General information
Poliomyelitis is a highly infectious viral disease primarily affecting young children and is caused by one of three serotypes of poliovirus (1,2 or 3). It affects the nervous system and can lead to general paralysis in a matter of hours. The virus is transmitted from person to person primarily through the fecal-oral route or, less commonly, through some common carrier of infection (for example, contaminated water or food) and multiplies in the intestines. Many infected people have no symptoms but shed the virus in their feces and can thus transmit the infection to others.
What should you do if an unvaccinated child came into contact with someone vaccinated against polio?
Indeed, what can happen to an unvaccinated baby, for example, in kindergarten when he comes into contact with a vaccinated OPV.
Yes, a vaccinated child releases pathogenic strains into the environment for some time. You need to understand that only virulent viruses pose a danger, and in order to become such, they must undergo a mutation in the intestines of the vaccinated person . This is possible if a person has a serious immunodeficiency, which in itself is a rare case.
Therefore, usually a vaccinated baby releases unchanged (non-dangerous) viruses in much smaller quantities (passive immunization) than they were injected with during immunization. That is, those around you who have received such a small dose simply maintain the tension of the immune system in the team.
This is the purpose of OPV vaccination. But even if we assume that an unvaccinated baby still managed to catch a virulent virus (that is, he also has severe immunodeficiency), the probability of contracting polio is only 5% (or less).
But, even if included in these statistics (which is absolutely incredible), the child is unlikely to get paralytic (which is what everyone is afraid of). The disease will go unnoticed or will be similar to ARVI or an intestinal infection.
And only 2% of children have a chance of getting vaccine-associated paralysis. But do not forget that such a baby has severe immunodeficiency. In addition, the contact must be long and close.
In a kindergarten setting, all of the above points are unlikely to coincide. Therefore, such cases were not recorded.
So, the maximum that can happen is that the child receives passive immunization. It should be remembered that this situation is only permissible with OPV vaccination, since no virus release occurs with IPV.
Chance of getting sick
Polio mainly affects children under 5 years of age. The disease still exists, although WHO estimates that since 1988, the number of polio cases has decreased by more than 99%, or from 350,000 to 359 cases reported in 2014 and further in 2015 to 73 cases. In 1988, the number of countries experiencing transmission of wild poliovirus (WPV) exceeded 125, in 2014 there were only 9, and in 2015 only 2 countries reported cases of polio caused by WPV (Afghanistan and Pakistan).
But as long as there is at least one infected child in the world, children in all countries are at risk of contracting polio.
How does infection occur and who is at risk?
The routes of infection with polio mainly come down to the penetration of the virus through the digestive tract - if water, food or hands have previously come into contact with contaminated substances. For example, feces of a sick person get into a pond, and then when swimming, the patient gets the virus along with the contaminated water. The causative agent of the disease is poliovirus.
You can become infected through water, food, dirty clothes, etc. At risk are:
- children under 7 years old. Poliomyelitis occurs much more often in children than in adults;
- Pregnant women;
- people with very weakened immune systems. This can be facilitated by various diseases, as well as disorders at the endocrine level, periods after operations, etc.;
- people suffering from immunodeficiencies.
The risk of infection is higher during the warm season: summer or autumn. The virus is very tenacious; in a humid environment it can live up to 4 months.
Symptoms and nature of the disease
The incubation period is usually 7-10 days (ranges from 4 to 35 days). The first symptoms are fever, fatigue, headache, vomiting and pain in the limbs.
Complications after an illness
Acute flaccid paralysis (usually of the legs) develops in one in 200 cases of infection. Persistent, irreversible paralysis and resulting deformities of the lower extremities are a common consequence of the disease.
Poliomyelitis is also dangerous due to other complications: pneumonia, pulmonary atelectasis, interstitial myocarditis; Sometimes acute dilation of the stomach and severe gastrointestinal disorders with bleeding, ulcers, and perforation develop.
Signs of infection after contact with a child who has been vaccinated
As mentioned earlier, if an infection occurs, then most likely the baby will experience it asymptomatically, or the negative manifestations will resemble a cold or intestinal infection.
But even if the worst thing happened, and the child fell ill with vaccine-associated paralysis (VAPP), this is not a death sentence.
The treated pathology (according to statistical data) leaves paralysis in only 25% of those who have recovered from the disease, and in more than 30% of cases it is cured without consequences.
How does polio manifest? Symptoms of this disease can be diagnosed at different time periods and directly depend on the route of infection. Typically, a vaccine recipient may develop signs of polio within 4-30 days after immunization.
However, if a child is infected through contact with a person vaccinated with a live vaccine, symptoms usually appear after two or three months. Interestingly, immunocompromised individuals may develop vaccine-associated polio after as long as six months.
Based on severity, doctors distinguish three main forms of VAPP:
- mild, passing after a month (abortive form);
- paralytic, causing the syndromes of the same name and increasing the fragility of bone tissue;
- and severe, capable of causing disability (muscle atrophy) or even death.
Symptoms of VAPP include:
- headache;
- increase in body temperature;
- muscle twitching;
- cough;
- pain in the back and limbs;
- rhinitis;
- insomnia (or vice versa, drowsiness);
- and dyspeptic disorders.
It should be noted that symptoms rarely last more than a month. But paralytic forms of VAPP are much more difficult for children to tolerate. Here the muscles of almost the entire body suffer greatly.
Vaccinated children are not dangerous to others. The exception is OPV vaccination. After this procedure, the patient releases viral strains into the environment for another 60 days. During this period, if there is close contact, an unvaccinated baby may become infected.
But if by this time he has already undergone 2-fold IPV vaccination, he will never get VAPP, which means he can safely contact people vaccinated with OPV. It should be remembered that a child can only get vaccine-associated polio if he has an immunodeficiency.
However, if there is even potential contact with a vaccinated OPV, the unvaccinated baby should be vaccinated.
If you refuse the procedure, be sure to separate the children for 2 months from the date of oral immunization.
Effectiveness of vaccination
In 1988, governments created the Global Polio Eradication Initiative (GPEI) to rid humanity of the disease forever. Following widespread use of the polio vaccine, the incidence of the disease fell sharply in many industrialized countries. Since 1988, the number of polio cases has decreased by more than 99%, from 350,000 to 73 cases reported in 2015, according to WHO.
Just 20 years ago, polio caused paralysis in 1,000 children every day. In 2010, 1,349 children were paralyzed. This decrease was the result of global efforts to eradicate the disease. In fact, this is the largest peacetime mobilization of people in history.
In 2014, only three countries in the world (Afghanistan, Nigeria and Pakistan) remained endemic for polio; in 2015, Nigeria was removed from this list, while in 1988 the number of such countries exceeded 125. Failure to eradicate polio in these remaining persistent foci could result in up to 200,000 new cases of the disease occurring annually worldwide within 10 years. The world can be freed from the threat of polio if everyone commits to it - from parents to government workers and from political leaders to the international community.
Live polio vaccine and an unvaccinated child: is there a risk of infection?
VAPP is diagnosed very rarely - one case per 500,000 - 2,000,000 doses. And this happens after the first injection. It has been established that with the second vaccination the frequency of this phenomenon is much less, and with the third it almost never occurs.
The chances of a healthy child getting infected from an injection are negligible. But is it possible to catch polio from someone who has already been vaccinated? Yes, theoretically.
Unvaccinated people suffering from immunodeficiency, pregnant women, and infants with pathologies of the immune system are susceptible to this threat. Therefore, caution should be exercised. In addition, if there are several children in a family, and one has already been vaccinated with OPV, then others who are not vaccinated may become infected with VAPP. It is transmitted through food or household contact.
After the OPV procedure, the virus exists in the child’s intestines for about two months. That is why parents are warned that if their child has just been vaccinated, he is prohibited from attending kindergartens during the above-mentioned period.
It is worth noting that the inactivated version of the vaccine cannot lead to infection. For this reason, some parents choose it.
Remember that viral shedding in children is extremely low, and during transmission, the volume of pathogenic particles decreases several times.
This means that if a child contracts vaccine-associated polio, this is not a reason to panic. As a rule, this infection passes in a mild form, without causing complications.
And yet, can a child infect others after being vaccinated against polio? Such cases are very rare and almost never observed in life. This is why it is important to understand the need for immunization. This is the only way to be sure that the virus will not affect anyone.
Vaccines
There are two types of vaccines to prevent polio—live oral polio vaccine (OPV) and inactivated polio vaccine (IPV). OPV provides essential protection for children against polio. If used repeatedly, it protects the child for life. All available evidence indicates that OPV is not teratogenic and is safe for pregnant women and HIV-infected individuals. However, rare serious adverse events associated with OPV may include vaccine-associated paralytic polio (VAPP) among vaccinated individuals and their contacts, and the emergence of vaccine-derived polioviruses (VDPV). The incidence of VAPP is estimated to be 2–4 cases per million births per year in countries using OPV. The introduction of at least one dose of IPV before OPV vaccination leads to the elimination of VAPP. Let us remind you that in the National Calendar of Preventive Vaccinations of the Russian Federation, the first two (!) vaccinations against polio are given with inactivated polio vaccine!
IPV is considered a highly safe vaccine whether given alone or in combination with other vaccines. There is no evidence of a cause-and-effect relationship with adverse events other than mild local erythema (0.5-1%), tissue induration (3-11%), and tenderness (14-29%).
More about vaccines
Poliomyelitis in adults. Prevention
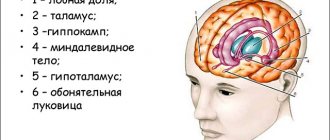
An acute infectious disease caused by a virus of the same name, characterized by damage to the central nervous system, primarily to the cells of the anterior horns of the spinal cord responsible for motor activity, the membranes of the brain and spinal cord. It is observed more often in children and leads to the development of paralysis.
- Diagnosis of polio in children
- Features of polio in adults
- At what age is polio vaccination given to children?
- Fever after polio vaccination
Polio
One of the childhood infections that is very dangerous and leaves behind severe complications is polio. It mainly affects preschoolers, but older children and adults can also suffer from it. You can protect yourself and your children from polio by getting vaccinated against this disease, which begins in the first year of life. How does polio progress in children? Is the polio vaccine really necessary? Is there another way to prevent polio? What are the consequences and complications of polio?
What is polio
Poliomyelitis is a viral infection in which the tissue of the nervous system is involved in the inflammatory process. The nervous system is affected by a type of flaccid paralysis. In addition to neurological signs, symptoms of intoxication are noted. The vast majority of cases of polio occur in children.
Poliomyelitis virus is the causative agent of the disease
The polio virus is the culprit of this serious disease. It's called poliovirus. There are three types of pathogen (poliovirus). The polio virus belongs to a subgroup of enteroviruses. It contains ribonucleic acid (RNA). The polio virus is unstable if it is heated or treated with disinfectants. In addition, antibiotics do not affect it.
Routes of infection with polio
You can become infected with the polio virus from a sick person or a virus carrier. The pathogen enters the environment with the patient’s feces; this process continues for several weeks. The virus can be detected in mucus from the nasopharynx for no more than two weeks. The first five days the patient is considered especially contagious to others. The virus is transmitted in two ways: fecal-oral and airborne, with the first route being the leading one.
The primary reproduction of the virus occurs in the digestive tract, namely on its mucous membrane. In addition, the virus multiplies in the mucous membrane of the nasopharynx. The pathogen then spreads throughout the body through the bloodstream. If it overcomes the barrier with the central nervous system, a paralytic or meningeal form of the disease will occur.
Classification of polio
Like most infectious diseases, polio has its own classification. The infectious process can be of varying degrees of severity (from mild to severe), occurring in typical and atypical forms. The severity of the disease is determined based on the severity of symptoms of intoxication, as well as the nature of motor disorders.
Sometimes the disease proceeds smoothly, but in some cases complications arise and other infections occur.
Prevention of polio
Vaccination against polio is the best way to prevent the disease. Yes, it happens that a vaccinated child gets sick with polio, but in this case the disease is mild, with minor symptoms of intoxication.
Among their neurological symptoms, muscle spasms predominate. Mild paralysis of the leg muscles also occurs in vaccinated people who are sick with polio; they are manifested by limping and muscle weakness. However, these symptoms quickly disappear, and muscle hypotonia persists for a longer time. Persistent complications of polio are not typical for vaccinated children.
Non-specific methods of prevention include maintaining personal hygiene, washing hands after visiting the toilet and before eating, limiting contact with the sick.
Measures at the source of infection
As soon as a doctor or paramedic identifies a patient with polio, he must send an emergency notification to the Center for Hygiene and Epidemiology. The sick person himself is isolated for a period of 3 weeks to 40 days. After the patient is hospitalized, the outbreak is disinfected.
All exposed children under 7 years of age are given emergency immunization. Is it possible to urgently vaccinate against polio for those children who have previously been vaccinated against this infection? It must be done only once. This does not depend on how the child was vaccinated previously. However, at least 6 weeks must pass from the last vaccination.
If emergency vaccination is the first against polio, then subsequent vaccinations are carried out at the necessary intervals.
Poliomyelitis in children
Poliomyelitis in children occurs in various forms. It is not always possible to make a diagnosis, as the signs may be nonspecific. Parents may not even know that their child has suffered from polio. However, there are very severe forms of the disease, with classic neurological symptoms, according to which an experienced doctor will definitely suspect infection with the polio virus.
The latent (incubation) period of infection lasts from 5 days to 5 weeks. On average it lasts about two weeks. With the disease “poliomyelitis,” the symptoms depend on the form of infection, of which there are several.
- Inapparent form of infection
In other words, this form of infection can be called healthy virus carriage. Such a diagnosis can only be made in a laboratory. This form of the disease is rather of scientific interest, since the carrier of the virus himself does not complain about anything and is not dangerous to others. The virus remains in the intestine and does not go beyond it.
- Abortive form of the disease
It is very difficult to suspect polio in this form, since there are no typical symptoms of the disease; the entire infection is hidden under the guise of an acute respiratory disease (ARI). The child develops a slight increase in temperature, weakness, loss of appetite, cough, runny nose, discomfort in the throat, and intestinal disorders. There are no neurological symptoms of polio. The child gradually recovers on his own and requires only simple symptomatic treatment.
- Non-paralytic poliomyelitis (meningeal form)
The disease occurs in the form of serous meningitis. Characterized by an acute onset of the disease, in which the child becomes ill very quickly. He is bothered by headaches, high fever, and frequent vomiting. During the examination, the doctor or paramedic notes positive meningeal symptoms in the patient, which is one of the criteria that the child has inflammation of the membranes of the brain.
With this form of the disease “poliomyelitis” the symptoms are vivid, there are signs of involvement of the nervous system in the process. I am concerned about pain along the nerve trunks. It is difficult for a sick child, he refuses to eat, lies down almost all the time, sleeps, and often cries. Muscle twitching may be observed. This is typical for the first days of illness. There may be some eye symptoms. Paralysis does not occur with this form of polio in children. The child makes a full recovery.
- Paralytic polio
The symptoms of polio in this form of the disease are even more striking; they change in different periods of the disease. In total, it is customary to distinguish four periods of paralytic poliomyelitis.
The preparalytic period of the disease lasts from one to six days. The disease begins with pronounced symptoms of intoxication and high temperature. Sometimes signs of digestive tract disorder appear in the form of constipation or diarrhea. A number of sick children have catarrhal symptoms (sore throat, runny nose, cough).
After a couple of days, the child develops neurological symptoms: pain in the back, arms, legs is noted, sensitivity to various irritants increases, and symptoms of irritation of the meninges become positive. Because of such unpleasant sensations, the sick person tries to lie still.
The paralytic period lasts from a couple of hours to two weeks. Its symptoms vary depending on the specific location of the nervous system lesion.
When neurons located in the anterior horns of the spinal cord, which are responsible for movement, are damaged, a spinal infection develops. Within a week from the onset of the disease, the child develops paralysis. They appear suddenly and develop very quickly. The nature of the paralysis is flaccid, muscle atrophy is present. Sensitivity does not change. It is characteristic that the proximal parts of the extremities (shoulder, thigh) suffer more.
With polio in children, it is not just the limbs that are affected. The intercostal muscles and diaphragm are often involved in the process. In this case, signs of respiratory failure appear.
There is another form of the disease - bulbar. The child has a very pronounced intoxication syndrome, headache and vomiting. Neurological disorders appear very quickly: the child cannot swallow normally, chokes, thin food gets into the nose, the tone of the voice changes (hoarse, hoarse). Since the baby cannot swallow food and saliva normally, his breathing appears bubbling. In some cases, the disease goes so far that the vasomotor and respiratory centers are damaged, paralysis of the diaphragm occurs, which can lead to the death of the baby.
The third form of infection is called pontine. In this case, the bridge in the brain and the nuclei of the cranial nerves, which are located there, are damaged. When the facial nerve is damaged, paralysis of the facial muscles is observed, which is manifested by facial asymmetry, different sizes of palpebral fissures and other signs.
The recovery period for polio in children lasts a long time, from one to three years. The disease makes itself felt for a long time, namely: muscle tone remains reduced for a long time, reflexes from the limbs are not evoked, muscles remain atrophied. Muscle functions are restored gradually and unevenly. Because of this, the consequences of polio include various deformities of the limbs, stiffness (contractures), retarded growth of the affected limb, and lameness.
During the period of residual effects of the disease “poliomyelitis”, consequences are visible that remain with a person for life. Such consequences include persistent flaccid paralysis, deformities of the limbs, shortening of the arms or legs, and atrophy of the muscles of the limbs.
Diagnosis of polio in children
Diagnosis of polio in children is based on medical history, examination of the patient and study of his complaints, as well as on the results of additional studies.
Nonspecific methods for diagnosing polio are as follows:
- General blood analysis
In this analysis, there may be no pathological changes or a moderate increase in leukocytes due to neutrophils.
- Lumbar puncture and cerebrospinal fluid examination
One of the additional diagnostic methods is the study of cerebrospinal fluid obtained by lumbar puncture. Pathological changes in the cerebrospinal fluid occur in non-paralytic and paralytic poliomyelitis.
Cerebrospinal fluid flows out under higher pressure, cytosis (cell number) moderately increases due to lymphocytes, glucose does not increase. Protein in the cerebrospinal fluid may increase in the paralytic form of polio.
- Electromyography
This instrumental research method makes it possible to identify lesions localized in the anterior horns of the spinal cord already on the first day after the onset of the first symptoms.
- Nuclear magnetic resonance imaging of the spinal cord
This study is informative after the acute period of the disease, when the patient begins to recover. It can reveal spinal cord atrophy, which depends on the level of damage.
Specific methods for diagnosing polio are aimed at identifying the pathogen itself or antibodies to it. These include the following methods:
- Virological research
For this study, feces and cerebrospinal fluid are collected from the patient. Moreover, a double examination of feces is required for a patient admitted to the hospital. The material is taken for analysis two days in a row.
- Express diagnostics
To quickly diagnose an infection, an immunofluorescent assay (ELISA) is used, which can be used to detect the virus itself in the patient’s stool or cerebrospinal fluid.
- Serological study
This polio test detects antibodies to the polio virus. Blood and cerebrospinal fluid are taken for analysis. The study is carried out repeatedly, since it is necessary to determine the dynamics of the growth of antibodies and determine type-specific antibodies.
Treatment of polio in children
- If a child is suspected of having polio, he is hospitalized in the infectious diseases department. It must be placed in a separate box.
- It is very important to maintain strict bed rest. The child needs peace.
- In the acute period, thermal procedures on the affected limbs are effective. These include hot wrapping, applications with paraffin and ozokerite.
- To relieve severe pain and alleviate the symptoms of intoxication, the use of analgesics and antipyretics is justified.
- As therapy aimed at the causative agent of the disease, recombinant interferons are prescribed (usually in tablets or suppositories).
- Sometimes diuretics are prescribed to relieve intracranial pressure.
- From the third week of illness, drugs are used that improve neuromuscular conduction (prozerin, galantamine).
- During the recovery period, it is very important to carry out therapeutic exercises and massage. Also, a good effect is observed after sanatorium treatment.
Complications of polio in children
An alarming reaction to the diagnosis of polio is completely justified, because parents, as a rule, have heard about the serious consequences of the disease. Abortive and meningeal forms of the disease occur without consequences.
With the disease polio, the consequences and complications remain after the spinal form of the infection. Some disorders resolve over time. Others stay for a long time or for life. The most severe complications arise from deep injuries. The child may be left lame or have permanent paresis or paralysis of the facial nerve and other cranial nerves.
A fatal outcome may occur in the patient if the vital centers of the brain are involved in the process. Aspiration pneumonia often develops against the background of severe respiratory disorders. Complications such as destructive processes in the lungs and atelectasis were also noted.
Poliomyelitis in adults
Poliomyelitis in adults is very rare, since most people are still vaccinated against this serious infection in infancy. Prevention of polio in some countries is so effective that not a single case of the disease has been reported in them for many years.
For those people who are contraindicated from receiving live vaccines, polio prevention is carried out with inactivated vaccines. However, in some cases this infection still occurs in adults.
Features of polio in adults
As a rule, poliovirus infection occurs in adults who suffer from severe immunodeficiency conditions, such as HIV infection (human immunodeficiency virus). A weakened adult is usually infected from a sick child or from a baby who has recently been vaccinated with a live polio vaccine.
The disease occurs with the same symptoms as in children. Sometimes the infection is not recognized, as it occurs under the guise of an acute respiratory infection. In other cases, damage to the nervous system occurs, paralysis and paresis of the limbs, cranial nerves, and diaphragm develop. Diagnosis and treatment of the disease in adults are similar to those in children.
Consequences of polio in adults
In most cases, polio in adults occurs without serious consequences, impaired functions are gradually restored. Persistent neurological impairment remains uncommon. Fatal outcomes in adults also occur, but with timely diagnosis and treatment, they are rare.
Vaccination against polio
According to the vaccination calendar, according to the rules, vaccination against polio begins in the first half of the baby’s life. Polio vaccinations for children are the best way to prevent this terrible disease.
At what age is polio vaccination given to children?
Children are vaccinated against polio according to the calendar in the first year of life. Following the calendar, the polio vaccine is given first at 3 months, then two more times with an interval of 6 weeks. Sometimes the immunization schedule is disrupted. But in any case, it is important to observe the time interval between vaccine administrations; it should be at least 6 weeks (between the first three).
Many parents are afraid to violate the vaccination schedule and ask the question: “Is it possible to be vaccinated against polio if the child has slight catarrhal symptoms (mild cough, runny nose)?” No, a child can be vaccinated no earlier than 2-4 weeks after recovery. This rule is especially strict when a child is given a live vaccine. The fact that vaccination is carried out not with injections, but with drops, does not reduce the possibility of adverse reactions and complications. Although some parents mistakenly consider drops to be an “easy” method of vaccination.
When is revaccination against polio carried out?
Revaccination against polio is done three times. Children in the second year of life are revaccinated against polio twice (at one and a half years and at 20 months), and the final time at 14 years. Revaccination against polio is carried out with live vaccines if the child has no contraindications to this.
What are the polio vaccines?
Polio vaccines are available live and inactivated (killed). Different countries have different polio vaccination schemes in terms of the choice of live or inactivated vaccine. For a short time, only live polio vaccine was used. Currently, our country has adopted a combined scheme for vaccinating children against polio. That is, children are vaccinated against polio with both inactivated and live vaccines.
Live polio vaccine (drops)
If a child is vaccinated against polio infection, which live vaccines can be given?
OPV is a vaccine whose name stands for “oral polio vaccine.” Oral means given to the child through the mouth. By the way, this is the only vaccination that is given to children in this way. This vaccine is produced in our country.
The imported live polio vaccine, which is also used in our country, is called Polio Sabin Vero. It is used in exactly the same way as OPV.
What are polio drops? Polio drops is the colloquial name for live polio vaccine.
When vaccinated against polio, drops are given to a child as follows: one hour before meals, the nurse puts drops into the mouth (four drops when using OPV and 2 drops when using Polio Sabin Vero). This can be done using a pipette, a special dropper or a syringe. You should not drink any liquid after administering the drops. The baby does not feed for an hour after vaccination.
If during vaccination against polio drops the baby burps or vomits, then you must immediately give him a second dose of the polio vaccine. If regurgitation occurs again, a new dose is given only at the next vaccination visit.
The live polio vaccine is given once in the first year of life (third vaccination). Then all revaccinations against polio are carried out with a live vaccine. Often, parents choose imported combination vaccines against several diseases at once, in which protection against poliovirus is presented in an inactivated form. In this case, the child receives all three first vaccinations with an inactivated vaccine, and the live one is administered only during revaccination. This is not a violation of the rules for vaccinating children.
Conducted studies prove that even a single vaccination with a live vaccine forms immunity against poliovirus infection in more than 90% of those vaccinated. But repeated vaccination is justified, since polio is caused by three different viruses, and a single vaccination does not always protect against three viruses at once.
Inactivated polio vaccine
In our country, it is currently customary to give the first two vaccinations against polio with inactivated vaccines, followed by a live vaccine. Until recently, there was a scheme when all three vaccinations were given with inactivated vaccines in the first year of life. It is worth noting that many parents still adhere to this old vaccination schedule for their children.
Some children have contraindications for vaccination with live vaccines. These children are vaccinated against a disease such as polio only with killed vaccines.
A primary course of immunization with an inactivated vaccine provides good protection against poliovirus infection in more than 96% of vaccinated individuals. In a number of countries where no cases of polio have been reported for many years, vaccinations are given only with inactivated vaccines.
There are mono vaccines for the prevention of polio, that is, they protect only against this disease. And there are also combination drugs. An example of a monovaccine is Imovax Polio.
Can the polio vaccine be given with other vaccinations?
Modern parents are often afraid to combine the administration of several vaccines in one day. Is it possible to vaccinate children against polio on the same day as other vaccinations?
If a child is vaccinated according to the calendar and does not have an individual vaccination schedule, then on the same day he is vaccinated against the following diseases: whooping cough, tetanus, diphtheria and polio.
In some cases, a child is given either 2-3 vaccinations at once, or a combined vaccine is simply given. For example, there are vaccines called “Tetracok”, “Infanrix IPV”, which contain components against protection against the following infections: whooping cough, tetanus, diphtheria, polio.
Recently, vaccination against hemophilus influenzae infection has appeared on the schedule; it is also done on the same day. Vaccines have been developed that contain protection against all of these diseases: whooping cough, tetanus, diphtheria, polio and Haemophilus influenzae. An example of such a vaccine is the drug Pentaxim.
In the first year of life, the baby is vaccinated against hepatitis B three times. If you follow the calendar, the third vaccination against hepatitis B (at 6 months) coincides with the last vaccination against diseases such as tetanus, whooping cough, diphtheria and polio.
If the immunization schedule is disrupted, vaccination against hepatitis B may coincide with other administrations of vaccines against the above diseases, that is, not only at the age of six months.
It is possible to use a monovaccine against hepatitis B, while giving an additional injection to the child. Another, more gentle method of vaccination is possible. For this purpose, vaccines are used that protect against several diseases, as well as hepatitis B.
The Infanrix Penta vaccine protects the child against the following infections: whooping cough, diphtheria, tetanus, hepatitis B and polio. The Infanrix Hexa vaccine provides protection against six diseases: whooping cough, diphtheria, tetanus, Haemophilus influenzae, hepatitis B and polio.
The Hexavak vaccine contains immune components against the following diseases: whooping cough, tetanus, diphtheria, Haemophilus influenzae, hepatitis B and polio.
Sometimes hepatitis B vaccinations are started or continued in the second year of life for various reasons. Some immunizations may coincide with polio vaccinations. Therefore, the following combination of vaccines against hepatitis B and polio is quite realistic: hepatitis monovaccine + OPV, as well as other combinations.
Is it possible to be vaccinated against polio with a live vaccine in combination with other vaccines that are not listed above? Yes, live polio vaccine is compatible with other vaccines except BCG.
Is it possible to send a child who has not been vaccinated against polio to kindergarten?
Not all parents vaccinate their children. Some people do not get vaccinated because they have contraindications. Some people unreasonably refuse vaccinations, considering them harmful and dangerous. Unvaccinated children often have difficulty visiting childcare facilities. It is impossible not to take them to kindergarten; after all, vaccinations are voluntary.
However, a child who has not been vaccinated against polio will be temporarily suspended from visiting a child care facility if there is a child in his group who has recently been vaccinated against this disease with a live vaccine.
Reaction to polio vaccine
A person may have adverse reactions and complications with any vaccination. If the baby is vaccinated against polio, the vaccination can cause complications and cause normal post-vaccination reactions. It is important to distinguish them from each other.
To prevent the reaction to vaccination against polio from being very pronounced, it is important to approach the issue of vaccination competently and carefully question and examine the patient. It is important to find out if he is allergic to those substances that are part of the vaccines, and also to see if he is currently suffering from acute illnesses.
Fever after polio vaccination
Can the temperature rise after polio vaccination? An increase in temperature after vaccination against polio with live vaccine is not typical.
When using inactivated polio vaccine, fever after vaccination is relatively common. This is usually noted in the first two days after administration of the drug.
Fever is most often observed with combination vaccines, but they also contain components against other infections. In particular, the pertussis component is one of the most reactogenic, so the severity of the reactions may be associated with it.
Sometimes the temperature rises after a polio vaccination, but it is not related to the vaccination, but is only a signal that the child has become infected with some other concomitant infection, in other words, has become ill.
Other possible normal reactions to vaccination
What are some normal reactions to the polio vaccine, other than fever? There is practically no response to the introduction of live polio vaccine in babies and older children.
When a child is given a combination vaccine or an inactivated monovaccine against polio, the body's reaction varies. A normal reaction may be mild intoxication (headache, loss of appetite, sleep disturbance), slight compaction at the injection site and redness (no more than 8 cm in diameter), as well as slight pain.
Complications of the polio vaccine
If a child is vaccinated against polio, can the vaccination cause complications?
What complications occur with the polio vaccine?
It is possible to develop local complications following vaccination: a purulent inflammatory process at the site of drug administration, purulent inflammation of the lymph nodes, induration and redness greater than 8 cm in diameter.
Allergic reactions to the polio vaccine are its complications. They manifest themselves as various swellings and rashes. A severe reaction is the development of anaphylactic shock to the administration of the drug. Allergic complications occur in the first days after immunization. Typically, allergies occur to vaccine excipients, which can be chicken protein, streptomycin, neomycin and others.
A very serious complication of polio vaccination is the development of vaccine-associated polio. This complication occurs in one out of 1.5-2 million vaccinated children. Children who have not been vaccinated against polio can also get sick if they have been in contact with a child who has been vaccinated with a live vaccine against this disease. These children are called contacts of children vaccinated with live polio vaccine.
Vaccine-associated polio is a neurological complication that is manifested by the development of acute flaccid paralysis in the baby. At the same time, he retains sensitivity. After the illness, the child has lifelong immunity.
The development of this complication begins from 4 to 30 days after vaccination in the child who was vaccinated, and up to 60 days after vaccination, a child who has not been vaccinated against polio (that is, a contact) may become ill. Therefore, children who have not been vaccinated against polio should not come into contact with those children who have been vaccinated against this infection for 8-9 weeks.
Historical information and interesting facts
Expert opinion
CM. Harit
Professor, Doctor of Medical Sciences, Head of the Department of Prevention of Infectious Diseases of the Research Institute of Children's Infections
In Europe and the USA and Japan and Australia and other countries, vaccinations are given with a killed polio vaccine, in our country the child receives the first 2 vaccinations with the same killed vaccine and only the subsequent ones with a live one...
Scientific research on polio dates back to the work of the German orthopedist J. Heine (1840), the Russian neurologist A. Ya. Kozhevnikov (1883) and the Swedish pediatrician O. Medina (1890), who showed the independence and contagiousness of this disease.
Iron Lung apparatus, circa 1950
Before the polio vaccine was invented, patients were placed in an iron lung machine that stimulated breathing. It was he who served as the prototype of modern anesthesia machines and devices for artificial ventilation of the lungs.
On April 112, 1955, a large-scale study was successfully completed in the United States, confirming the effectiveness of the Jonas Salk vaccine, the first vaccine against polio. The importance of this event cannot be overestimated. In 1954, more than 38 thousand cases of polio were reported in the United States, and after 10 years of the use of the Salk vaccine, in 1965, the number of cases of polio in the United States was only 61.
All over the world, attenuated (weakened) strains obtained by Dr. Sabin - serotypes 1, 2 and 3 - are used for the production of live polio vaccines.
3 serotypes. No indigenous wild poliovirus type 2 has been detected in the world since 1999. 26-31% of VAPP cases are associated with vaccine virus 2, which is a component of trivalent OPV. It has therefore become critical to move from the use of trivalent OPV (containing virus serotypes 1,2 and 3) to bivalent OPV (containing only serotypes 1 and 3) in national immunization programs and to coordinate this transition internationally. In 2015, the World Health Assembly agreed that all WHO Member States currently using OPV should prepare for a global phaseout of the type 2 poliovirus component of OPV. In April 2021, all stocks of trivalent OPV were seized and destroyed from all service delivery points, and their seizure was confirmed by WHO.
How the disease is treated in Moscow
Treatment of polio is carried out in an infectious diseases hospital and involves an integrated approach, including:
- strict bed rest. The patient should remain calm, in a favorable environment;
- protection of paralyzed muscles. For this purpose, special splints can be applied;
- physiotherapy. This includes physical therapy, swimming in the pool under the supervision of a trainer, and massage. This also includes electrical stimulation, paraffin applications, UHF therapy and much more. The procedures are aimed at stabilizing the nervous system, helping paralyzed muscles;
- Ventilation Clinical guidelines for polio also suggest major life-sustaining interventions. The use of a mechanical ventilation device is indicated for patients whose paralysis has affected the respiratory system, and therefore threatens respiratory arrest;
- use of special medications.
It is very important that a polio patient be closely monitored, especially when the disease is progressing or not showing significant improvement.