oxygen, glucose and some other substrates for the formation of high-energy molecules and the biosynthesis of substances necessary for the normal functioning of the nervous system ensures fine regulation of metabolic processes, economical use of resources and timely removal from tissues of metabolic products, the excess of which can be dangerous . In addition to synthetic functions, the extremely high need of the brain for oxygen and glucose is explained by the need for constant operation of ion pumps, which are responsible for maintaining the membrane potential and performing functions specific to nervous tissue—the generation and conduction of an electrical impulse [35].
Regulation of the lumen of the cerebral arteries in response to physiological stimuli occurs due to changes in the lumen of the large and pial arteries and arterioles. At the same time, brain capillaries, the walls of which are devoid of a muscular layer, are practically incapable of actively changing their lumen and do not take a significant part in the regulation of local blood flow [36]. At the level of the capillary segment of the vascular bed, a blood-brain barrier is formed, and metabolic processes take place between blood and nerve cells [37]. An important role in ensuring autoregulation of cerebral circulation is played by small-caliber arteries, which are significantly affected by hypertension and diabetes mellitus. In addition, there is a significant decrease in their ability to respond to physiological stimuli, such as insufficient dilation ability. Such damage, as a rule, is diffuse and involves different vascular systems of the brain [38].
In the case when the functioning of the mechanisms regulating cerebral circulation is ineffective, cerebral blood flow passively follows systemic blood pressure and its level decreases under conditions of arterial hypotension [39]. Blood flow disturbances in this situation are described by the concept of the “last meadow”, according to which damage to the large cerebral or extracranial great arteries leads to hypoperfusion in the areas of adjacent circulation located between the areas receiving blood from the anterior, middle and posterior cerebral artery systems, as well as in areas of the subcortical ganglia and internal capsule [40].
With regard to the pathogenesis of CRMC, it is important to note that areas of adjacent blood circulation that are vulnerable to fluctuations in systemic blood pressure are located in the area of the periventricular white matter, which is supplied with blood by penetrating arteries, as well as the hippocampus, which receives blood from the small branches of the anterior choroidal and posterior cerebral arteries [41]. The risk of ischemic damage to these areas increases not only due to the fact that the bulk of the white matter and subcortical nuclei are supplied with blood by end-type arteries that have virtually no anastomoses, but also due to impaired autoregulation of cerebral circulation.
Dysfunction of cerebrovascular regulation in patients with stenotic atherosclerosis of the carotid arteries is associated with an increased risk of developing ischemic brain damage. The results of a meta-analysis of 13 studies (991 patients included, average follow-up 32.7 months) showed that a decrease in cerebrovascular reactivity significantly increases the risk of developing transient ischemic attacks (TIA) and ischemic stroke, and the likelihood of their development does not depend on whether the existing stenosis was symptomatic or asymptomatic [42].
Dysfunction of the endothelium plays an important role in dysregulation of the lumen of blood vessels. One of the important consequences of endothelial dysfunction is an increase in the sensitivity of arterial wall receptors to vasoconstrictors or physical factors that cause vasoconstriction [43]. It has been shown that endothelial dysfunction is closely associated with a certain type of vascular lesion and the development of lacunar infarctions [44]. To understand the mechanisms of development of CRMC, it is also important that endothelial dysfunction is involved in the pathogenesis of lacunar infarctions in patients with asymptomatic cerebral infarctions and diffuse white matter lesions [45].
Correction of cerebral circulation in the treatment of patients with CRMC
Based on the position that the pathogenesis of ischemic brain damage lies in the obstruction of arterial patency, over the course of many decades, attempts have been made repeatedly to use drugs that have a vasodilator effect. However, the use of vasodilators has not demonstrated its effectiveness in conditions of acute cerebral ischemia, both in experimental and clinical settings [46, 47]. This is largely due to the fact that in conditions of total thrombosis or embolism of one or more arteries, their dilatation is not able to compensate for disturbances in local blood flow. Similarly, with complete occlusion of the arterial trunk due to atherosclerosis or microangiopathy, the administration of vasodilators cannot restore blood flow through the stenotic vessel, and the dilation of nearby unchanged or less affected arteries will not be able to facilitate the flow of blood into the unchanged area due to the poor development of the network of collateral vessels in the brain tissue brain [48].
At the same time, the use of a number of vasodilators can be considered justified in a situation where cerebrovascular disease is caused by a partial narrowing of small arteries and arterioles that have retained the ability to respond to external influences [9]. The possibility of using drugs that not only have a vasodilating effect, but also restore the sensitivity of arterial wall receptors to physiological stimuli and, accordingly, increase the impaired ability for autoregulation of cerebral circulation, seems promising. There is also evidence that the administration of cerebral vasodilators can be effective along with the simultaneous use of antiplatelet agents [49].
In order to restore blood flow through narrowed arteries and slow down the rate of progression of CRMC, it was proposed to use blockers of slow calcium channels, in particular dihydropyridine derivatives, capable of modulating the lumen of cerebral capillaries and small arteries that have retained their normal structure and ability to perceive appropriate stimuli [50]. The results of a number of clinical studies have demonstrated the ability of drugs in this group to slow the progression of vascular dementia.
Of significant practical interest is the possibility of not only providing vasodilation, thereby increasing the level of cerebral perfusion, but also restoring the autoregulation of cerebral blood flow, i.e., normalizing the response of the vascular wall to physiological stimuli. Under experimental conditions, it was demonstrated that the administration of angiotensin-converting enzyme inhibitors to spontaneously hypertensive rats led to the restoration of autoregulation of cerebral circulation and a decrease in the incidence of death, without having a significant effect on the level of systemic blood pressure [51]. Similarly, the use of angiotensin II receptor inhibitors in an experimental model of hemorrhagic stroke in spontaneously hypertensive rats ensured the restoration of autoregulation of cerebral circulation, and was also accompanied by a decrease in the severity of blood-brain barrier dysfunction and the severity of cerebral edema [52]. It is noteworthy that the protective effect of the studied drugs under the conditions of this experiment was also not associated with a decrease in systemic blood pressure. The restoration of arterial function could be associated with the normalization of both the endothelial and myogenic components of the regulation of vascular tone. In experimental and clinical settings, the ability of voltage-gated calcium channel blockers has been demonstrated to eliminate excessive contraction of the muscles of small-caliber cerebral arteries, preventing vasospasm and an excessive increase in vascular resistance [53].
Nicergoline (Sermion), an ergoline derivative, has shown its effectiveness in treating patients with CRMC. The drug improves metabolic and hemodynamic processes of the brain, reduces platelet aggregation and improves hemorheological blood parameters, increases the rate of tissue perfusion. Nicergoline exhibits an α1-adrenergic blocking effect, leading to improved blood flow, and also has a direct effect on the cerebral neurotransmitter systems - adrenergic, dopaminergic and cholinergic.
For a long period of time, nicergoline has been used to treat patients with various types of vascular lesions of the brain, as well as patients with cognitive impairment, including Alzheimer's disease. The first systematic review [54] devoted to studying the effectiveness of the drug showed that its use for 2 to 12 months is accompanied by a slowdown in the progression of cognitive decline, recorded on the standard MMSE scale. The drug is considered promising for the treatment of patients with Alzheimer's disease and other types of dementia [55].
Nicergoline has positive effects on the state of brain functions both due to improved cerebral circulation at the level of macro- and microcirculation, and directly due to its own effect on various parts of cerebral metabolism [56]. L. Iliff et al. [57] in 1977 were among the first to study the effect of the drug on cerebral blood flow. In accordance with the study protocol, 13 patients with different forms of cerebrovascular pathology (10 with multi-infarct dementia, 3 with repeated TIAs) were administered intravenous nicergoline (2 mg). The intensity of cerebral blood flow was assessed by the clearance of radioactive xenon (Xe133), which was administered intracarotidly. In 7 patients there was a significant increase in hemispheric blood flow, which confirmed the assumption of a positive effect of the drug on cerebral hemodynamics. A number of studies conducted at the same time using various, including invasive, methods for assessing cerebral blood flow confirmed the ability of nicergoline to improve cerebral hemodynamics in patients with vascular lesions of the brain.
Subsequent studies made it possible to significantly expand the understanding of the pharmacological effects of nicergoline and explain the mechanism of its action in patients with various brain diseases. At the same time, the authors who studied the possibility of its clinical use noted the good tolerability of the drug and the low incidence of side effects inherent in other ergot derivatives. Sermion can be prescribed as a therapy for patients with CRGM, as well as with cognitive impairment caused by a combination of ischemic brain damage and a neurodegenerative process.
The authors declare no conflict of interest.
results
MRI analysis data showed that all patients in the analyzed sample had signs of diffuse brain damage involving the hemispheric and in 29 (78.4%) of 37 patients - brainstem structures. At the same time, the small number of patients in the groups with intact and impaired autoregulation did not allow us to identify significant differences in the outcomes according to the GOS severity of injury according to the GCS. The groups did not differ from each other in gender and age characteristics. Localization and depth of brain damage assessed according to the classifications of R. Firsching et al. [22] and N.E. Zakharova et al. [23], also did not differ significantly between the comparison groups (see Table 1).
Prevalence of damage to brain stem and subcortical structures in impaired AMB
Next, a statistical analysis was carried out on the frequency of occurrence of unilateral or bilateral damage to each brain structure in patients with impaired (group 2) and intact (group 1) autoregulation (Table 2).
Table 2. Frequency of unilateral and/or bilateral damage to brain structures in patients with normal and impaired autoregulation Note. *—significant differences between groups.
Statistical analysis of the data showed that in patients with traumatic brain injury, accompanied by disturbances of the AMB in the acute period of injury, in general, damage to the brainstem was observed somewhat more often than in the group of patients with normal autoregulation. Among the studied stem structures, significantly more often ( p
=0.02) in patients of group 2, there was structural damage to the substantia nigra of the midbrain - a structure that is the source of dopaminergic projections for the neostriatum, cingulate cortex, olfactory nuclei, posterior hypothalamus and tonsils of the brain.
The odds ratio was 5.333 (95% CI 1.252, 29.346), sensitivity 62.5% and specificity 76.2%. Also, more frequent damage to the cholinergic structure - the area of Meynert's nucleus - was revealed in patients with impaired autoregulation ( p
= 0.01), and unilateral or bilateral damage to this area of the brain had a fairly high specificity (81%) for patients in this group.
Additionally, the frequency of occurrence of combined damage to the substantia nigra and Meynert's nucleus was assessed, which significantly prevailed in the group with impaired autoregulation ( p
= 0.02). The odds ratio was 7.39 (95% CI 1.043, 65.37), sensitivity 43.8% and specificity 90.5%.
Thus, the analysis showed that impaired autoregulation of cerebral blood flow in patients with brain DAP is often associated with the presence of primary damage to the substantia nigra, the area of Meynert’s nucleus, and their combination (Fig. 2).
Rice. 2. MRI of the brain of patients with severe TBI with damage to the structures of the substantia nigra (a), the area of Meynert’s nucleus (b), combined damage to the substantia nigra and the area of Meynert’s nucleus (c). Damage is indicated by arrows.
Prevalence of damage to subcortical and brain stem structures in long-term autoregulation disorders
To analyze the effect of damage to the subcortical and stem structures of the brain on the parameter of autoregulation of blood flow (PRx), patients were divided into three approximately equal groups depending on the duration of the period of lost autoregulation (PRx>0.2) relative to the entire measurement time: 1) less than 20% time ( n
=17);
2) 20–34% of the time ( n
=10);
3) 35% of the time or more ( n
=10). The results of this analysis are presented in table. 3.
Table 3. Frequency of damage to brain structures in patients with different durations of autoregulation disorders (as a percentage of the duration of ICP measurement) Note.
* — differences between groups 1 and 3; # — differences between the 2nd and 3rd groups. It was found that in patients with lost autoregulation more than 35% of the measurement time, trunk damage was somewhat more likely to be present. In this group of patients, injuries to the substantia nigra were significantly more common ( p
=0.05).
The odds ratio was 5.6 (95% CI 0.785, 45.938), sensitivity and specificity were 70 and 70.6%, respectively. Also in this group, more frequent damage to the Meynert nucleus region was noted ( p
= 0.04). The odds ratio was 7.6 (95% CI 1.006, 68.466), sensitivity and specificity were 70 and 76.5%, respectively.
According to the results of this analysis, significant differences remained in the frequency of damage to the substantia nigra, the area of the Meynert nucleus and their combination between extreme groups (with the duration of impaired autoregulation less than 20% and more than 35% of the measurement time). Thus, the presence of primary damage to the brainstem in the area of the substantia nigra and basal forebrain (Meynert's nucleus area) makes a significant contribution to the disruption of the AUB mechanisms.
NSICU.RU neurosurgical intensive care unit website of the intensive care unit of the N.N. Research Institute Burdenko
Autoregulation of cerebral blood flow (BFF) is a protective mechanism aimed at maintaining cerebral blood flow in response to changes in cerebral perfusion pressure (CPP) and cerebrovascular resistance (CVR) [1]. The term was proposed by N. Lassen in 1959 [2]. In this case, CPP is the difference between mean arterial pressure and intracranial pressure (ICP) and is inversely proportional to CVR. CVR, in turn, represents the total vascular resistance, including arterioles of the pia mater and penetrating precapillary arterioles of the brain [3]. The speed of cerebral blood flow is directly proportional to CPP and inversely proportional to CVR.
There are a number of mechanisms involved in the regulation of maintaining the level of cerebral blood flow (the norm is 50 ml/100 g/min): 1) metabolic (blood pH, balance of CO2/O2 dissolved in the blood, nitric oxide, adenosine, products of the functioning of astrocytes and neurons) [ 4, 5]; 2) myogenic (Ostroumov-Beilis effect - a reaction from the smooth muscle layer of arteries in the form of contraction when blood pressure increases and relaxation when blood pressure decreases); 3) peripheral (or systemic) (activity of the sympathoadrenal system, carotid glomeruli, temperature, endothelial factors); 4) neurogenic (vasomotor center, centers for regulating the activity of the sympathetic system and, possibly, a number of other brain structures). The links of the latter are the least studied.
All AUB mechanisms ensure the maintenance of cerebral perfusion when blood pressure fluctuates between 60-70 and 170-180 mmHg. When blood pressure increases or decreases beyond this range, a breakdown of autoregulation occurs—a condition in which cerebral blood flow passively depends on systemic blood pressure, and ICP becomes directly dependent on blood pressure. This condition is dangerous both due to the development of ischemia and the development of “luxury perfusion syndrome”, reactive hyperemia, associated with a high risk of secondary ischemic or hemorrhagic complications.
BUN is often disrupted in the acute period of severe traumatic brain injury (sTBI), which occurs with hemodynamic instability and is associated with an unfavorable outcome. Assessing the state of the AUB currently serves as the main objective guideline for monitoring and correcting conservative treatment and making a decision on neurosurgical intervention in the acute period of mTBI [6]. For patients with impaired autoregulation due to TBI, achieving the recommended level of CPP (not lower than 70 mm Hg) may be associated with cerebral hyperemia, predisposing to the formation of intracranial hypertension, edema and intracerebral hemorrhage [6]. Therefore, according to the latest recommendations, for this group of patients the required CPP limit is reduced to 60 mmHg. [7]. Recent studies [3] have shown that maintaining CPP levels below 50-60 mm Hg. is associated with a large number of positive outcomes, while CPP is more than 70-80 mm Hg. more often leads to unfavorable outcomes in patients with impaired BUN.
In the classic works of N. Lundberg [8], three types of spontaneous ICP oscillations are identified: A-waves (plateau), B- and C-waves. Subsequent studies showed that plateau waves reflect cerebral vasodilation, which leads to an increase in cerebral blood flow and, as a consequence, an increase in ICP [9]. Currently, one of the most reliable and safe methods for continuous assessment of autoregulation of the state of cerebral vessels in the acute period of mTBI is based on the analysis of wave fluctuations of arterial and intracranial pressure - monitoring of the pressure reactivity index (PRx). PRx is the correlation coefficient between slow-wave fluctuations in blood pressure and ICP [10, 11]. It has been shown that plateau waves of ICP in patients with TBI are more often recorded when the autoregulation of cerebral vessels is preserved. At the moment of formation of plateau waves, maximum vasodilation of arterioles develops and autoregulation is lost, which is recorded by an increase in PRx [12].
Previously, experimental studies [13, 14] showed that damage to certain structures of the brain stem and hypothalamus is accompanied by the development of cerebral edema. Electrical stimulation of individual brainstem structures initiates processes leading to cerebral vasodilation and an increase in volumetric cerebral blood flow [15, 16]. It is assumed that the brainstem may be directly involved in the generation of waves characteristic of intracranial hypertension, but the anatomical pathways and mechanisms of this influence are still not well understood. A number of experimental studies have shown the effect of stimulation of individual structures of the brainstem (including the locus coeruleus - locus coeruleus) of the reticular formation of the medulla oblongata and hemispheric structures of the brain (in particular, the anterior cingulate gyrus and anterior parts of the hypothalamus) on changes in ICP [17]. It was also previously shown that damage to brain stem structures and frontal lobes during TBI can lead to changes in the activity of the sympathetic nervous system, affecting arterial tone [18].
A feature of DAP is the predominant damage to the subcortical and stem structures of the brain involved in maintaining vital functions, including the regulation of cerebral vascular tone and BUN.
The purpose of this work is to identify anatomical damage to deep brain structures that influence the degree and duration of BUN disturbances in the acute period of severe DAP.
Material and methods
The analysis included 37 patients with mTBI (3-8 points on the Glasgow Coma Scale) who were treated in the intensive care unit of the National Medical Research Center for Neurosurgery named after. N.N. Burdenko in the period from 2009 to 2014. The inclusion criteria were met by patients who, according to clinical indications, required monitoring of blood pressure, ICP, CPP and in whom MRI of the brain revealed signs of DAP. Monitoring data was stored, analyzed and calculated using ICM Plus software. In total, the analysis included 23 men and 12 women, whose average age was 28±12.4 years. Seven patients in this group underwent decompressive craniotomy due to diffuse cerebral edema.
In the intensive care unit, patients were given mechanical ventilation, PaCO2 was maintained at 35-45 mm Hg, PaO2 was not lower than 100 mm Hg, sedation and analgesia were administered (propofol 1-3 mg/kg/h or midazolam 10-30 mcg/kg/h, fentanyl 1-2 mcg/kg/h). CPP was maintained above 60 mm Hg. When ICP is above 20 mm Hg. bolus administration of 15% mannitol (0.25-1 g/kg) or Hyperhaes at a dose of 2-3 ml/kg was used.
The Glasgow Coma Scale (GCS) was used to assess the depth of coma [19, 20]. TBI outcomes were assessed using the Glasgow Outcome Scale (GOS) [20, 21]. Brain damage in DAP was assessed using a classification based on MRI data [22]. The location and level of brain damage were assessed using the MRI classification proposed by N.E. Zakharova et al. [23].
All patients underwent ICP monitoring in accordance with international recommendations and the protocol of the Association of Neurosurgeons of the Russian Federation [7, 24]. ICP monitoring was carried out using a Codman ICP Express Monitor and a Codman MicroSensor (Jonson & Johnson Professional, Inc., Raynham, USA). The ICP sensor was implanted into the white matter of the brain through the trefination foramen in the projection of Kocher's point into the premotor zone of the subdominant hemisphere. BUN was assessed by monitoring the cerebral vascular reactivity index PRx [10]. The average duration of PRx monitoring was 7 days. The ratio of the duration of the period of impaired autoregulation to the total duration of monitoring of this parameter was also assessed.
BP monitoring was performed using direct measurement through an arterial catheter placed in the radial, femoral, or dorsalis pedis arteries.
Based on the calculation of the average PRx coefficient for the entire observation period when monitoring ICP and CPP, two groups of patients were identified:
Group 1 - with preserved AUB - PRx [–1; 0];
Group 2 - with partially or completely lost AUB - PRx (0; 1].
The characteristics of patients in each group are presented in Table. 1.
Group 1 consisted of 19 patients. In 16 (84.2%) of them, the cause of injury was a traffic accident. Brain stem damage was diagnosed in 15 (78.9%) patients during MRI. Group 2 was represented by 18 patients. In 15 of them, the cause of injury was a traffic accident. Seven patients underwent decompressive trepanation due to diffuse cerebral edema. In 15 (83.3%) patients in this group, brain stem damage was visualized during MRI.
Neuroimaging methods. MRI of the brain was performed on a 3 T GE tomograph in standard modes (T1, T2, FLAIR) and SWI/T2* GRE, DWI modes, which made it possible to evaluate both ischemic and small hemorrhagic focal lesions. In each patient, according to MRI data, damage to individual subcortical structures and areas of the brain stem, which are projections of the main neurotransmitter systems of the brain, was assessed (Fig. 1),
as well as areas of damage to the frontal lobes (mediobasal, pole and dorsolateral sections). Statistical methods. Data processing was carried out in the Statistica 8.0 software package. (StatSoft Inc, USA). In all cases, nonparametric tests were used for statistical evaluation. To analyze qualitative characteristics, Fisher's test (F) was used; odds ratios, sensitivity and specificity of each factor were calculated to assess the influence of anatomical factors on the risk of developing unstable hemodynamics. Results were considered statistically significant at p < 0.05.
results
MRI analysis data showed that all patients in the analyzed sample had signs of diffuse brain damage involving the hemispheric and in 29 (78.4%) of 37 patients - brainstem structures. At the same time, the small number of patients in the groups with intact and impaired autoregulation did not allow us to identify significant differences in the outcomes according to the GOS severity of injury according to the GCS. The groups did not differ from each other in gender and age characteristics. Localization and depth of brain damage assessed according to the classifications of R. Firsching et al. [22] and N.E. Zakharova et al. [23], also did not differ significantly between the comparison groups (see Table 1).
Prevalence of damage to brain stem and subcortical structures in impaired AMB
Next, a statistical analysis was carried out on the frequency of occurrence of unilateral or bilateral damage to each brain structure in patients with impaired (group 2) and intact (group 1) autoregulation (Table 2).
Statistical analysis of the data showed that in patients with traumatic brain injury, accompanied by disturbances of the AMB in the acute period of injury, in general, damage to the brainstem was observed somewhat more often than in the group of patients with normal autoregulation. Among the studied brainstem structures, significantly more often (p = 0.02) in patients of group 2 there was structural damage to the substantia nigra of the midbrain - a structure that is the source of dopaminergic projections for the neostriatum, cingulate cortex, olfactory nuclei, posterior hypothalamus and tonsils of the brain. The odds ratio was 5.333 (95% CI 1.252, 29.346), sensitivity 62.5% and specificity 76.2%. Also, more frequent damage to the cholinergic structure - the area of Meynert's nucleus - was revealed in patients with impaired autoregulation (p = 0.01), and unilateral or bilateral damage to this area of the brain had a fairly high specificity (81%) for patients in this group. Additionally, the incidence of combined damage to the substantia nigra and Meynert's nucleus was assessed, which significantly prevailed in the group with impaired autoregulation (p = 0.02). The odds ratio was 7.39 (95% CI 1.043, 65.37), sensitivity 43.8% and specificity 90.5%.
Thus, the analysis showed that impaired autoregulation of cerebral blood flow in patients with brain DAP is often associated with the presence of primary damage to the substantia nigra, the area of Meynert’s nucleus, and their combination (Fig. 2).
Prevalence of damage to subcortical and brain stem structures in long-term autoregulation disorders
To analyze the effect of damage to the subcortical and stem structures of the brain on the parameter of autoregulation of blood flow (PRx), patients were divided into three approximately equal groups depending on the duration of the period of lost autoregulation (PRx>0.2) relative to the entire measurement time: 1) less than 20% time (n=17); 2) 20-34% of the time (n=10); 3) 35% of the time or more (n=10). The results of this analysis are presented in table. 3.
It was found that in patients with lost autoregulation more than 35% of the measurement time, trunk damage was somewhat more likely to be present. In this group of patients, injuries to the substantia nigra were significantly more common (p=0.05). The odds ratio was 5.6 (95% CI 0.785, 45.938), sensitivity and specificity were 70 and 70.6%, respectively. Also in this group, more frequent damage to the Meynert nucleus region was noted (p = 0.04). The odds ratio was 7.6 (95% CI 1.006, 68.466), sensitivity and specificity were 70 and 76.5%, respectively.
According to the results of this analysis, significant differences remained in the frequency of damage to the substantia nigra, the area of the Meynert nucleus and their combination between extreme groups (with the duration of impaired autoregulation less than 20% and more than 35% of the measurement time). Thus, the presence of primary damage to the brainstem in the area of the substantia nigra and basal forebrain (Meynert's nucleus area) makes a significant contribution to the disruption of the AUB mechanisms.
Discussion
Our proposed hypothesis about the influence of certain neurotransmitter structures of the brain as central links on AMB in severe brain injury has not previously been covered in the literature. The data we obtained on the DAP model can be explained by the previously accumulated results of studying other human brain diseases (mainly neurodegenerative) and previous experimental work.
It has now been proven that many neurotransmitter systems can influence blood flow through receptors located on capillaries or perivascular glia. Such effects, in particular, are shown for dopamine, which has two types of receptors: D1- and D2-like receptors, the first of which have vasorelaxing effects, and the second - vasoconstrictor effects. Dopamine in humans has a constricting effect on large cerebral arteries and thereby increases the linear velocity of cerebral blood flow [26].
The substantia nigra functionally belongs to the extrapyramidal system, since it is involved in the regulation of muscle tone while ensuring motor functions. The least known and studied are the anatomical pathways through which it affects autonomic functions: breathing, cardiac activity and vascular tone. The substantia nigra contains two types of neurons, some of which use dopamine (pars compacta), and others (pars reticulata) use glutamate. A number of experimental studies have shown that electrical stimulation of the substantia nigra pars compacta causes tachycardia and increased blood pressure [25, 27-29]. Such data indicate that dopaminergic neurons of the substantia nigra activate the central pathway of the cardiovascular depressor center, through which inhibition of sympathetic fibers occurs, causing constriction of the arteries and increased heart rate.
Dopaminergic neurons in the substantia nigra send projections to the basal forebrain system, called the extended amygdala. The “extended amygdala” is closely associated with forebrain and brainstem structures involved in the regulation of the cardiovascular system [29, 30]. Stimulation of its structures, as well as stimulation of the substantia nigra, leads to the suppression of cardiovascular reactions [31, 32], which makes it possible to combine them into a single regulatory system. Previous studies have shown that the activity of dopaminergic neurons in the substantia nigra can be regulated by arterial baroreceptors [33, 34]. Denervation of baroreceptors leads to decreased production and release of dopamine into the striatum. These data point to the important fact that dopaminergic neurons of the substantia nigra may be part of a long central baroreceptor reflex pathway that regulates blood pressure [35].
There is evidence that cholinergic neurons are also involved in the regulation of regional cerebral blood flow [36, 37], and this regulatory mechanism does not depend on regional metabolism and systemic blood pressure. Activation of cholinergic fibers of the Meynert nucleus and septal complex leads to the release of acetylcholine in the cortex and hippocampus, which provokes an increase in cerebral blood flow in these structures. A diffuse increase in blood flow in the cortex during walking is associated with excitation of the vasodilatory system of the basal nucleus of Meynert [36]. Activation of cholinergic neurons in the basal forebrain may contribute to increased ICP and the formation of plateau waves due to vasodilation [17].
It is known that in a number of neurodegenerative diseases of the brain (Parkinson’s disease, multiple system atrophy), autoregulation disorders are also observed, which is associated with autonomic dysfunction [38]. However, each link of the autonomic system has its own representation in the central nervous system, in particular in the brain stem. A clinical model for understanding the role of the substantia nigra in regulating blood flow is Parkinson's disease, a disease characterized by the progressive loss of dopaminergic neurons in the substantia nigra. Experimental studies modeling this disease indicate a weakening of the sympathetic component of the regulation of blood pressure and heart rate during degeneration of the substantia nigra [39].
Thus, this work shows that damage to the dopaminergic structure of the substantia nigra and the cholinergic structure of the Meynert nucleus area in patients with DAP is associated with a more pronounced and long-lasting impairment of the autoregulation of cerebral blood flow. The data obtained indicate the existence in humans of neurogenic mechanisms regulating cerebral vascular tone that contribute to changes in ICP. Damage to these regulatory links as a result of injury is associated with a more severe and prolonged period of impaired autoregulation of cerebral blood flow, which may require longer monitoring and correction of ICP.
The results of the work show the presence of different patterns of brain damage in patients with impaired and intact mechanisms of cerebral autoregulation with the same severity and clinical form of TBI. Our data, from the clinical side, indirectly confirm the results of previously conducted experimental studies regarding the presence of direct neuronal mechanisms for regulating vascular tone. However, these data should be interpreted with caution; they are preliminary and only lift the curtain on the complex mechanisms of regulation of cerebral blood flow in acute brain pathology. Of course, further, more detailed research in this direction is needed, including to identify all parts of the neuronal regulatory system.
The work was supported by the Russian Foundation for Basic Research grant No. 16−04−01472.
The authors declare no conflict of interest.
A comment
The 1960-1970s were marked by intensive study of cerebral circulation and autoregulation of cerebral blood flow (BF). Morphological studies made it possible to detect nerve fibers in the walls of cerebral vessels from the circle of Willis and its branches to the smallest arterioles. Nerve cells, fibers and receptors were identified in the connective tissue strings that stabilize the arteries in the cerebrospinal fluid channels of the subarachnoid space. The main arteries are richly innervated, the nervous apparatus in the area of the siphon of the internal carotid artery is especially developed. No one doubts the presence of nervous regulation of cerebral circulation. However, the mechanisms of this regulation remain unclear. First of all, the nature of the central mechanisms involved in the regulation of the lumen of cerebral vessels is unclear. Some suggest that the function of such a regulatory center can be performed by neurons or their groups, which are located in the cortex itself, near the effector arteries; others look for this center in the reticular formation, tent nuclei and hypothalamus.
The authors conducted a study of BUN in 37 patients with cerebral DAP using monitoring of the cerebral vascular reactivity coefficient. They divided all patients into two groups comparable in other indicators: with preserved (19 patients) and with partially or completely lost AUB (18). MRI revealed in both groups 15 patients with damage to brain stem structures. Statistical analysis using a modern software package found that brain damage in the projections of the dopaminergic structure of the substantia nigra and the cholinergic structure in the zone of the substantia innominata of Meynert’s nucleus was significantly more common in patients with impaired AMB. The revealed pattern is not only of theoretical interest, but of great practical importance.
It is known that damage to the substantia nigra and Meynert's nucleus is pathognomonic for Parkinson's disease. AUB disorders could explain the worsening of the condition of patients after surgical treatment complicated by pneumocephalus. Recent studies have confirmed changes in autoregulation in idiopathic parkinsonism. However, these are not necessarily AUB disorders. It is likely that the central mechanisms of AUB are much more complex than just their localization in the brain structures indicated by the authors.
The problem raised in this article certainly requires further more detailed study. The results of the work carried out by the authors deserve to be published.
A.L. Krivoshapkin (Moscow)
Bibliography:
- Zweifel S, Dias S, Smielewski P, Czosnyka M. Continuous time-domain monitoring of cerebral autoregulation in neurocritical care. Medical Engineering and Physics. 2014 1 May;36: Issue 5:638-645. https://doi.org/10.1016/j.medengphy.2014.03.002
- Lassen N.A. Cerebral blood flow and oxygen consumption in man. Physiol Rev. 1959;39:183-238.
- Johnson U, Nilsson P, Ronne-Engström E, Howells T, Enblad P. Favorable outcome in traumatic brain injury patients with impaired cerebral pressure autoregulation when treated at low cerebral perfusion pressure levels. Neurosurgery. 2011;68:714-722. https://doi.org/10.1227/neu.0b013e3182077313
- Attwell D, Buchan AM, Charpak S, Lauritzen M, Macvicar BA, Newman EA. Glial and neuronal control of brain blood flow. Nature. 2010;468:232-243. https://doi.org/10.1038/nature09613
- Betz E. Cerebral blood flow: Its measurement and regulation. Physiol Rev. 1972;52:595-630. https://doi.org/10.1152/physrev.1972.52.3.595
- Bor-Seng-Shu E, Kitaw S, Figueiredo EG, Paiva wS, Fonoff ET, Teixeira MJ, Panerai RB. Cerebral hemodynamics: concepts of clinical Importance. Arq Neuropsiquiatr. 2012;70(5):357-365. https://doi.org/10.1590/s0004-282×2012000500010
- Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, Manley GT, Nemecek A, Newell DW, Rosenthal G, Schouten J, Shutter L, Timmons SD, Ullman JS, Videtta W, Wilberger JE, Wright D.W. Guidelines for the management of severe traumatic brain injury. VII. Intracranial pressure monitoring technology. J Neurotrauma. 2007;24(Suppl 1):S45-S54. https://doi.org/10.1089/neu.2007.9990
- Lundberg N. Continuous recording and control of ventricular fluid pressure in neurosurgical practice. Acta Psychiatr Neural Scand. 1960;36(Suppl 149):1-193. https://doi.org/10.1097/00005072-196207000-00018
- Risberg J, Lundberg N, lngvar DH. Regional cerebral blood volume during acute transient rises of the intracranial pressure (plateau waves). J Neurosurg. 1969;31:303-310. https://doi.org/10.3171/jns.1969.31.3.0303
- Szosnyka M, Smielewski P, Kirkpatrick P, Laing RJ, Menon D, Pickard JD. Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurgery. 1997;41:11-17. https://doi.org/10.1097/00006123-199707000-00005
- Oshorov A.V., Savin I.A., Goryachev A.S., Popugaev K.A., Potapov A.A., Gavrilov A.G. The first experience of using monitoring of autoregulation of cerebral vessels in the acute period of severe traumatic brain injury. Anesthesiology and resuscitation. 2008;2:61-67. https://doi.org/10.14412/1995-4484-2008-8
- Oshorov A.V., Savin I.A., Goryachev A.S., Popugaev K.A., Polupan A.A., Sychev A.A., Gavrilov A.G., Kravchuk A.D., Zakharova N. E.E., Danilov G.V., Potapov A.A. Plateau waves of intracranial pressure in victims with severe traumatic brain injury. Anesthesiology and resuscitation. 2013;4:44-50. 13.Obrador S, Pi-Suiier j. Experimental swelling of the brain. Arch Neural Psychiatry. 1943;49:826-830. https://doi.org/10.1001/archneurpsyc.1943.02290180050005
- Ishii S. Brain swelling. Studies of structural, physiological and biochemical alterations. In: Caveness WH, Walker AF, eds. Head Injury Conference Proceedings. Philadelphia: Lippincott, 1966;276-299.
- Meyer JS, Teraura T, Sakamoto K, Kondo A. Central neurogenic control of cerebral blood flow. Neurology. 1971;21:247-262. https://doi.org/10.1212/wnl.21.3.247
- Ladecola C, Nakai M, Arbit E, Reis D. Global cerebral vasodilation elicited by focal electrical stimulation within the dorsal medullary reticular formation in anesthetized rat. J Cereb Blood Flow Metab. 1983;3:270-279. https://doi.org/10.1038/jcbfm.1983.41
- Maeda M, Matsuura S, Tanaka K, Katsuyama J, Nakamura T, Sakamoto H, Nishimura S. Effects of electrical stimulation on intracranial pressure and systemic arterial blood pressure in cats. Part I: Stimulation of the brain stem. Neurol Res. 1988a Jun;10(2):87-92. https://doi.org/10.1080/01616412.1988.11739821
- Aleksandrova E.V., Tonoyan A.S., Sychev A.A., Kryukova K.K. Activity of the sympatho-adrenal system in the acute period of severe traumatic brain injury: the significance of neuroanatomical factors. Bulletin of the Russian Foundation for Basic Research. 2016;2(90):41-49. https://doi.org/10.22204/2410-4639-2016-090-02-41-49
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974 Jul 13;2(7872):81-84. https://doi.org/10.1016/S0140-6736(74)91639-0
- Jennett B, Plum F. Persistent vegetative state after brain damage: A syndrome in search of a name. Lancet. 1972;1:734-737. https://doi.org/10.1016/S0140-6736(72)90242-5
- Firsching R, Woischneck D, Klein S, Reissberg S, Döhring W, Peters B. Classification of severe head injury based on magnetic resonance imaging. Acta Neurochir (Wien). 2001;143:263. https://doi.org/10.1007/s007010170106
- Zakharova N.E., Potapov A.A., Kornienko V.N., Pronin I.N., Alexandrova E.V., Danilov G.V., Gavrilov A.G., Zaitsev O.S., Kravchuk A. .D., Sychev A.A. New classification of traumatic brain injuries based on magnetic resonance imaging data. Bulletin of the Russian Foundation for Basic Research. 2016;2(90):12-19. https://doi.org/10.22204/2410-4639-2016-090-02-12-19
- Potapov A.A., Krylov V.V., Gavrilov A.G., Kravchuk A.D., Likhterman L.B., Petrikov S.S., Talypov A.E., Zakharova N.E., Oshorov A. .V., Sychev A.A., Aleksandrova E.V., Solodov A.A. Recommendations for the diagnosis and treatment of severe traumatic brain injury. Part 3. Surgical treatment (options). Issues of neurosurgery named after. N.N. Burdenko. 2016;2:93-101.https://doi.org/10.17116/neiro201680293-101
- Potapov A.A., Krylov V.V., Gavrilov A.G., Kravchuk A.D., Likhterman L.B., Petrikov S.S., Talypov A.E., Zakharova N.E., Oshorov A. .V., Sychev A.A., Aleksandrova E.V., Solodov A.A. Recommendations for the diagnosis and treatment of severe traumatic brain injury. Part 2. Intensive care and neuromonitoring. Issues of neurosurgery named after. N.N. Burdenko. 2016;80(1):98-106. https://doi.org/10.17116/neiro201680198-106
- Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS, Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, Manley GT, Nemecek A, Newell DW, Rosenthal G, Schouten J, Shutter L, Timmons SD, Ullman JS, Videtta W, Wilberger JE, Wright DW. Guidelines for the management of severe traumatic brain injury. VII. Intracranial pressure monitoring technology. J Neurotrauma. 2007;24 Suppl 1:S45-S54. https://doi.org/10.1089/neu.2007.9989
- Niimi T, Sawada T, Kuriyama Y, The effect of dopamine on cerebral circulation and metabolism in man. Jpn J Stroke. 1981;3:318-325.
- Ångyán L. Role of the substantia nigra in the behavioral-cardiovascular integration in the cat. Acta Physiol Scand. 1989;74:175-187.
- Lin MT, Yang JJ. Stimulation of the nigrostriatal dopamine system produces hypertension and tachycardia in rats. Am J Physiol. 1994 Jun;266(6 Pt 2):H2489-H2496. https://doi.org/10.1152/ajpheart.1994.266.6.H2489
- Dampney RAL. Functional organization of central pathways regulating the cardiovascular system. Physiol Rev. 1994;74:323-364. https://doi.org/10.1152/physrev.1994.74.2.323
- Sun MK. Central neural organization and control of the sympathetic nervous system in mammals. Prog Neurobiol. 1995;47:157-233. https://doi.org/10.1016/0301-0082(95)00026-8
- Ciriello J, Janssen SA. Effect of glutamate stimulation of the bed nucleus of the stria terminalis on arterial pressure and heart rate. Am J Physiol. 1993;265 (Heart Circ Physiol. 34): H1516-H1522. https://doi.org/10.1152/ajpheart.1993.265.5.H1516
- Roder S, Ciriello J. Contribution of the bed nucleus of the stria terminalis to the cardiovascular responses elicited by stimulation of the amygdala. J Auton Nerv Syst. 1993;45:61-75. https://doi.org/10.1016/0165-1838(93)90362-X
- Alexander N, Hirata Y, Nagatsu T. Reduced tyrosine hydroxylase activity in the nigrostriatal system of sinoaortic-denervated rats. Brain Res. 1984;299:380-382. https://doi.org/10.1016/0006-8993(84)90724-8
- Alexander N, Nakahara D, Ozaki N, Kaneda N, Sasaoka T, Iwata N, Nagatsu T. Striatal dopamine release and metabolism in sinoaortic-denervated rats by in vivo microdialysis. Am J Physiol. 1988;254. (Regulatory Integrative Comp Physiol. 1988;23):R396-R399. https://doi.org/10.1152/ajpregu.1988.254.2.R396
- Kirouac GJ, Ciriello J. Cardiovascular depressor responses to stimulation of substantia nigra and ventral tegmental area. Am J Physiol. 1997 Dec;273(6 Pt 2):H2549-H2557. https://doi.org/10.1152/ajpheart.1997.273.6.H2549
- Sato A, Sato Y, Uchida S. Regulation of regional cerebral blood flow by cholinergic fibers originating in the basal forebrain. Int J Dev Neurosci. 2001 Jun;19(3):327-337. Review. https://doi.org/10.1016/S0736-5748(01)00017-X
- Maeda M, Miyazaki M. Control of ICP and the cerebrovascular bed by the cholinergic basal forebrain. Acta Neurochir Suppl. 1998;71:293-296. https://doi.org/10.1007/978-3-7091-6475-4_85
- Gregor K. Wenning, Carlo Colosimo, Felix Geser and Werner Poewe. Multiple system atrophy. Lancet Neurology. 2004;3:93-103. https://doi.org/10.1016/S1474-4422(03)00662-8
- Ariza D, Sisdeli L, Crestani CC, Fazan R, Martins-Pinge MC. Dysautonomias in Parkinson's disease: cardiovascular changes and autonomic modulation in conscious rats after infusion of bilateral 6-OHDA in substantia nigra. Am J Physiol Heart Circ Physiol. 2015 Feb 1;308(3):H250-H257. https://doi.org/10.1152/ajpheart.00406.2014
Discussion
Our proposed hypothesis about the influence of certain neurotransmitter structures of the brain as central links on AMB in severe brain injury has not previously been covered in the literature. The data we obtained on the DAP model can be explained by the previously accumulated results of studying other human brain diseases (mainly neurodegenerative) and previous experimental work.
It has now been proven that many neurotransmitter systems can influence blood flow through receptors located on capillaries or perivascular glia. Such effects, in particular, are shown for dopamine, which has two types of receptors: D1- and D2-like receptors, the first of which have vasorelaxing effects, and the second - vasoconstrictor effects. Dopamine in humans has a constricting effect on large cerebral arteries and thereby increases the linear velocity of cerebral blood flow [26].
The substantia nigra functionally belongs to the extrapyramidal system, since it is involved in the regulation of muscle tone while ensuring motor functions. The least known and studied are the anatomical pathways through which it affects autonomic functions: breathing, cardiac activity and vascular tone. The substantia nigra contains two types of neurons, one of which uses dopamine ( pars compacta
), and others (
pars reticulata
) - glutamate.
A number of experimental studies have shown that electrical stimulation pars compacta
causes tachycardia and increased blood pressure [25, 27-29]. Such data indicate that dopaminergic neurons of the substantia nigra activate the central pathway of the cardiovascular depressor center, through which inhibition of sympathetic fibers occurs, causing constriction of the arteries and increased heart rate.
Dopaminergic neurons in the substantia nigra send projections to the basal forebrain system, called the extended amygdala. The “extended amygdala” is closely associated with forebrain and brainstem structures involved in the regulation of the cardiovascular system [29, 30]. Stimulation of its structures, as well as stimulation of the substantia nigra, leads to the suppression of cardiovascular reactions [31, 32], which makes it possible to combine them into a single regulatory system. Previous studies have shown that the activity of dopaminergic neurons in the substantia nigra can be regulated by arterial baroreceptors [33, 34]. Denervation of baroreceptors leads to decreased production and release of dopamine into the striatum. These data point to the important fact that dopaminergic neurons of the substantia nigra may be part of a long central baroreceptor reflex pathway that regulates blood pressure [35].
There is evidence that cholinergic neurons are also involved in the regulation of regional cerebral blood flow [36, 37], and this regulatory mechanism does not depend on regional metabolism and systemic blood pressure. Activation of cholinergic fibers of the Meynert nucleus and septal complex leads to the release of acetylcholine in the cortex and hippocampus, which provokes an increase in cerebral blood flow in these structures. A diffuse increase in blood flow in the cortex during walking is associated with excitation of the vasodilatory system of the basal nucleus of Meynert [36]. Activation of cholinergic neurons in the basal forebrain may contribute to increased ICP and the formation of plateau waves due to vasodilation [17].
It is known that in a number of neurodegenerative diseases of the brain (Parkinson’s disease, multiple system atrophy), autoregulation disorders are also observed, which is associated with autonomic dysfunction [38]. However, each link of the autonomic system has its own representation in the central nervous system, in particular in the brain stem. A clinical model for understanding the role of the substantia nigra in regulating blood flow is Parkinson's disease, a disease characterized by the progressive loss of dopaminergic neurons in the substantia nigra. Experimental studies modeling this disease indicate a weakening of the sympathetic component of the regulation of blood pressure and heart rate during degeneration of the substantia nigra [39].
Thus, this work shows that damage to the dopaminergic structure of the substantia nigra and the cholinergic structure of the Meynert nucleus area in patients with DAP is associated with a more pronounced and long-lasting impairment of the autoregulation of cerebral blood flow. The data obtained indicate the existence in humans of neurogenic mechanisms regulating cerebral vascular tone that contribute to changes in ICP. Damage to these regulatory links as a result of injury is associated with a more severe and prolonged period of impaired autoregulation of cerebral blood flow, which may require longer monitoring and correction of ICP.
The results of the work show the presence of different patterns of brain damage in patients with impaired and intact mechanisms of cerebral autoregulation with the same severity and clinical form of TBI. Our data, from the clinical side, indirectly confirm the results of previously conducted experimental studies regarding the presence of direct neuronal mechanisms for regulating vascular tone. However, these data should be interpreted with caution; they are preliminary and only lift the curtain on the complex mechanisms of regulation of cerebral blood flow in acute brain pathology. Of course, further, more detailed research in this direction is needed, including to identify all parts of the neuronal regulatory system.
The work was supported by the Russian Foundation for Basic Research grant No. 16−04−01472.
The authors declare no conflict of interest.
CEREBRAL CIRCULATION INSUFFICIENCY OF VASCULAR GENESIS
Preferanskaya Nina Germanovna Associate Professor, Department of Pharmacology, Educational Department, Institute of Pharmacy and Translational Medicine, Multidisciplinary Center for Clinical and Medical Research, International School “Medicine of the Future”, First Moscow State Medical University. THEM. Sechenov (Sechenov University), Ph.D.
Divaza (tablet for resorption No. 100) is an innovative combination drug containing affinity-purified antibodies to the brain-specific protein S-100 and affinity-purified antibodies to endothelial NO synthase. Antibodies to the brain-specific protein S-100 have antioxidant, antihypoxic, neuroprotective, and anxiolytic effects. The combined use of the components of the drug is accompanied by an increase in the neuroprotective activity of antibodies to the S-100 protein, an increase in the vegetative-stabilizing effect, normalization of the vegetative status, a synergistic effect of both components on neuronal plasticity and, as a result, an increase in the brain’s resistance to toxic influences.
The use of the drug improves integrative activity and restores interhemispheric connections of the brain, helps eliminate cognitive impairment, stimulates reparative processes and accelerates the restoration of central nervous system functions, increases mental performance, restores learning and memory processes, normalizes somatovegetative manifestations, and increases cerebral blood flow. The drug does not have a sedative or muscle relaxant effect, and does not cause addiction or addiction.
Divaza is used to restore integrative brain activity in a wide range of organic disorders of the central nervous system caused by neurodegenerative, cerebrovascular diseases, neuroinfections, and traumatic brain injury. Used as part of complex therapy. Individual hypersensitivity reactions to the components of the drug are possible.
1 tablet of the drug contains affinity-purified antibodies to the brain-specific protein S-100 - 0.006 g and affinity-purified antibodies to endothelial NO synthase - 0.006 g.
Instenon is a combination drug containing etamivan, hexobendine and etophylline . The neuroprotective effect of the drug is based on mutual potentiation of effects. The drug selectively stimulates brain metabolism, stabilizes cerebral and systemic circulation, slows down the death of brain neuron cells, moderately dilates coronary and cerebral vessels, increases the utilization of glucose and oxygen by brain cells. When using the drug, performance increases, fatigue, headaches decrease, mood and general tone improve.
The drug is prescribed to patients with acute and chronic forms of vascular pathology of the brain, consequences of a stroke, 2 ml IM or IV, after dissolving it in 200 ml of 5% glucose, 1-2 times a day.
Use 1-2 tablets orally. 3 times a day, without chewing, if necessary, increase the dose to 5 tablets.
Available: table, cover. obol. (50 mg etamivan + 20 mg hexobendine dihydrochloride + 60 mg etophylline); table forte (100 mg etamivan + 60 mg hexobendine + 60 mg etophylline); solution for injection, amp. 2 ml (50, 10 and 100 mg respectively).
Important! The most common side effects are decreased blood pressure, headache, and short-term tachycardia.
Piracetam + Cinnarizine (“ Omaron ”, tab., “ Combitropil ”, caps., “ Pyracesin ”, caps.) is a combination drug ( piracetam 400 mg + cinnarizine 25 mg ). Both components mutually potentiate their actions: antihypoxic, reduce cerebral vascular resistance and improve cerebral metabolism, and contribute to a significant increase in cerebral blood flow. The combined drug is quickly and completely absorbed from the gastrointestinal tract. The therapeutic effect appears after 1–6 hours.
Indications for use are various cerebrovascular accidents; for the prevention of migraines, to improve learning and memory of children with intellectual retardation. The usual dose for adults is 1-2 caps. 3 times a day for 1–3 months, depending on the severity of the disease. Repeat the course 2-3 times a year. Children from 5 years of age are prescribed 1-2 capsules 1-2 times a day.
Vinpocetine + Nootropil ( Vinpotropil , capsule, tablet, coating, concentrate d/injection solution) is a combination drug ( vinpocetine 5 mg + piracetam 400 mg ). The action is due to the components included in the composition, the effect develops gradually. Vinpocetine is a vasodilator that improves cerebral circulation; as a cerebrovasodilator, it improves cerebral circulation, causes a slight decrease in systemic blood pressure, dilation of cerebral vessels, increased blood flow and improved supply of oxygen and glucose to the brain; increases the resistance of brain cells to hypoxia, facilitating oxygen transport.
Piracetam as a nootropic agent has a positive effect on the metabolic processes of the brain, increases the concentration of ACE in brain tissue, enhances the synthesis of RNA and phospholipids, stimulates glycolytic processes, enhances glucose utilization; improves the integrative function of the brain.
Adults and adolescents over 14 years of age are prescribed orally, before meals, 1-2 caps. 3 times a day. Maintenance dose - 1 capsule 3 times a day. The course of treatment is from 2–3 weeks to 2–6 months. Before discontinuing the drug, the dose is reduced gradually.
PREPARATIONS OF ANIMAL ORIGIN
Cerebrolysin (injection solution, 1, 5 and 10 ml, amp.) is a product of hydrolysis of pig brain substance (1 ml of aqueous solution of the drug contains 0.2152 g of Cerebrolysin ). It is a clear, amber-colored liquid that contains low molecular weight neuropeptides (15%) and about 18 biologically active amino acids (85%). Active amino acids and peptides easily penetrate from the blood into neurons, exerting an organ-specific complex effect on the brain. The drug provides neuroprotection, functional neuromodulation, as well as regulation of metabolism, increases the efficiency of aerobic energy metabolism in brain tissue, improves oxygen utilization, protein synthesis in brain neurons, reduces the harmful effects of lactic acidosis, and stimulates transsynaptic transmission. The neuroprotective effect of Cerebrolysin is to increase the resistance of brain tissue to hypoglycemia, intoxication, hypoxia and other damaging influences.
It has been established that the drug has an antioxidant effect, inhibits the process of free radical oxidation, and has a positive effect on the homeostasis of antioxidant microelements (selenium, magnesium, potassium, manganese).
The drug is prescribed for ischemic stroke, cerebral atherosclerosis, complications after neurosurgical operations and traumatic brain injuries - from 10 to 50 ml is administered daily through very slow intravenous infusions with preliminary dilution with special solutions for infusions (Ringer's solution, dextrose solution). The duration of infusions is from 15 minutes. up to an hour. Duration of therapy is 10–20 days. If necessary, the course of treatment should be repeated, reducing the frequency of injections to 2-3 times a week. Contraindication is hypersensitivity to any component of the drug.
Actovegin (4% solution for injection, amp. 2, 5, 10 ml; solution for infusion, vial 250 ml; dragee forte 200 mg; tablet, coating volume, 200 mg) - a drug containing deproteinized homoderivative from calf blood serum with low molecular weight peptides, amino acids, nucleosides and intermediate products of carbohydrate and lipid metabolism. Actovegin activates metabolism in brain tissue, improves trophism and stimulates regeneration processes.
The drug is used for metabolic and circulatory disorders in the central nervous system, cerebrovascular accidents, encephalopathies, traumatic brain injuries and strokes. When using Actovegin, the pharmacological effect begins to appear no later than after 30 minutes. after parenteral administration or oral administration and reaches a maximum after an average of 3 hours. Parenteral administration of Actovegin should be carried out with caution due to the possible development of anaphylactic reactions.
Important! Side effects are mainly allergic reactions.
Cortexin (porous lyophilized 10 mg dosage solution for injection) is a complex of polypeptide fractions isolated from the cerebral cortex of cattle and pigs. The drug has a cerebroprotective and nootropic effect, restores bioelectrical activity and improves brain metabolism, regulates the ratio of inhibitory and excitatory amino acids, has a GABAergic effect, and has antioxidant activity. Cortexin is administered intramuscularly at a dose of 10 mg daily for 10 days. No side effects were identified during use.
PHYTOMEDICATIONS
Ginkgo biloba leaf extract is a herbal remedy. Produced under the trade names Bilobil forte, Ginkgo biloba, Ginos, Tanakan, etc.
The leaves contain biologically active substances - a sum of flavonoids ( quercetin, luteolin, kaempferol), terpene trilactones, gincolide, alkaloids, etc. The drug has antioxidant activity, prevents the formation of free radicals and lipid peroxidation of cell membranes, improves cerebral and peripheral circulation, strengthens the walls blood vessels, improves immunity, has an anti-inflammatory effect. Normalizes metabolic processes, has an antihypoxic effect on tissues. It has a pronounced anti-edematous effect both at the level of the brain and at the periphery. Affects the release, reuptake and catabolism of neurotransmitters (norepinephrine, dopamine, acetylcholine) and their ability to bind to membrane receptors. Ginkgo preparations have a wide range of applications, including encephalopathies of various origins (consequences of stroke, traumatic brain injury), and pathological processes that develop in old age, decreased intellectual abilities, sleep disturbances, and many others. etc. (see instructions).
Important! When used, allergic reactions (redness, swelling of the skin, itching), gastrointestinal disorders, headache, decreased blood clotting, hearing impairment, and dizziness are possible. There are reports of internal bleeding observed after long-term use of preparations based on Ginkgo biloba.
Tanakan is a preparation that contains 40 mg of dry standardized extract of Ginkgo biloba leaves, standardized, titrated in a quantitative volume: 24% Ginkgo heterosides and 6% Ginkgolides-Bilobalides. The effect of the drug is due to its influence on metabolic processes in cells, rheological properties of blood and microcirculation, as well as vasomotor reactions of blood vessels. The drug improves cerebral circulation and the supply of oxygen and glucose to the brain. It has a vasoregulatory effect on the entire vascular system: arteries, veins, capillaries. Helps improve blood flow, prevents red blood cell aggregation, and has an inhibitory effect on platelet activation factor.
Tanakan is prescribed 1 tablet. or 1 ml of solution for oral administration 3 times a day with meals (120 mg/day). When treating asthenic disorders, the optimal daily dose of the drug is 240 mg - 2 tablets each. or 2 ml oral solution 3 times a day. The duration of treatment is from 1 to 3 months.
Important! When using the drug, digestive disorders, allergic skin reactions, and headaches may occur.
Memoplant is a preparation containing 40 mg of dry standardized extract of Ginkgo biloba leaves, 9.6 mg of ginkgoflavone glycosides , 2.4 mg of terpene lactones and 0.2 μg of ginkgolic acid . The drug increases the body's resistance to hypoxia, especially brain tissue, inhibits the development of traumatic or toxic cerebral edema, improves cerebral and peripheral circulation, and has an inhibitory effect on platelet aggregation factor. Organic (arising as a result of age-related circulatory disorders) and functional disorders of the brain with such manifestations as memory impairment, decreased ability to concentrate and intellectual capabilities, dizziness, tinnitus, headache. Disorders of the inner ear, manifested by dizziness, unsteady gait and tinnitus.
Use the drug 1-2 tablets. 3 times a day. The duration of treatment is at least 8 weeks.
HOMEOPATHIC MEDICINES
Memoria (20, 50, 100 ml, bottle with drip dispenser) - 100 ml of the drug contains Hypericum D1 15 ml, Arnica D12 10 ml, Conium D6 10 ml, Ginkgo D6 10 ml, Panax D6 10 ml, ethyl alcohol 43% by weight. For the treatment of memory and concentration disorders, in the complex treatment of cerebral atherosclerosis, accompanied by headaches and dizziness. To ensure the greatest effectiveness, Memoria should be taken 30 minutes before. before or 1 hour after meals. At the onset of the disease, as well as in cases requiring rapid relief of symptoms, adults and adolescents can take 10 drops every half hour to hour, hold a little in the mouth before swallowing, take until the condition improves, but no more than 8 times, after which take 3 times a day. Since Memoria contains natural plant components, during storage there may be slight turbidity and a weakening of smell and taste, which does not lead to a decrease in the effectiveness of the drug.